An antibiotic (antibacterial drug, antimicrobial agent) is a drug that is effective in treating bacterial infections. Its effect is to directly affect the bacterium, it kills it. Its effect may also be to slow down the proliferation of bacteria, which allows the immune system to cope with it. The high prevalence of infections, a large selection of antibiotics for children, and the unjustified prescription of these drugs for diseases in children and adults have led to threatening consequences for human life—antibiotic resistance. According to the Eurasian recommendations, 25,000 deaths annually in the EU are associated with antibiotic resistance. At the moment, antimicrobial agents are an irreplaceable resource for humanity. Antibacterial resistance can be considered a threat to national security.
Before moving on to the choice of a children's antibiotic, consideration of dosage, duration of use, it is necessary to analyze and explain the main points in the formation of resistance to antibacterial agents. Only after this can one adequately judge the choice and approach to prescribing these medications.
Story
Zalman Vaksman - one of the fathers of antibiotics Antibiotics are substances of natural or semi-synthetic origin that inhibit the growth of living cells. The term was coined by Z. Waksman, an American microbiologist who received the Nobel Prize in 1952 for the discovery of streptomycin. The term “antibios” itself was coined by L. Pasteur and carried a certain meaning - “life against life.” The first antibiotic was penicillin , isolated from the fungus Penicillum notatum. Observations of the relationship between the culture of streptococcus and fungus were begun by Fleming in a London hospital in the 20s of the last century. However, his speech at the Second International Congress of Microbiologists did not make an impression on the public (perhaps due to the fact that he was not a very skilled speaker). The further history of the study of penicillin is connected with the names of the members of the “Oxford Group” - Howard Florey and Ernst Chain. Chain was involved in isolating penicillin, and Flory was testing it on animals. The first trial of penicillin took place in 1941 on a London policeman dying of sepsis. Scientists managed to improve his condition, but the supply of the drug was too small, and the patient died.
The same Petri dish with a culture of Staphylococcus sp., in which Alexander Fleming, upon returning from vacation, discovered the mold Penicillium notatum instead of bacterial colonies. 1928 In 1945, Fleming, Chain and Florey were awarded the Nobel Prize. Penicillin, optimally combining high antibacterial activity and safety for humans, is still used successfully. gramicidin was isolated in 1939 , streptomycin in chlortetracycline in 1945 chloramphenicol in 1947 , and by 1950 more than 100 antibiotics had been described. Over time, it became clear that existing antibiotics were not active enough against microorganisms: this was the reason for the start of chemical research and the creation of semi-synthetic antibiotics. Since then, various groups of antibacterial agents have been discovered. Thus, in Russia today about 30 groups of antibiotics are used. Among them, there are drugs with antibacterial, antiparasitic, antifungal and antitumor effects. The postulates of antibiotic therapy were also formed. The basic rules of antibacterial therapy can be formulated as follows:
1. Identify the causative agent of the disease;
2. Determine the drugs to which the pathogen is most sensitive;
3. For an unknown pathogen, use either a drug with a broad spectrum of action, or a combination of two drugs, the total spectrum of which includes probable pathogens;
4. Treatment should be started as early as possible;
5. Doses of drugs must be sufficient to provide concentrations in cells and tissues that prevent reproduction ( bacteriostatic ) or destroy bacteria ( bactericidal );
6. The duration of treatment must be sufficient; a decrease in body temperature and weakening of other symptoms are not grounds for stopping treatment;
7. The choice of rational routes of drug administration plays a significant role, given that some of them are not completely absorbed from the gastrointestinal tract, do not penetrate the blood-brain barrier , etc.;
8. The combined use of antibacterial agents must be justified, since if the combination is incorrect, the total activity may be weakened and their toxic effects may be cumulative.
Let us consider the antibacterial drugs themselves from the point of view of the nature, spectrum and mechanism of their action.
Antibiotics act directly on the etiological factor, and by the nature of their action they are bacteriostatic and bactericidal:
- Bacteriostatic drugs inhibit the growth and reproduction of microorganisms. They do not cause their death. It is assumed that the immune defense mechanisms are able to independently cope with the destruction and elimination of microbes. Bacteriostatic drugs include macrolides, clindamycin, streptogramins, chloramphenicol, tetracyclines;
- Bactericidal drugs lead to the death of microorganisms, and the body only needs to ensure their elimination. These include beta-lactam antibiotics, aminoglycosides, fluoroquinolones, glycopeptides and others (trimethoprim, metronidazole, rifampicin, etc.).
How are microorganisms neutralized? There are several mechanisms of action of antibiotics:
- Violation of cell wall synthesis by inhibiting peptidoglycan synthesis (penicillin, cephalosporin, monobactams), the formation of dimers and their transfer to growing peptidoglycan chains (vancomycin), chitin synthesis (nikkomycin). Antibiotics acting according to this mechanism have a bactericidal nature of action; they do not act on resting cells and L-forms (devoid of a cell wall) of bacteria;
- Impaired functioning of membranes due to disruption of their integrity, formation of ion channels, binding of ions into lipid-soluble complexes and disruption of their transport (nystatin, gramicidins, polymyxins);
- Suppression of nucleic acid synthesis : DNA (streptomycin, griseofulvin, rifampicin, rifamycin, vancomycin) and RNA (bruneomycin, rubomycin, olivomycin);
- Violation of protein synthesis by the cell (tetracyclines, macrolides);
- Violation of the synthesis of purines and pyrimidines (azaserine, sarcomycin);
- Inhibition of the respiratory chain (antimycins, oligomycins).
For ease of use, it is customary to classify antibiotics according to their spectrum of antimicrobial action:
- Acting predominantly on gram-positive microflora: biosynthetic penicillins, oxacillin, first generation macrolides, lincomycin, rifampicin, rifamycin, ristomycin, vancomycin;
- Acting predominantly on gram-negative microflora: polymyxin;
- Broad spectrum of action: semisynthetic penicillins (except oxacillin), cephalosporins, second generation macrolides, tetracyclines, aminoglycosides;
- Antifungal antibiotics: nystatin, levorin, amphotericin B, mycoheptin, griseofulvin, etc.;
- Antitumor antibiotics: olivomycin, rubomycin, etc.
The value of antibiotics as medicines is undoubtedly very high. The discovery of these drugs has made it possible to get rid of many previously fatal infections. But microorganisms quickly adapt to changing environmental conditions, including acquiring resistance to antibiotics.
There are several “basic” mechanisms of resistance:
1.
Changing
the target of an action ;
2. Enzymatic inactivation of an antimicrobial drug;
3. Active removal of the antimicrobial drug from the microbial cell ( efflux );
4. Violation of the permeability of the microbial cell to the antimicrobial drug;
5. Formation of metabolic “shunts”.
Methicillin-resistant Staphylococcus aureus The emergence of antibiotic-resistant strains of bacteria is undoubtedly dangerous both for the person from whom they are isolated and for many other people. Increased resistance leads to worsening of the course of infectious diseases, increased mortality, and increased healthcare costs.
Let's look at the most popular classes of antibiotics:
Classification of antibiotics by chemical structure and origin
1. Natural - waste products of bacteria, fungi, actinomycetes:
- Gramicidins®;
- Polymyxins;
- Erythromycin®;
- Tetracycline®;
- Benzylpenicillins;
- Cephalosporins, etc.
Read: About natural antibiotics and their use in the treatment of diseases
2. Semi-synthetic - derivatives of natural antibacterials:
- Oxacillin®;
- Ampicillin®;
- Gentamicin®;
- Rifampicin®, etc.
3. Synthetic, that is, obtained as a result of chemical synthesis:
- Levomycetin®;
- Amikacin®, etc.
Penicillins
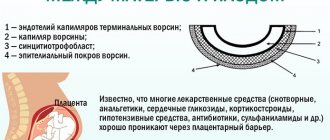
Benzylpenicillin The oldest group, but not losing its relevance. Penicillins are β-lactam antibiotics and have a four-membered β-lactam ring in their structure. In turn, they are divided into natural (biosynthetic), secreted by certain strains of mold fungi, and semi-synthetic, obtained through laboratory modification. According to the mechanism of action, all penicillins are bactericidal: they block the final stages of peptidoglycan synthesis and thereby lead to the death of bacteria. This, in turn, explains the low toxicity of penicillins for humans, whose cells are not characterized by peptidoglycan synthesis. To target bacteria that have acquired resistance through the synthesis of β-lactamase enzymes, drugs combined with clavulanic acid (a β-lactamase inhibitor) were created. According to classical sources, they have a fairly wide spectrum of action, and semisynthetic penicillins, due to their acid resistance and protection from β-lactamases, expand it significantly. But due to the growing resistance of microorganisms, penicillins do not always produce a sufficient medicinal effect.
Classification
1) Biosynthetic:
- sodium, potassium and novocaine salts of benzylpenicillin;
- prolonged (bicillin-3, bicillin-5, retarpen);
- phenoxymethylpenicillin;
2) Semi-synthetic:
- ampicillin (G->G+);
- oxacillin (penicillinase-resistant, acid-resistant);
- Ampiox (ampicillin + oxacillin);
- amoxicillin: acid-resistant, trade names - Amoxicillin, Amoxil-KMP, Bactox, Gramox, Ospamox, Flemoxin, Hiconcil, E-Mox;
- Amoxicillin + clavulanic acid (amoxiclav).
Penicillins have the lowest toxicity among antibiotics. The main side effects are allergic reactions (urticaria, Quincke's edema, anaphylactic shock), gastrointestinal disorders (nausea, vomiting, diarrhea, when using ampicillin and inhibitor-protected penicillins - pseudomembranous colitis). Certain types can cause hyperkalemia (usually benzylpenicillin-K-salt), hypernatremia (usually benzylpenicillin-Na-salt), non-allergic maculopapular (ampicillin) rash, as well as pain at the injection site, anemia, thrombocytopenia, neutropenia, transient hematuria in children.
Drug interactions
- Penicillins cannot be mixed in the same syringe or in the same infusion system with aminoglycosides due to their physicochemical incompatibility;
- When ampicillin is combined with allopurinol, the risk of ampicillin rash increases;
- The use of high doses of benzylpenicillin potassium salt in combination with potassium-sparing diuretics, potassium supplements or ACE inhibitors predetermines an increased risk of hyperkalemia;
- Caution is required when combining penicillins active against Pseudomonas aeruginosa with anticoagulants and antiplatelet agents due to the potential risk of increased bleeding; It is not recommended to combine with thrombolytics;
- The use of penicillins in combination with sulfonamides should be avoided, as this may weaken their bactericidal effect;
- Cholestyramine binds penicillins in the gastrointestinal tract and reduces their bioavailability when taken orally;
- Oral penicillins may reduce the effectiveness of oral contraceptives by impairing the enterohepatic circulation of estrogens;
- Penicillins can slow down the elimination of methotrexate from the body by inhibiting its tubular secretion.
Cephalosporins
General structure of cephalosporins Also classified as β-lactam antibiotics, they are one of the most numerous and frequently prescribed classes due to their low toxicity. The mechanism of action is similar to penicillins, they have 4 generations, each of which is ahead of the previous one in the spectrum of action.
I generation:
1) Parenteral (cefazolin);
2) Oral (cephalexin, cefadroxil). Antibiotics are active against Streptococcus spp. (S.pyogenes, S. pneumoniae) and methicillin-sensitive Staphylococcus spp. In terms of the level of antipneumococcal activity, first-generation cephalosporins are inferior to aminopenicillins and most later cephalosporins. First generation cephalosporins have a narrow spectrum of action and a low level of activity against gram-negative bacteria. The main indications for the use of cephalosporin are preoperative prophylaxis in surgery, as well as the treatment of skin and soft tissue infections; to the use of cefazolin - streptococcal tonsillopharyngitis, community-acquired infections of the skin and soft tissues of mild severity.
II generation:
1) Parenteral (cefuroxime);
2) Oral (cefaclor, cefuroxime axetil).
With a similar antimicrobial spectrum, cefuroxime is more active against Streptococcus spp.
and Staphylococcus spp. The spectrum of action of cephalosporins of the second generation against gram-negative microorganisms is wider than that of representatives of the first generation; The activity of cefuroxime against gonococci is of clinical significance. Due to the resistance of cefuroxime to β-lactamases, it is active against M. catarrhalis, Haemophilus spp., E. coli, Shigella spp., Salmonella spp., P. mirabilis, Klebsiella spp., P. vulgaris, C. diversus. The main indications for use are community-acquired upper respiratory tract infections, hospital-acquired community-acquired pneumonia, community-acquired skin and soft tissue infections, urinary tract infections, perioperative preparation in surgery.
III generation:
1) Parenteral (cefotaxime, ceftriaxone, ceftazidime, cefoperazone, cefoperazone + sulbactam);
2) Oral (cefixime, cefibutene).
The basic antibiotics in this group are ceftriaxone and cefotaxime, which have high activity against Streptococcus spp., Staphylococcus aureus, corynebacteria, meningococcus, gonococci, H. influenzae and M. catarrhalis, penicillin-resistant pneumococcus and viridans streptococcus.
They have high activity against almost the entire Enterobacteriaceae family. Ceftazidime and cefoperazone also have activity against P. aeruginosa, but significantly less activity against streptococci. Cefixime and cefibutene have little activity against Streptococcus spp., the Enterobacteriaceae family and pneumococci. Indications are moderate and severe community-acquired and nosocomial infections of the lower respiratory tract, urinary tract, skin, soft tissues, bones, joints, intra-abdominal infections, infections of the pelvic organs, meningitis, sepsis, infections due to immunodeficiency. Cefixime and cefibutene are also prescribed for mild to moderate pyelonephritis in children, pregnant and lactating women.
IV generation:
1) Parenteral (cefepime).
It is similar in parameters to third generation drugs, but also has high activity against P. aeruginosa, Enterobacter spp., C. freundii, Serratia spp., M. morganii, P. stuartii, P. rettgeri and non-fermenting microorganisms.
Indications are severe infections of the lower respiratory tract, urinary tract, skin, soft tissues, bones, joints caused by multidrug-resistant microflora, as well as sepsis. Common side effects of cephalosporins include allergic reactions and gastrointestinal dysfunction; Convulsions from the central nervous system, cholestasis and pseudocholelithiasis from the liver may be observed. The allergy is cross-allergic to all cephalosporins, and cross-allergy with penicillins can also be observed. Due to low excretion in children and the elderly, their half-life of cephalosporins increases. Combination with aminoglycosides or loop diuretics may cause a nephrotoxic effect. Antacids reduce the absorption of oral forms.
Carbapenems
General structure of carbapenems They belong to β-lactam antibiotics; compared to penicillins and cephalosporins, they are more resistant to the action of β-lactamases. These include impineme and meropenem . The mechanism of action is similar to that of penicillins and cephalosporins. They have a wider spectrum of activity, acting on many Gr+ and Gr– bacteria. Staphylococci, streptococci, including pneumococci, gonococci, meningococci, bacteria of the Enterobacteriaceae family, spore-forming and non-spore-forming anaerobes are sensitive to them. Indications: 1. Severe infections of the lower respiratory tract, urinary tract, intra-abdominal, pelvic organs, skin and soft tissues, sepsis caused by multiresistant and mixed microflora; 2. Endocarditis, infections of bones and joints - only impinema; 3. Meningitis - only meropenem. Frequent side effects: allergic, dysfunction of the gastrointestinal tract, from the central nervous system - dizziness, tremor, convulsions. Allergic reactions are cross-reactions with all carbapenems, and in 50% of patients also with penicillins. Cannot be used with other β-lactam antibiotics due to their antagonism.
Classification of antibiotics by spectrum of action and purposes of use
| Acting mainly on: | Antibacterial products with a wide spectrum of action: | Anti-tuberculosis agents | |
| Gram+: | Gram-: | ||
| biosynthetic penicillins and 1st generation cephalosporins; macrolides; lincosamides; preparations Vancomycin®, Lincomycin®. | monobactams; cyclical polypeptides; 3rd generation cephalosporins. | aminoglycosides; chloramphenicol; tetracycline; semi-synthetic extended spectrum penicillins (Ampicillin®); 2nd generation cephalosporins. | Streptomycin®; Rifampicin®; Florimycin®. |
Monobactams
1 - penicillins; 2 - cephalosporins; The β-lactam ring is highlighted in red. They belong to β-lactam antibiotics; in clinical practice, aztreonam , which has a narrow spectrum of antibacterial activity. Aztreonam is used as a reserve drug for the treatment of infections caused by Gr-microflora. Active against bacteria of the Enterobacteriaceae family, P. aeruginosa, including strains resistant to aminoglycosides, penicillins, and cephalosporins. Given the narrow spectrum of action of aztreonam, it should be prescribed in combination with antibiotics that are active against Gr+ microflora. The drug rarely causes allergic reactions, but reactions from the gastrointestinal tract, liver, central nervous system, and kidneys are also common. In patients with renal and hepatic insufficiency, the dose is adjusted. Aztreonam should not be combined with carbapenems due to their drug antagonism.
Aminoglycosides
Streptomycin Drugs of this class are almost the same age as penicillins: the first of them were discovered in 1944. There are currently three generations of aminoglycosides:
I generation:
- streptomycin;
- neomycin;
- kanamycin;
II generation:
- gentamicin;
- tobramycin;
- netilmicin;
III generation:
- amikacin.
According to the mechanism of action, the drugs are bactericidal ; it is achieved by blocking protein synthesis on ribosomes. These drugs are of primary importance in the treatment of nosocomial infections caused by Gr-anaerobes and infective endocarditis. Streptomycin and kanamycin are active against M. tuberculosis , while amikacin is more active against atypical mycobacteria. Streptomycin is also active against pathogens of plague, tularemia, and brucellosis. Prescribed as empirical therapy for sepsis of unknown etiology, infective endocarditis, post-traumatic and postoperative meningitis, fever in patients with neutropenia, nosocomial pneumonia, pyelonephritis, intra-abdominal infections, pelvic organ infections, diabetic foot, osteomyelitis, septic arthritis; as local therapy for eye infections. As a specific therapy, streptomycin is used in the treatment of plague, tularemia, brucellosis, tuberculosis; gentamicin - in the treatment of tularemia; kanamycin - for tuberculosis. They have nephrotoxic and ototoxic effects. They can lead to disorders of the vestibular apparatus and block neuromuscular transmission. Aminoglycosides cannot be mixed with β-lactams and heparin due to their physicochemical incompatibility. Nephrotoxicity and ototoxicity increase when combined with other nephro- and ototoxic drugs: polymyxin B, amphoterecin B, ethacrynic acid, furosemide, vancomycin. Neuromuscular blockade is enhanced when combined with drugs for inhalation anesthesia, opioid analgesics, and magnesium sulfate.
Levomycetin
Levomycetin, or chloramphenicol, is a natural antibiotic with a wide spectrum of action, active against a significant number of gram-positive and gram-negative microorganisms, many large viruses. According to its chemical structure, this derivative of nitrophenylalkylamines was first obtained from the culture of actinomycetes in the mid-20th century, and two years later it was also synthesized chemically.
Levomycetin has a bacteriostatic effect on microorganisms. The mechanism of action of antibiotics on a bacterial cell is to suppress the activity of catalysts for the formation of peptide bonds in ribosomes during protein synthesis. Resistance to chloramphenicol in bacteria develops very slowly. The drug is used for typhoid fever or dysentery.
Tetracyclines
Basic chemical structure of tetracyclines Like penicillins, they are one of the earliest classes of antibiotics. They were discovered in the 40s of the last century, but currently their use is limited. They have a bacteriostatic effect associated with disruption of protein synthesis in the microbial cell. Currently, many microorganisms have become resistant to tetracyclines, but drugs (natural tetracycline and synthetic doxycycline) remain important for rickettsiosis, chlamydial infections, and severe acne. Tetracyclines have a large number of side effects. They disrupt the functions of the gastrointestinal tract, affect the central nervous system (dizziness, increased intracranial pressure), cause metabolic disorders (impaired protein metabolism with a predominance of catabolism, increased azotemia), lead to disturbances in the formation of bone tissue, and cause allergic reactions that cross all tetracyclines. Tetracyclines have a very high hepatotoxic effect, up to the development of fatty degeneration or liver necrosis. Risk factors for hepatotoxicity include rapid intravenous administration of the drug, underlying liver dysfunction, pregnancy, and renal failure. When tetracyclines are taken orally simultaneously with antacids containing calcium, aluminum and magnesium, sodium bicarbonate and cholestyramine, their bioavailability may decrease due to the formation of non-absorbable complexes and an increase in the pH of the gastric contents. It is not recommended to combine tetracyclines with iron supplements, since this may interfere with the absorption of both. Carbamazepine, phenytoin and barbiturates increase the hepatic metabolism of doxycycline and reduce its concentration in the blood, which may require dose adjustment of this drug or replacement with tetracycline. When combined with tetracyclines, the effect of estrogen-containing oral contraceptives may be weakened. Tetracyclines may enhance the effect of indirect anticoagulants due to inhibition of their metabolism in the liver, which requires careful monitoring of prothrombin time. There are reports that when tetracyclines are combined with vitamin A preparations, the risk of pseudotumor cerebri syndrome increases.
Myths associated with antibiotics
Antibiotics have been and remain drugs around which many myths swirl. Let's discuss the most famous of them.
Myth 1: Antibiotics can be used without a doctor's prescription.
Uncontrolled use of antibiotics often leads to the emergence of resistant microorganisms, which is quite a problem for world medicine. The number of effective drugs is decreasing, and, according to scientists, in order for the activity of the antibiotic to be restored, it is necessary to stop using it for at least 40 years.
Myth 2: It is necessary to start taking an antibiotic at the first manifestation of acute respiratory infections symptoms.
In most cases, acute respiratory diseases have a viral etiology. Antibiotics, as we know, are not able to affect viruses. At the same time, these drugs are quite toxic and can cause side effects in a weakened body.
Myth 3: The duration of antibiotic therapy should be at least 10–14 days.
The arsenal of modern antimicrobial drugs makes it possible to take both a single dose and short courses. The duration of treatment depends on the nature of the disease. Thus, for uncomplicated respiratory tract infections, the use of appropriate drugs occurs over a course of 3–5 days, and for chronic osteomyelitis it extends over several months.
Myth 4: Antibiotics can be used for a couple of days and, if it becomes easier, discontinued.
Due to the growing resistance of microorganisms, taking antibiotics should be appropriate, take a course and vary depending on the degree of effectiveness of the drug. Even if the condition improves, it is necessary to continue the course of treatment until it ends.
Myth 5: There are antibiotics that can be used frequently.
This is not true; all antibiotics are quite toxic drugs and have a large number of side effects. These can be allergic manifestations, disorders of the gastrointestinal tract, liver, kidneys, neurological disorders, disorders of the hematopoietic organs and much more.
Myth 6: Antibiotics kill all living things and should absolutely not be taken.
A correctly selected antibiotic has a greater effect on the microorganism, but we should not forget that this fight takes place in the patient’s body and, accordingly, the structures of his body react to what is happening. It would be foolish to deny the absence of side effects, but they are all eliminated after the end of treatment.
Myth 7: Antibiotics disrupt the function of the gastrointestinal tract, and therefore they must be used together with bifid drugs.
There is no evidence of the effectiveness of co-administration. Accordingly, this will only increase the cost of treatment, but will not bring any effect.
Myth 8: Antibiotics are necessary for food poisoning.
Poisoning is most often caused not by the microorganisms themselves, but by their toxins. Antibiotics are ineffective in the fight against toxins.
Myth 9: Antibiotics should be used for fever.
Yes, no matter how stupid it may sound, but this is heard quite often. Antibiotics do not have an antipyretic effect, and therefore their use when the temperature rises is pointless.
Myth 10: Antibiotics should be taken with milk or citrus juice.
Milk can lead to the neutralization of the antibiotic in the stomach, and citrus juices, on the contrary, inhibit the inactivation of antibiotics, which, in turn, can lead to an overdose. Antibiotics are one of the few groups of drugs that are used irrationally and unjustifiably in 50% of cases. This often happens through the fault of the patients themselves, who prescribe them to themselves, their relatives and colleagues, copying previously heard treatment tactics. They prescribe them for acute respiratory viral infections (according to VTsIOM, 46% of Russians are confident that antibiotics in the fight against viruses are no less effective than in the fight against bacteria), for pain in the stomach and throat, as antipyretics and antitussives. They are often prescribed by pharmacists in pharmacies for the same indications. But since their discovery, antibiotics have remained one of the most important breakthroughs in medicine. Of course, if you use them correctly...
Macrolides
Slightly toxic drugs that have a bactericidal effect on:
- gram-positive bacteria (streptococci, staphylococci, mycobacteria);
- gram-negative bacilli (enterobacteriaceae, Helicobacter pylori, Haemophilus influenzae);
- intracellular microorganisms (moraxella, legionella, mycoplasma, chlamydia).
14-member:
| Representatives | Tradename | Method of application, price (rub.) |
| Clarithromycin | Klacid | Tablets: 0.5 g each. twice a day, taken for 2 weeks. 510-800 |
| Granules for preparing a suspension: to prepare the mixture, pour warm water up to the mark on the bottle, stir, take 2 times a day. 355-450 | ||
| Solution for infusion: 0.5 g. twice a day. 650-700 | ||
| Fromilid | Tablets: 0.5 g twice a day, taken for 2 weeks. 290-680 | |
| Clarithrosin | Tablets: 0.25 g each. twice a day, taken for 2 weeks. 100-150 | |
| Roxithromycin | RoxyHEXAL | Tablets: 0.15 g each. twice a day or 0.3 g. in one dose, course of treatment 10 days. 110-170 |
| Esparoxy | Tablets: 0.15 g each. twice a day 15 minutes before meals or 0.3 g. once, the course of administration is 10 days. 330-350 | |
| Rulid | Tablets: 0.15 g each. twice a day, course of treatment is 10 days. 1000-1400 | |
| Oleandomycin | Oleandomycin phosphate | Powder substance. Practically not used at present. 170-200 |
| Erythromycin | Erythromycin | Tablets: 0.2-0.4 g. four times a day before or after meals, washed down with water, course of administration is 7-10 days. 70-90 |
| Lyophilisate for preparing a solution for infusion: 0.2 g, diluted with a solvent, 3 times a day. The maximum course of treatment is 2 weeks. 550-590 | ||
| Eye ointment: place behind the lower eyelid three times a day, course of use is 14 days. 70-140 | ||
| External ointment: apply a small layer to the affected areas of the skin 2-3 times a day. 80-100 |
15-member:
| Representatives | Tradename | Method of application, price (rub.) |
| Azithromycin | Sumamed | Capsules: 0.5 g each. x 1 time per day before or 2 hours after meals. 450-550 |
| Powder for oral suspension: add 11 ml of water to the bottle, shake, take 1 time per day before or after meals. 220-570 | ||
| Tablets: 0.5 g each. x 1 time per day before or after meals. 250-580 | ||
| Azitral | Capsules: 0.25-0.5 g each. x 1 time per day before or after meals. 280-340 | |
| Azitrox | Capsules: 0.25-0.5 g each. x 1 time per day. 280-330 | |
| Powder for oral suspension: add 9.5 ml of water to the bottle, shake, orally 2 times a day. 130-370 |
16-member:
| Representatives | Tradename | Method of application, price (rub.) |
| Midecamycin | Macropen | Tablets: 0.4 g each. three times a day, course of administration for 2 weeks. 250-340 |
| Josamycin | Vilprafen | Tablets: 0.5 g each. twice a day, without chewing, with water. 530-620 |
| Vilprafen solutab | Tablets: 0.5 g each. x twice a day, without chewing or dissolved in 20 ml of water. 650-750 | |
| Spiramycin | Spiramycin-vero | Tablets: 2-3 tablets (3 million IU) in 2-3 doses per day. 220-1750 |
| Rovamycin | Tablets: 2-3 tablets (3 million IU) or 5-6 tablets (6-9 million IU) for 2-3 doses per day. 1010-1700 |