The term “kidney inflammation” is widely used to define pathological phenomena that occur in acute or chronic form and affect individual segments of the kidneys. This pathology can be equally diagnosed in men and women, regardless of age category. The main factors provoking the occurrence of pathological processes are pathogenic microorganisms that inhabit the natural microflora of the human body. The inflammatory process in the kidneys must be treated at the first manifestations, otherwise there is a high probability of developing various kinds of complications.
Types and causes of jade
Nephritis is a large group of diseases that have different etiologies (origins) and course patterns. Diseases of the kidneys and urinary tract can be infectious or autoimmune.
The infectious process is usually one-sided: inflammation is localized only in the right or left kidney.
Inflammation of the pelvis is called pyelonephritis. Autoimmune diseases affect two kidneys at once. For example, lupus nephritis with systemic lupus erythematosus or glomerulonephritis.
Pyelonephritis
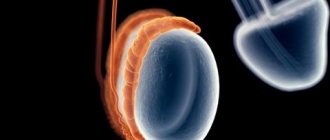
With pyelonephritis, the renal pelvis (bowls) becomes inflamed. The name comes from the Latin word “pielos” - renal pelvis. It is usually caused by bacteria, most commonly Escherichia coli (E. coli). Inflammation can be acute or chronic.
Pyelonephritis is one of the most common urological diseases. Mostly women suffer from it.
Factors that increase the risk of developing pyelonephritis:
- childhood;
- female;
- active sex life;
- pregnancy and childbirth;
- prostate hyperplasia in men;
- urolithiasis disease;
- neoplasms that obstruct the flow of urine;
- diabetes;
- decreased immunity;
- abnormal development of the urinary system.
Often inflammation of the pelvis appears after hypothermia. Another reason is cystitis. If treated incorrectly, bacteria can “rise” into the pelvis and cause inflammation in them.
Glomerulonephritis
Glomerulonephritis affects the glomeruli (glomeruli). The glomerulus is the functional, working unit of the kidney. Damage to it leads to organ failure.
The inflammatory process in the kidneys with glomerulonephritis is of an autoimmune nature. This means that the body destroys itself. The main cause of glomerular nephritis is group A beta-hemolytic streptococcus. This bacterium stimulates the body to produce autoantibodies that destroy its own glomeruli. Therefore, autoimmune inflammation is usually preceded by a bacterial infection of a completely different localization.
What causes glomerulonephritis:
- pneumonia;
- tonsillitis;
- erysipelas of the skin;
- scarlet fever.
You can also get glomerulonephritis after ARVI, chickenpox, or measles.
General hypothermia does not cause this disease, but it increases the risk of getting sick.
Autoimmune inflammation can be acute or chronic. It can also occur in a typical (violent) form or be erased.
Interstitial nephritis
Tubulointerstitial nephritis (TIN) is inflammation of the renal tubules not associated with infection. The disease is also immunological in nature. It is characterized by a malignant course, that is, it leads to serious consequences (renal failure).
With tubulointerstitial nephritis, the connective tissue of the kidneys and the renal vessels are affected.
Reasons for TIN:
- Use of nephrotoxic substances and medications. More than half of all cases of TIN are associated with the use of antibacterial drugs and painkillers (NSAIDs). In addition, tubulointerstitial nephritis is caused by taking thiazide diuretics (hydrochlorithiazide), barbituric acid derivatives (Corvalol, Barboval), as well as immunosuppressants.
- Systemic diseases. TIN may be part of systemic connective tissue inflammation in sarcoidosis, systemic lupus erythematosus, Sjögren's syndrome, etc. Sometimes interstitial nephritis complicates the course of lymphoma.
- Infectious diseases. Tubulointerstitial nephritis is caused by pathogens of brucellosis, plague, mononucleosis, typhus and other dangerous infections.
- Unknown reasons. Sometimes it is impossible to determine the origin of a TIN.
Interstitial inflammation progresses rapidly and often leads to severe renal failure.
Classification of inflammatory kidney diseases by course
Nephritis can occur in acute or chronic form. Not only the treatment, but also the prognosis of the disease depends on the form of renal inflammation. Chronic damage cannot be cured, but acute kidney inflammation can be treated. The exception is severe and malignant forms of acute nephritis.
For example, acute glomerulonephritis does not require treatment at all. It may go away on its own. At the same time, chronic glomerulonephritis constantly progresses and leads to complete kidney failure.
Treatment of pyelonephritis
consists primarily in eliminating its cause - the underlying disease (urolithiasis, ureteral strictures, prostate adenoma, etc.). In addition, adequate antimicrobial therapy is necessary, selected on the basis of urine culture and determination of the sensitivity of bacteria to antibiotics. There are a number of additional treatments for kidney inflammation.
What's important? The patient must understand that chronic pyelonephritis is a “gentle killer” of the kidneys. And if you don’t fight it, it will probably lead you to the hemodialysis department. Modern methods of treating kidney inflammation make it possible to effectively prevent the development of this disease.
Symptoms of kidney inflammation
Signs of kidney inflammation vary. The same disease can occur in different ways. Sometimes people suffer from nephritis in an asymptomatic form. The clinical picture also depends on the nature of the inflammation.
Typical renal syndromes:
- Uric. This symptom complex is characterized by a decrease in the amount of urine, hematuria (blood in the urine), leukocyturia (white blood cells in the urine) and other laboratory changes. There are no systemic signs of inflammation or other symptoms.
- Nephrotic syndrome includes proteinuria (loss of more than 3.5 g of protein per day in the urine), hypoproteinemia (low total protein in the blood), dyslipidemia (increased cholesterol in the blood) and edema.
- Nephritic syndrome is also characterized by proteinuria (loss of less than 3.5 g per day) and hematuria. Additionally, blood pressure increases.
All these syndromes are characteristic of different nephritis.
The following symptoms are also characteristic of inflammation:
- fever;
- chills;
- pale skin;
- urine the color of meat slop or other unnatural shade;
- increased frequency of trips to the toilet, pain and pain when urinating;
- rash all over the body;
- pain in the lumbar region.
In children, fever is more pronounced, in adults - pain syndrome.
What symptomatic characteristics of the disease are observed in children?
Inflammation of the kidneys in a child is expressed by incontinence or, conversely, lack of bowel movements. The process of urination is painful, which brings the baby to tears. The temperature is elevated, there is pain in the lower abdomen and lower back. The urine has darkened and there are flakes of other specific impurities in it. In combination, all the symptoms of kidney inflammation in children cause vomiting.
If parents notice at least one such sign of pathology, it is necessary to immediately show the child to a qualified physician.
Diagnostics
To diagnose nephritis, laboratory and instrumental studies are carried out.
How to determine kidney inflammation:
- general urinalysis with microscopy;
- urine tests according to Zimnitsky and Nechiporenko;
- daily microalbuminuria;
- general blood analysis;
- biochemical blood test and rheumatic tests;
- Ultrasound of the kidneys;
- Doppler examination of renal vessels;
- radioisotope research.
The only method that can confirm glomerulonephritis or TIN is a kidney biopsy. However, due to the high risk of complications and low availability, it is rarely performed.
The diagnosis is made based on a set of collected data: anamnesis, laboratory and hardware tests.
How to treat kidney inflammation with drugs
Treatment for nephritis depends on its type and shape. The most important thing is to start quality therapy in a timely manner. The further prognosis of recovery and even life depends on this factor.
Antibiotics
Antibacterial agents are prescribed for infectious inflammation of the kidneys. These are the main drugs in the treatment of pyelonephritis.
How to treat kidney inflammation caused by bacteria:
- Cephalosporins: Ceftriaxone (analogs - Emsef, Rotacef, Medaxone), Cefpodoxime (Foxero, Cefma, Cefodox), Ceftibuten (Cedex).
- Fluoroquinolones: Ciprofloxacin (Flaprox, Tsiprinol, Tsiprolet), Levofloxacin (Levoximed, Tigeron, Levaxela).
- Protected penicillins: amoxicillin with clavulanic acid (Augmentin).
- Aminoglycosides: Gentamicin (Gentamicin-Sandoz, Chitosan-Genta).
The course of antibiotic therapy is selected by the doctor. Usually the duration is 5-10 days for uncomplicated pyelonephritis, several weeks for complicated ones.
Uroantiseptics
To better cleanse the pelvis of bacteria, uroantiseptics are prescribed in combination with antibiotics.
Uroseptics for cleansing the kidneys of pathogenic microorganisms:
- quinolone series: Palin, Urosept;
- nitrofurans: Furamag, Urofuragin, Furadonin.
A number of herbal uroantiseptics also help well: Canephron N, Trinephron, Urolesan.
Antispasmodics and painkillers
Infectious inflammation in the kidneys is usually accompanied by severe pain.
Since analgesics are contraindicated due to their high nephrotoxicity, antispasmodics are prescribed.
Platiphylline, Papaverine, and Drotaverine (No-Shpa) help well. They relieve spasm of smooth muscles, relieve pain and improve urine flow.
Preparations for dissolving stones
Not all stones can be dissolved with medications. Therefore, the need for their appointment is determined by a urologist/nephrologist.
Medicines to dissolve kidney stones:
- Allopurinol;
- potassium citrate;
- Blémarin;
- Xydiphone;
- Spilled;
- Cholestyramine;
- Tiopronin;
- Uralit-U.
To cure urolithiasis with medications, you need to decide on the type of stones. Oxalates and urates respond best to conservative therapy.
Other medicines
For glomerulonephritis, glucocorticosteroids (Prednisolone) are prescribed. These medications relieve autoimmune inflammation in the glomeruli. Cytostatics (Cyclophosphamide) are also used.
If intoxication is severe, infusion therapy is performed (droppers with glucose, Ringer's solution). For high renal pressure, ACE inhibitors (Lisinopril, Perindopril, Enalapril) are prescribed.
Therapeutic measures
Inflammation of the adrenal glands and kidneys should be treated only in a hospital setting. The main treatment method is drug therapy. The patient is prescribed the following medications:
- antibacterial. These pharmaceuticals may be prescribed as tablets or injections. They are prescribed with caution during pregnancy;
- antihistamines;
- diuretics;
- glucocorticosteroids;
- calcium supplements (usually in tablet form);
- immunostimulants;
- cytostatics (prescribed during pregnancy in extremely difficult situations);
- vitamins;
- antihypertensive drugs;
- drugs that normalize blood circulation in the kidneys.
If the prescription of tablets and injections does not bring the desired result, then the treatment plan includes hemosorption and plasmapheresis. If the treatment was chosen correctly, the patient’s condition will gradually begin to improve within a week.
Diet and drinking regime
For uncomplicated kidney diseases, drink plenty of alkaline fluids. For inflammation, you need to drink a decoction of dried fruits, green tea, mineral waters (Essentuki, Borjomi, Polyana Kvasova). If renal filtration is impaired, be sure to control the volume of fluid drunk and excreted to avoid edema.
Diet is an important part of kidney treatment. Therefore, it is prescribed simultaneously with the main drug course.
What can you eat if you have kidney inflammation?
- vegetables;
- fruits;
- cereals;
- berries;
- bread;
- vegetable oils;
- dairy products.
It is forbidden to consume table salt, animal protein (meat, eggs), fatty foods, and canned food.
Possible complications
If the kidneys are not treated in a timely manner, complications may arise associated with the spread of E. coli to nearby organs (uterus, vagina, bladder, adrenal glands, large intestine), which leads to purulent inflammation, new diseases, and chronic forms.
If the symptoms are ignored, acute renal failure, paranephritis, hypertension, water metabolism disorders, carbuncle, kidney abscess, and possible death may develop. Kidney disease can affect fetal development during pregnancy due to the spread of pathogenic microorganisms.
How to relieve kidney inflammation at home
Traditional methods of treatment should be used in combination with the main therapy and only in consultation with the attending physician. Herbal medicine has shown good effectiveness in the treatment of urological diseases.
How to relieve inflammation in the kidneys quickly and effectively using folk remedies:
- Infusion of birch buds. Pour a glass of boiling water over a handful of birch buds. Leave for 1 hour. Strain and cool. Drink a third of a glass 3 times a day 20 minutes before meals. The course of treatment is 10 days.
- Juniper berry tincture. 100 g of fresh or dried juniper berries pour 0.5 liters of vodka. Leave for 7 days in a cool, dark place. Take 1 tsp. tincture, previously diluted in a glass of warm mineral water. The course of treatment is 10-14 days.
- Lime tea. It is best to prepare tea in a thermos for the whole day. Add 1 liter of boiling water to two handfuls of linden. Leave for half an hour. Then strain and pour into a thermos. Drink 1 glass hot 3 times a day instead of tea.
- The infusion is half-burnt. 1 tbsp. herbs for 1 cup of boiling water. Leave for 15-20 minutes. Strain and cool. Drink a third of a glass 3 times a day 1 hour before meals through a straw.
Herbal phytoncides relieve inflammation well and also kill pathogenic microorganisms in the kidneys.
Diseases of other organs with pain in the renal area
Pain in the area of the kidney organ can also occur with diseases of other organs. Pain in the lower back is caused by lumbar osteochondrosis. The pain radiates to the leg. Muscle weakness, tingling and numbness of the limbs are observed.
Severe and acute pain occurs when there is a hernia in the spine. Such symptoms occur with injuries to the spine, ribs, spinal cord, liver and spleen. In this case, the symptoms are mixed, and the diagnosis is established after a thorough examination of the patient.
Pain in the kidney area occurs with acute appendicitis and is accompanied by a number of negative symptoms. Pain occurs at the location of the kidneys due to prostate pathology. Here there is a disturbance in the outflow of urine, problems with potency arise, and the pain radiates to the perineum.