Epididymitis is an inflammation of the epididymis. In most cases, it is infectious in nature and only in rare cases has a cause unrelated to infection. Epididymitis is one of the most common pathologies of the reproductive system in men. It usually occurs in patients 20-50 years old: it is in this age range that the highest sexual activity is observed. However, the disease occurs in children, adolescents, and older men.
Epididymitis is accompanied by severe pain and significantly reduces the patient's quality of life. It can also become chronic and lead to infertility and other serious complications, so its symptoms cannot be ignored.
Classification of epididymitis
Epididymitis is classified according to its origin, prevalence of the pathological process and form.
By origin, epididymitis in men can be infectious or non-infectious. It can be caused by bacterial, viral and fungal infections.
Most often, epididymitis is caused by bacteria. In men under 40 years of age, the disease in most cases develops due to gonococcus, chlamydia, and other sexually transmitted microorganisms. In older men - due to urinary tract infections (pathogens enter the epididymis from nearby organs of the urinary system).
Reference! Epididymitis can occur as a complication of a number of infectious viral, bacterial or fungal diseases: sore throat, mumps, influenza, pneumonia, etc. The pathogens enter the epididymis through the bloodstream. Epididymitis can also develop against the background of systemic infections: tuberculosis, cryptococcosis and brucellosis.
Non-infectious epididymitis is quite rare. It may occur due to:
- Scrotal injuries.
- Chemical irritation of the epididymis (when taking certain medications or throwing urine into the epididymis).
According to the prevalence of the pathological process, the disease is:
- Unilateral (develops on the epididymis of only one testicle, most often on the left side - due to anatomical features, the left duct is more elongated);
- Bilateral (inflammation affects both appendages).
According to the nature of the course, epididymitis occurs:
- Acute - develops sharply, violently. The symptoms are pronounced. Most often it affects one side and lasts from 7 to 10 days.
- Subacute - characterized by a not as rapid onset as acute, it develops slowly. Symptoms are less pronounced. The pathological process lasts longer than in the acute form.
- Chronic - is a consequence of an untreated acute or subacute disease. It is characterized by alternating periods of exacerbations and remissions. The chronic process usually extends to both testicles. If left untreated, this form of the disease can lead to the development of infertility and other complications.
Reference! Epididymitis often occurs in parallel with orchitis, an inflammation of the testicle. This is due to the fact that the infection quickly spreads from the testicle to its epididymis and vice versa. Therefore, orchitis is often followed by the development of epididymitis, and epididymitis is often followed by orchitis. The pathological process in which both the testicle and the epididymis are involved is called epididymitis orchioepididymitis.
What is epididymitis?
The testicles are a paired organ located in the scrotum. On the back surface of the testicle there is its appendage - a dense formation that contains a kind of tube, coiled in the form of a spiral. The tube is filled with fluid and nutrients necessary for sperm to mature. Since the epididymis is directly connected to the testicles, when they become inflamed, infection of the testicle often occurs. This disease is called epididymitis orchioepididymitis. This is the most common inflammatory process of the scrotal organs.
The end of the epididymis is connected to the vas deferens, which passes through the prostate gland to the urethra. Therefore, infection from these organs can retrogradely penetrate the appendage. Infection of the latter when microbes enter the bloodstream is rarely recorded.
Every year, one in 1,000 men develops epididymitis. The chronic form of the disease causes long-term pain in the scrotum in 80% of cases.
Description of the pathology
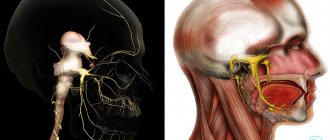
The term epididymis (epididymis) of the testicle in urologists refers to a small spiral-shaped tube located on top of the testicle and on its posterior surface.
The length of the hollow organ is about 6 mm. Its main function is to create conditions under which sperm mature.
Sperm cross the duct in about two weeks, during which time they are completely ready to fertilize the egg.
Inflammation of the epididymis occurs most often due to exposure to infectious agents on the epididymis. But epididymitis can also be of non-infectious origin. Sometimes the inflammatory process spreads to the testicle, in which case they speak of orchiepididymitis.
In most cases, only one appendage becomes inflamed, but sometimes pathological processes begin to occur immediately on both sides (in 10-20% of cases) or the second epididymis becomes inflamed later.
Epididymitis is typical for young men with an active sexual life. Inflammation of the appendage can also occur in a child; as a rule, in this case it is a consequence of a systemic infectious disease or injury.
Causes of the disease
The causative agent of the disease is most often pathogenic bacteria that cause infectious epididymitis. They penetrate retrogradely from the tissues of the urethra, prostate, and vas deferens. This mechanism of development of pathology is observed in 80% of patients.
The main causes of epididymitis: sexually transmitted microorganisms and bacteria that are part of the intestinal microflora. In men under 40 years of age, almost 60% of cases of pathology are caused by chlamydia; gonorrhea, gardnerella, and sometimes treponema are somewhat less common.
In patients over 40 years of age, E. coli is more common. This microorganism often causes a bladder infection, and from there rises into the appendages. The risk of such an infection increases in people of any age who practice anal sex. In some cases, the disease is caused by staphylococci, streptococci and other microbes. In children and men over 40, pathology can be caused by different types of Proteus, Klebsiella, Pseudomonas, Ureaplasma, Corynebacterium and Mycoplasma. Bacteria can enter the tissue of the appendage and through blood vessels (rarely) from other organs, that is, through the hematogenous route.
In children, the cause of inflammation of the appendages can be a viral infection, including mumps, as well as infection with coxsackievirus infection, chickenpox or ECHO viruses.
In persons with immunodeficiencies, epididymitis can be caused by pathogens of coccidioidosis, blastomycosis, cytomegaloviruses, and Candida fungi.
Inflammation caused by retrograde reflux of urine from the prostatic part of the urethra through the vas deferens contributes to damage to the appendages. This happens during physical activity (for example, weightlifting) or sexual intercourse with a full bladder, and is also widespread with prostate adenoma. 56% of men over 60 years of age with epididymitis also have prostatic hyperplasia or urethral stricture.
In this case, urine is thrown into the overlying parts of the genitourinary tract, and pathogenic microorganisms penetrate with it. Therefore, it is important to empty your bladder promptly.
Acute epididymitis orchididymitis occurs in 12-19% of patients with Behçet's syndrome. In addition, the incidence of the disease increases with Henoch-Schönlein syndrome, especially in children. This is probably due to the systemic nature of the inflammatory process in these diseases. Damage to the scrotal organs is present in 38% of patients with Henoch-Schönlein syndrome.
Drug-induced epididymitis is sometimes observed, the most common cause of which is the drug Amiodarone, used for heart rhythm disorders. With this variant of the pathology, the appendages are affected on both sides. The incidence of pathology depends on the dose taken and increases if the patient uses more than 200 mg of Amiodarone per day. At the same time, the body synthesizes antibodies that are directed not only against drug molecules, but also attack the tissues of the appendage, causing lymphoid infiltration and focal tissue fibrosis.
Congestive epididymitis occurs when blood circulation in the pelvic organs is impaired. Its development is facilitated by interrupted sexual intercourse, hemorrhoids, and constant constipation. Lack of blood circulation leads to impaired nutrition of tissues and a decrease in their immune defense. Against this background, a bacterial infection quickly develops.
About 1 in 1,000 men who have a vasectomy (removal of the vas deferens) experience pain in the form of chronic, dull, aching pain in the epididymis and testicle. The pain is caused by secondary retention of sperm and seminal fluid in the epididymis, which continues to be released after the vasectomy. As a result, granulomas and inflammation of the appendage occur.
Factors that increase the likelihood of the disease are trauma and hypothermia, as well as instrumental interventions - urethral dilation, urethroscopy, bladder catheterization, cystoscopy.
In addition, the risk of the disease increases if the patient:
- does not use condoms during sexual intercourse;
- has structural abnormalities in the development of the genitourinary tract;
- suffered from or is sick with tuberculosis or sarcoidosis;
- has prostate hyperplasia or adenoma that blocks the normal flow of urine from the bladder;
- recently had surgery on the urinary organs or groin area.
A procedure such as circumcision of the foreskin reduces the risk of developing urinary infections, and epididymitis in particular.
Sometimes the cause of acute epididymitis cannot be determined, then it is called idiopathic.
The structure of the epididymis (epididymis)
Epididymitis affects the male internal reproductive system. The length of the appendage is no more than 5-8 centimeters, and the width does not exceed 2 centimeters. The epididymis plays an important role in the male body: this is the place where sperm mature and accumulate. They move through the canals of the appendage for about 20 days. The movement is passive and is carried out due to the cilia, which are located inside the channels.
The appendage itself can be divided into three main structural parts: the body, the head and the tail. The head consists of fifteen lobes, which are formed thanks to the efferent canals. The epididymal duct, which connects to the vas deferens, passes through the body of the epididymis and widens at the tail. It is in this place that sperm accumulate.
There are known cases of incorrect primary formation of the genitourinary system or genetic mutations, as a result of which torsions and other pathogenic changes are possible, which cause the development of an acute form of epididymitis.
Classification
There are acute and chronic forms of the disease. These forms differ in symptoms and treatment tactics.
- Acute epididymitis
Caused by nonspecific pathogens, it develops quickly and is accompanied by the appearance of pronounced clinical symptoms, often on one side. Right-sided epididymitis usually occurs. This is due to the peculiarities of the anatomy of the male genital organs.
Often the testicular membrane is involved in the process, and dropsy occurs. With proper treatment, signs of the disease disappear after a week, but compaction in the appendage area can persist for 2 months.
The acute form is serous and purulent. In the first case, swelling and tissue infiltration are characteristic. During the purulent process, individual foci first form, and then the appendage melts on the left or right.
If treatment tactics are incorrect, the disease becomes chronic. The temperature is normal, the appendage is moderately enlarged and compacted, and minor pain in the scrotum is noted. The duration of the disease exceeds 3 months.
- Chronic forms of pathology
May be associated with inflammation, obstruction (obstruction) of the vas deferens. Sometimes there are no external changes, but prolonged pain in the affected organ persists.
There are also specific variants of pathology caused by pathogens of tuberculosis, cryptococcosis, and brucellosis. Syphilitic epididymitis is observed very rarely. Tuberculous epididymitis occurs in patients with pulmonary and other forms of tuberculosis, in particular with damage to the kidneys or bladder. Tuberculosis and other systemic diseases, for example, Behçet's syndrome, lead to rapid chronicization of the acute process.
ICD
A large number of modern classifications have been collected; the main and most significant is ICD 10, acute epididymitis, which is included under a general nosology.
The ICD scheme was to organize all data on diseases, collect a summary description, symptoms, syndromes, signs, factors from the practical medical side. This is what the main and most important classification of diseases looks like. A. The ICD-10 code for epididymitis is encrypted into the international classification of diseases, symptoms, and syndromes under a single standard for the healthcare system around the world.
The document is used as a generally accepted statistical basis. The structure of ICD-10 was developed on the basis of all possible classifications, according to the nature of the course of the disease, according to location, severity, and pathogen. We are interested in a disease of the male genitourinary system, which is described as epididymitis - Acute Epididymitis, code according to ICD-10, or rather, this nosology is included in the landmarks of the male genitourinary system. How exactly to find acute Epididymitis in CodeICD-10. This disease is included in the list of all pathologies of the male reproductive urinary system under number XIV, this class belongs to diseases of the male system, has the serial number N00-N99, to select the diagnosis I need, it is enough to know the clinical signs or symptoms. ICD code acute epididymitis is included in the subgroup of diseases of the male genital organs N40-N51. Diagnosis with code N45
- N45.0 - Orchitis, epididymitis and epididymo-orchitis with abscess;
- N45.9 - Orchitis, epididymitis and epididymo-orchitis without mention of abscess;
The ICD code for acute epididymitis is not allocated separately; it is included in the group N45.0 and N45.9 and is encrypted with these codes.
Clinical signs
Inflammation of the epididymis occurs suddenly and often reaches its maximum severity within 24 hours. First, pain appears in the scrotum or groin. Unpleasant sensations may also occur in the lateral parts of the abdomen above the inguinal fold. This is typical for the primary focus of infection in the vas deferens. Then the microorganisms descend down, entering the appendages.
Other symptoms:
- swelling and pain in the scrotum (often the appendage doubles its normal size in a few hours);
- irradiation of pain to the lower back, groin, iliac region;
- painful urination and blood in the urine;
- mucous or purulent discharge from the urethra, especially in young men;
- redness and increased local temperature of the skin of the scrotum;
- fever and chills, nausea, weakness; the temperature may be low-grade;
- feeling of pressure or fullness in the testicles;
- enlarged lymph nodes in the groin;
- pain during sexual intercourse and ejaculation;
- pain when walking, urinating, or defecating;
- frequent urination;
- premature ejaculation;
- admixture of blood to sperm.
Pain in the scrotum, urinary problems, or any of the above symptoms require a visit to the doctor. There are also situations when medical attention is required immediately.
Severe pain in the scrotum may be a sign of testicular torsion, a very serious condition that requires urgent treatment. The sooner therapy is started, the greater the likelihood of maintaining the viability of the organ.
Signs of necrotizing fasciitis or other inflammatory complications may include:
- discharge from the urethra;
- pain and burning when urinating;
- frequent urination;
- significant fever and chills;
- nausea;
- pain in the lower abdomen;
- hardening or swelling of one of the testicles.
Such signs require immediate consultation with a urologist.
Diagnostic measures
Before deciding how to treat epididymitis in men, it is important to make sure the diagnosis is correct. The presence of the above symptoms in a man does not indicate epididymitis. To confirm the diagnosis, it is important to conduct a full diagnosis, including:
- clinical blood tests for suspected epididymitis are mandatory;
- microscopic examination of urethral discharge;
- smear for the presence of sexually transmitted infections;
- examination of the scrotum with an ultrasound machine, Doppler sonography;
- cystoureteroscopy.
Tuberculous epididymitis
Tuberculosis is a disease that can affect almost any organ, including the epididymis. Diagnosis and treatment of primary genitourinary tuberculosis is complex and requires invasive studies, including biopsy. This is necessary to distinguish tuberculous epididymitis from other diseases of the scrotum, for example, bacterial inflammation of the appendages or malignant tumors.
Mycobacterium tuberculosis enters the appendages either hematogenously or directly from the prostate gland and seminal vesicles.
Epididymitis may be a complication of treatment with the BCG vaccine for superficial bladder cancer. This occurs in 0.4% of patients treated in this way.
Isolated tuberculous epididymitis is rare and presents significant difficulties for diagnosis, since clinical manifestations and tomography data are very similar to a malignant tumor. The disease is accompanied by unilateral enlargement of the appendage, pain in the scrotum area, often there is an increase in temperature and impaired urination, for example, its frequency.
For diagnosis, urine cultures are performed, but in half of the cases mycobacteria cannot be detected in it. Ultrasound and tomography of the urinary tract are prescribed to exclude renal tuberculosis. Fine-needle aspiration biopsy and examination of the resulting material under a microscope are also used.
Tuberculous epididymitis is potentially curable with anti-TB drugs if diagnosed early. According to the recommendations of European urologists, treatment includes a combination of three anti-tuberculosis drugs for a period of 3 months, followed by two drugs for another 3 months. An alternative regimen is to use a combination of four agents for 2 months. If the disease develops against a background of suppressed immunity (for example, with HIV infection), the duration of therapy is at least 9-12 months. This treatment is prescribed by a phthisiatrician.
In advanced cases, surgery is necessary - removal of the epididymis along with the testicle. It is performed in case of ineffectiveness of medications or when complications develop, for example, abscess of the scrotal organs.
Laboratory research methods
To identify epididymitis, the causes of which are unknown to the patient, tests are taken to the laboratory. A general analysis and bacterial culture of urine, as well as culture of urine to determine the nutrient medium, are mandatory. The results of these tests will allow us to find the cause of infection and development of the disease and prescribe adequate and effective treatment.
How to identify the causative agent of the disease?
To determine epididymitis, the patient is prescribed microscopy and bacteriological examination. The essence of microscopy is that material is taken, stained and examined under a microscope.
The bacteriological research method involves taking a culture on a nutrient medium. The material used is a smear from the urethra, prostate secretion, sperm and urine.
Types of urethral culture
The tests that were submitted to the laboratory can be checked for other diseases. For example, diseases that are transmitted only sexually are found in the urethra.
Another method of identifying the infection that caused the development of epididymitis is to insert a swab into the urethra to a depth of 1 cm. This swab is then sent to the laboratory to identify the bacteria. The results of this study will be ready within 24 hours. Once the doctor receives the results of all tests, he will be able to understand and tell the patient the causes of the disease.
To determine the severity of the inflammation, the urologist may order a complete blood test to find out the number of white blood cells in the blood. If there are a lot of them, this indicates that there is an active inflammatory process in the body.
One of the main tests is the Gram analysis of the urethra. This test can determine the presence of bacterial contamination.
Diagnostics
The doctor collects anamnesis (medical history) and complaints, examines the patient, and performs a rectal examination of the prostate gland.
External manifestations that allow one to suspect the disease:
- a painful lump that first covers the tail of the appendage and then spreads higher;
- elevation of the affected half of the scrotum;
- normal cremasteric reflex;
- erythema of the scrotum;
- reactive hydrocele - accumulation of fluid between the membranes of the testicle;
- signs of bacterial prostatitis or vesiculitis in adult patients;
- focal compactions in the form of “beads” in tuberculous epididymitis;
- developmental anomalies of the genitourinary system (in children), for example, cryptorchidism.
Diagnosis of epididymitis includes the following additional studies:
- general urine analysis, bacteriological examination and determination of the sensitivity of the isolated microorganism to antibiotics;
- recognition of sexually transmitted diseases, primarily chlamydia, using PCR - an analysis that reveals the genetic material of microbes in material - urine, blood, urethral smear;
- blood test to determine the number of leukocytes;
- immunofluorescence analysis to determine antibodies to the mumps pathogen;
- Ultrasound of the testicle and epididymis;
- Dopplerography of the scrotal organs, if necessary, to distinguish the disease from testicular torsion.
After prostate massage, a urethral swab is obtained. If gram-negative diplococci are detected in it, this confirms gonorrhea.
Computer imaging (tomography) is rarely used. It is indicated when there are difficulties in diagnosis. For example, these studies are necessary for the diagnosis of cysts, hydroceles, hernias, tumors, and abscesses.
In some cases, a cystoureterogram, retrograde urethrography, or cystoureteroscopy is prescribed.
Accurate diagnosis of the causes of the disease is very important because an incorrect diagnosis can lead to many adverse consequences. More than 50% of infectious agents that cause epididymitis are sexually transmitted. Therefore, examination and treatment of patients’ sexual partners is necessary. Some patients, such as children and older adults, have other causes, so it is important to answer all your doctor's questions openly.
Diseases with which differential diagnosis of epididymitis is carried out:
- testicular torsion;
- scrotal hernia;
- inguinal hernia;
- idiopathic swelling of the scrotum;
- hydrocele;
- pyocele (accumulation of pus between the membranes of the testicle);
- Henoch-Schönlein purpura;
- Behçet's disease;
- periarteritis nodosa;
- vasculitis;
- neuralgia or radicular pain (radiculitis);
- epididymal cyst;
- complications after vasectomy;
- spermatocele;
- testicular tumor, including hemorrhage into it;
- tumors of the testicular membranes, in particular mesothelioma;
- varicocele;
- urinary tract infections.
Acute epididymitis: treat immediately!
Acute epididymitis is an inflammation of the epididymis in men. There is a distinction between acute epididymitis on the left and acute epididymitis on the right - in the left or right epididymis.
For patients with acute forms of pathology, the first and most important treatment is bed rest; it is also worth fixing the scrotum in an elevated position. To do this, you can use swimming trunks or roll a towel into a roll and thus fix the scrotum so that there is a good outflow. Treatment consists not only of local treatment, but is also complex; the primary cause of the disease must be taken into account, because as we know independently, it is extremely rare.
What antibiotics are prescribed for acute left-sided and right-sided epididymitis? As a rule, these are drugs from the group of macrolides (Azithromycin), tetracyclines (Doxycycline), fluoroquinolones (Levofloxacin or Ofloxacin). Antibiotics for the treatment of epididymitis in men begin to be taken from the first day of inflammation, and the course lasts up to several weeks, and in severe cases, months.
Risk group
Acute testicular epididymitis is most often observed in men fifteen to thirty years old, as well as after sixty. Children very rarely suffer from this pathology.
According to statistics, every fourth man in the period from twenty to forty years suffers from this disease in acute form. Ten percent of diseases are accompanied by acute orchitis.
Treatment methods
The disease must be treated urgently, otherwise there is a high probability that it will develop into chronic acute epididymitis. Treatment is carried out with antibiotics.
Pathology is diagnosed by examination and palpation. In some cases, an ultrasound may be prescribed. Laboratory tests of urine are also performed.
Why is acute epididymitis dangerous?
If acute epididymitis is observed on the left or right, treatment is necessary. If the process is left to chance, it can develop into epididymo-orchitis. This is dangerous for the development of infertility.
Treatment
In most cases, conservative methods of therapy are used. Treatment at home includes bed rest. It is necessary to use a suspensor that pulls the scrotum up. This measure can significantly reduce pain in the inflamed organ.
Spicy foods and alcohol are excluded from the diet. In the first 3 days of illness, pain can be relieved by applying cold compresses to the affected area. For pain relief, suppositories with ketorolac and drotaverine are used.
To cure epididymitis, you need to undergo a course of treatment with antibacterial drugs. Often 2 antibiotics are prescribed at once, because the pathology is caused by mixed microflora.
In men under 40 years of age, treatment is carried out according to two main schemes:
- cephalosporins intramuscularly in combination with tetracycline antibiotic tablets, course of treatment for 10 days;
- modern macrolides (for example, Sumamed) for 3-5 days.
Treatment of epididymitis in men over 40 years of age should be carried out with one of the following medications:
- Levofloxacin or Ciprofloxacin for oral administration;
- a combination of a sulfonamide agent and trimethoprim (Co-Trimoxazole) in tablets.
The doctor decides which antibiotics to treat the disease in each case. Health care workers have statistics on the sensitivity of microorganisms to different drugs in each region. Depending on the local characteristics of microbial resistance to drugs, the doctor may change the type of antibiotic and the duration of the course of treatment in order to achieve recovery for the patient. Incorrect treatment in the early stages can lead to complications that require surgery.
In patients with non-infectious causes of the disease, anti-inflammatory drugs, such as ibuprofen, are often used. In case of a chronic process, physiotherapy is prescribed.
Absorbable drugs for epididymitis help to avoid sclerosis of the appendage tissue. These include, for example, Longidaza suppositories. They must be inserted into the rectum at night for 10-20 days. They are prescribed if, after epididymitis, the appendage is enlarged.
If, after following all the recommendations, the disease does not go away, a consultation with a urologist and additional examination is prescribed. It is important to ensure that there is no orchitis, or inflammation of the testicles. This disease not only significantly impairs a man's reproductive abilities, but can also cause the bacteria to spread through the blood to other organs. In addition, treatment failure may be due to testicular tumor.
If sexual transmission of bacteria is confirmed, it is necessary to notify the patient’s sexual partner and prescribe him a course of treatment, even in the absence of symptoms. Otherwise, after treatment, re-infection will occur.
When an abscess forms, it is opened. If acute purulent epididymitis has developed, the epididymis along with the testicle is removed. The same operation is performed for frequent exacerbations of the chronic process. In this case, the function of the organ has already been lost, and the likelihood of infection spreading to the testicle remains.
Traditional medicine recipes
In addition to antibiotics, after consultation with a doctor, you can use folk remedies.
There are quite a few recipes for various herbal infusions. The plants that make up them have antiseptic, anti-inflammatory, soothing properties, and accelerate tissue regeneration after inflammation has ended. Here are some of them.
- Make a collection of equal parts of juniper cones, shepherd's purse and bearberry leaves, dandelion and steelhead roots, anise and dill seeds. Place 3 tablespoons in a half-liter container. spoons of this collection, add boiling water and leave for half an hour. Then strain the resulting infusion and drink it in 2 doses throughout the day.
- Make a collection of equal quantities of birch leaves, juniper cones, celandine leaves, steelweed roots and cinquefoil grass. Place 4 tablespoons in a liter container. spoons of the mixture and pour boiling water, let cool, then strain. Drink during the day in 3 doses.
- Mix equal amounts of corn silk, birch buds, dry bean pods and violet flowers. Make an infusion from 1 table. spoons of the mixture and 0.5 liters of boiling water. You need to take it 2 spoons three times a day.
- Make a mixture of equal quantities of lingonberry leaves, horsetail grass and tansy flowers. Take table 4. spoons of the collection and make an infusion in a half-liter container. Drink in 2 doses during the day.
The following components can be added to all medicinal preparations:
- peppermint;
- yarrow herb;
- calamus and licorice roots;
- wormwood grass;
- strawberry and currant leaves;
- St. John's wort, nettle;
- rosehip berries;
- Linden blossom.
Herbal infusions can be taken as a course for a month. For chronic epididymitis, if there is no need for surgery, treatment is repeated 3-4 times a year, especially in the off-season or after colds.
Medicines
Photo: hvylya.net
To begin treatment, it is recommended to use fluoroquinolones (Ofloxacin, Levofloxacin), since they penetrate well into the tissues of the genitourinary system and have a fairly wide spectrum of antimicrobial activity. The duration of treatment should be at least 10 days. In case of drug intolerance, fluoroquinolones can be replaced with antibiotics from the macrolide group (Erythromycin, Clarithromycin).
To treat the symptoms of inflammation, non-steroidal anti-inflammatory drugs (Ibuprofen, Diclofenac, Analgin, Nimesulide) are used. In a hospital setting, the use of intramuscular injections is justified. For young children, rectal suppositories are used. To enhance the anti-inflammatory effect, it is justified to use these drugs in combination with antispasmodics (Drotaverine, Papaverine) and antihistamines (Diphenhydramine, Clemastine).
In case of severe symptoms of fever, to replenish fluid losses, infusion therapy (solutions of sodium chloride, glucose, Ringer and others) is prescribed in a volume of up to 1-1.5 liters per day.
Complications
In most cases, acute epididymitis can be successfully treated with antibiotics. Long-term sexual or reproductive problems do not develop. However, the infection can recur, ultimately leading to the development of complications.
Bilateral epididymitis causes male infertility. The true prevalence of reproductive problems is unknown, but acute epididymitis is a rare complication. The impairment of sperm quality is transient and has the nature of secondary leukocytospermia, that is, an admixture of leukocytes or pus.
In severe cases of purulent process, right-sided or left-sided epididymitis becomes the cause of testicular abscess. An abscess that breaks out can cause the formation of a fistula.
This complication can only be treated surgically - so-called hemicastration is performed (removal of the testicle and epididymis on one side).
Impaired blood circulation in the surrounding edematous tissues can cause testicular infarction - cessation of its blood supply. As a result, organ tissues are irreversibly damaged and die.
Another complication of the disease is obstruction of the vas deferens, as a result of which sperm from one testicle do not enter the genital tract. A type of infertility called azoospermia develops. The incidence of this complication is unknown. Such consequences of epididymitis have an extremely adverse effect on a man’s ability to fertilize. To prevent this, it is necessary to consult a doctor in a timely manner; in case of an acute process, you can call an ambulance. Such a patient is usually sent to the hospital.
If the patient's inflammation has spread from the epididymis to the testicular tissue, the following complications may occur:
- hypogonadism, resulting from testicular atrophy and developing in 30-50% of patients;
- infertility in 7-13% of patients; the interstitial tissue of the testis is mainly affected, rather than the Leydig or Sertoli cells, but the number, motility and morphology of sperm may change;
- constant pain in the scrotum - orchalgia.
During treatment, it is important to take the entire course of antibiotics, even if all symptoms of the disease have already disappeared. In addition, you should visit your doctor after completing therapy to make sure there are no complications.
The outcome of the disease is worse in the presence of such aggravating factors:
- diabetes;
- elderly age;
- significant increase in body temperature;
- increase in the number of leukocytes in the blood;
- an increase in the content of urea and C-reactive protein in a biochemical blood test.
Patients with epididymitis resulting from sexually transmitted diseases (chlamydia, gonorrhea and others) have a risk of contracting HIV infection, which is 5-9 times higher than that of healthy people. Therefore, all sexual partners of such patients should undergo examination and treatment.
Surgery for acute epididymitis
Surgery for acute epididymitis is carried out only for emergency indications, when the process has already started, then doctors resort to surgical treatment - epididymectomy. Acute epididymitis, surgery involves removal of the affected organ or part thereof. This operation is performed in a hospital under local or general anesthesia. An important indication for surgery is the chronic form with frequent exacerbations, the infiltrates that arise in the testicular cavity are painful, dense, when the nature of the inflammation changes and it becomes tuberculous, when the treatment process is started, an abscess occurs, necrotizing tissues grow, which leads to damage to everything testicles. And so about the operation itself: the preparatory stage consists of consulting the patient with a urologist or andrologist, examining the affected organ, the doctor must assess the severity and extent of the damage. Collect all the necessary tests, the main thing is ultrasound or MRI, blood tests, urine tests, tests for HIV, syphilis. And also before the operation itself, a consultation with an anesthesiologist. A longitudinal incision is made on the scrotum, the testicle is exposed and brought out, thus exposing its affected appendage, the accessory ligament is crossed and everted out of the testicular membrane, the vessels are tied up and the vas deferens is cut off, the tissue is tucked back into the wound and sutured, having previously placed drainage in the wound. But it is worth considering that in order to avoid torsion of the testicle in the scrotum, it is sutured to the tissues of the scrotum itself.
Prevention
A measure to prevent the disease is timely diagnosis and treatment of sexually transmitted infections, including in sexual partners.
Other ways to avoid illness:
- sexual abstinence;
- using condoms, which reduces the likelihood of infection by 90%;
- sexual contact with only one partner;
- vaccination of children against mumps;
- maintaining personal hygiene.
If epididymitis is caused by long-term use of amiodarone, this drug must be replaced with another antiarrhythmic drug.
Causes and risk factors
Epididymitis develops for a number of reasons, of which the main and most common is infection. Based on the nature of the inflammatory process, specific and nonspecific forms of the disease are distinguished.
Specific:
- tuberculosis;
- STDs (sexually transmitted infections);
- brucellosis.
Non-specific:
- hemophilus influenzae, pseudomonas or Escherichia coli;
- chlamydia;
- staphylococci and streptococci;
- ureplasma.
Nonspecific causes also include viruses and fungi. In men under 40 years of age, inflammation of the epididymis most often develops as a result of infection with sexually transmitted infections. In older people, the disease is provoked by intestinal flora, which is the main cause of pathology in adherents of anal sex.
Main routes of transmission
Retrograde:
- during unprotected sexual intercourse;
- during medical manipulations with the genitourinary organs.
Hematogenous – for infections of the pelvic organs and chronic infections of other organs (influenza, sinusitis, pneumonia, etc.).
Other causes of epididymitis:
- constant use of medications;
- ingress of chemicals into the urethra during medical procedures or reflux of urine into the appendages;
- genital injuries are complications after adenomectomy and other surgical procedures;
- congestion – blood in the pelvic vessels can stagnate due to interrupted sexual intercourse, masturbation and frequent erections without sex, constipation and hemorrhoids, cycling;
- pathology of the testicles - the inflammatory process can be triggered by torsion of the epididymis, as well as by the entry of sperm into the testicular tissue as a result of surgical sterilization (ligation of the spermatic cord).
The main risk factors include:
- weakened immunity due to serious illnesses, as well as after surgery or chemotherapy;
- problems with urination;
- hypothermia/overheating of the pelvic organs;
- urinary tract infections, including purulent diseases of the genital organs;
- systemic diseases (Behcet's disease, sarcoidosis, etc.);
- sexual intercourse without a condom.
Instrumental method
Instrumental methods of modern diagnostics include ultrasound and magnetic resonance imaging.
Ultrasound is used to examine the scrotum. Using it, you can quickly assess the nature of the damage to a given organ. But there are cases when it is not possible to accurately determine the stage of the inflammatory process using ultrasound, then an MRI is prescribed. This method is the most modern at this stage of scientific development. Using MRI, you can accurately determine the condition of the testicles and appendages. Unfortunately, this diagnostic method is quite expensive, and not every patient can afford it.
Thanks to these two methods, the presence in the body of cysts, hernias, hydroceles and various neoplasms that appeared as a result of epididymitis is determined. Also, these research methods will help determine the severity of the disease.
To prescribe the correct treatment, a specialist must accurately establish the diagnosis and the true causes of the disease. Most infections that lead to inflammation of the epididymis are transmitted exclusively through sexual contact, but in men over 40 years of age, epididymitis can occur due to chemical inflammation or urinary infections.
Pathogenesis
There are several ways that infection can enter the body.
- The first is hematogenous, that is, through the blood. This indicates that the cause of inflammation of the appendages is sepsis, hemorrhoids and a number of other diseases that are infectious in nature.
- The second route of infection is lymphogenous. In this case, infection of the appendages occurs through the lymph.
- The third path is canalicular, in which the infection enters the appendages through the vas deferens.
- The last route is secretory, when infection occurs as a result of testicular inflammation.
Many doctors come to the conclusion that the most common route of infection is the vas deferens. Damage to the testicular appendages occurs with the active development of epididymo-orchitis or injury to the genitourinary organs.
With epididymitis, the patient experiences morphological changes, such as infiltration changes in the tissues of the appendages. There are cases when its shell thickens and even swells and serous exudate accumulates.