Penicillin antibiotics are β-lactam antibiotics. β-lactam antibiotics β-lactams, which are united by the presence of a β-lactam ring in their structure, include penicillins, cephalosporins, carbapen
ems and monobactams that have a bactericidal effect. The similarity of the chemical structure determines, firstly, the same mechanism of action of all β-lactams - inhibition of penicillin-binding proteins (PBPs), enzymes involved in the process of bacterial cell wall synthesis (under conditions of PBP inhibition, this process is disrupted, which entails lysis of the bacterial cell) , and, secondly, cross-allergy to them in some patients.
It is important that the cellular structures of bacteria, which are the target of the action of β-lactams, are absent in mammals, therefore, specific toxicity towards the macroorganism is not typical for these antibiotics.
Penicillins, cephalosporins and monobactams are sensitive to the hydrolyzing action of special enzymes - β-lactamases, produced by many bacteria. Carbapenems are characterized by significantly higher resistance to β-lactamases. Given their high clinical efficacy and low toxicity, β-lactam antibiotics have been the basis of antimicrobial chemotherapy for many years, occupying a leading place in the treatment of most bacterial infections.
Antibiotics of the penicillin group
Penicillins are the first antimicrobial drugs developed on the basis of biologically active substances produced by microorganisms. The ancestor of all penicillins, benzylpenicillin, was obtained in the early 40s. XX century. Its discovery marked a kind of revolutionary revolution in medicine, since, firstly, it transferred many bacterial infections from the category of inevitably lethal to potentially treatable, and secondly, it determined the fundamental direction on the basis of which many other antibacterial drugs were subsequently developed.
Currently, the group of penicillins includes more than ten antibiotics, which, depending on the sources of production, structural features and antimicrobial activity, are divided into several subgroups. At the same time, some antibiotics, primarily carboxypenicillins and ureidopenicillins, have lost their original meaning and are not used as single drugs.
Use during pregnancy
Penicillins migrate across the placental barrier, but despite this, there have been no documented facts that they cause complications in pregnant patients.
Based on their effects on the fetus, drugs in this group are classified as Category B by the FDA.
This means that in experiments on animals they did not show a negative effect on the fetus, did not cause congenital pathologies and mutations in the offspring, but controlled clinical studies were not conducted in pregnant patients. Only a doctor should select an antibiotic during pregnancy, taking into account the gestational age, the woman’s contraindications to starting therapy and its tolerability. In this case, the patient must be constantly under the supervision of a specialist who must monitor the condition of the mother and child.
Pregnant women may be prescribed natural and semi-synthetic penicillins, based on amoxicillin, ampicillin, and oxacillin.
General properties of penicillins
Antibacterial drugs from the penicillin group have the following properties:
- They have a bactericidal effect.
- They are well distributed in the body, penetrate into many organs, tissues and environments, with the exception of non-inflamed meninges, eyes, prostate, organs and tissues. Creates high concentrations in the lungs, kidneys, intestinal mucosa, reproductive organs, bones, pleural and peritoneal fluid.
- In small quantities they pass through the placenta and enter breast milk.
- They penetrate poorly through the BBB (with meningitis, permeability increases, and the concentration of penicillin in the cerebrospinal fluid is 5% of the serum level), the blood-ophthalmic barrier (BOB), and into the prostate gland.
- They are excreted by the kidneys, mainly through active excretion by the renal tubules.
- The half-life is 0.5 hours.
- The therapeutic level in the blood remains within 4-6 hours.
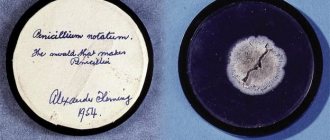
History of discovery
The history of the discovery of penicillin antibacterial agents dates back to the 30s of the 20th century, when scientist Alexander Fleming, who was studying bacterial infections, accidentally identified an area in which bacteria did not grow. As additional research showed, such a place in the bowl was the mold that usually covers stale bread.
As it turned out, this substance easily killed staphylococci. After additional research, the scientist was able to isolate penicillin in its pure form, which became the first antibacterial agent.
The principle of action of this substance is as follows: during bacterial cell division, to restore its own damaged membrane, these substances use elements called peptidoglycans. Penicillin does not allow this substance to form, which is why bacteria lose the ability not only to reproduce, but also to develop further, and are destroyed.
However, not everything went smoothly; after some time, bacterial cells began to actively produce an enzyme called beta-lactamase, which began to destroy beta-lactams, which form the basis of penicillins. To solve this problem, additional components were added to the composition of antibacterial agents, for example, clavulonic acid.
Side effects of penicillins
Allergic reactions (according to various sources, in 1-10% of cases): urticaria; rash; Quincke's edema; fever; eosinophilia; bronchospasm.
The most dangerous is anaphylactic shock, causing up to 10% mortality (in the USA, about 75% of deaths from anaphylactic shock are caused by the administration of penicillin).
Local irritating effect with intramuscular injection (pain, infiltrates).
Neurotoxicity: convulsions, which are more often observed in children, when using very high doses of penicillin, in patients with renal failure, when administering more than 10 thousand units endolumbarally.
Electrolyte imbalance - in patients with heart failure, when large doses of sodium salt are administered, edema may increase, and in case of hypertension, blood pressure (BP) may increase (1 million units contains 2.0 mmol of sodium).
Sensitization. Please be aware that the degree of sensitization to penicillin may vary over time in some people. In 78% of them, skin tests become negative after 10 years. Therefore, the statement about penicillin allergy as a lifelong clinical diagnosis is incorrect.
Prevention measures
Careful history taking, use of freshly prepared penicillin solutions, observation of the patient for 30 minutes after the first administration of penicillin, detection of hypersensitivity by skin testing.
Measures to help with the development of anaphylactic shock: ensuring airway patency (intubation if necessary), oxygen therapy, adrenaline, glucocorticoids.
It should be noted that with bronchial asthma and other allergic diseases, the risk of developing allergic reactions to penicillins (as well as to other antibiotics) is somewhat increased, and if they occur, they can be more severe. However, the prevailing point of view that penicillins should not be prescribed to persons with allergic diseases is erroneous.
Operating principle
The described active substance has a bactericidal and bacteriostatic effect on pathogens. The mechanism of the bactericidal scheme of action of drugs included in the penicillin type (series) is associated with damage to the cell walls (violation of the integrity of the structure) of infectious agents, which leads to the death of microorganisms.
The bacteriostatic principle of action on pathogens is characterized by temporary suppression of the ability of pathogenic organisms to reproduce.
The type of drug exposure is selected taking into account the severity of the disease.
Most penicillins in small doses affect microbes bacteriostatically. As the amount of the drug used increases, the effect changes to bactericidal. Only a doctor can select the specific dosage of a penicillin group medication; you cannot use antibiotics for treatment on your own.
Natural penicillin preparations
Natural penicillin preparations include the following:
- Benzylpenicillin;
- Benzylpenicillin sodium salt;
- Benzylpenicillin novocaine salt;
- Phenoxymethylpencillin;
- Ospen 750;
- Bicillin-1;
- Retarpen.
Phenoxymethylpenicillin
A natural penicillin preparation intended for oral administration. The spectrum of activity is practically no different from penicillin. Compared to penicillin, it is more acid-resistant. Bioavailability is 40-60% (slightly higher when taken on an empty stomach).
The drug does not create high concentrations in the blood: taking 0.5 g of phenoxymethylpenicillin orally approximately corresponds to administering 300 thousand units of penicillin intramuscularly. The half-life is about 1 hour.
Side effects
- Allergic reactions.
- Gastrointestinal tract (GIT) - pain or discomfort in the abdomen, nausea; less often vomiting, diarrhea.
Indications for use
- Streptococcal (GABHS) infections of mild to moderate severity: tonsillopharyngitis, skin and soft tissue infections.
- Year-round prevention of rheumatic fever.
- Prevention of pneumococcal infections in persons after splenectomy.
Benzathine phenoxymethylpenicillin
A derivative of phenoxymethylpenicillin. Compared to it, it is more stable in the gastrointestinal tract, absorbed faster, and better tolerated. Bioavailability is independent of food.
Indications for use
- Streptococcal (GABHS) infections of mild to moderate severity: tonsillopharyngitis, skin and soft tissue infections.
Holiday order and prices
A penicillin antibiotic can be purchased at a pharmacy only with a prescription. The price of medicines depends on the form of release, the manufacturer, and the specific pharmacy.
The approximate cost in rubles is as follows:
| City | Bicillin-3 1.2 million units | Ampicillin 250 mg 20 tablets. | Amoxicillin tablets 500 mg No. 20 produced by Biokhimik | Amoxicillin tablets, 0.25 g, produced by Dalkhimpharm OJSC, 20 pcs. |
| Moscow | 82 | 27 | 72 | 47 |
| Saint Petersburg | 94 | 27 | 76 | 49 |
| Kazan | 84 | 26 | 73 | 48 |
| Ekaterinburg | 79 | 26 | 79 | 46 |
Uncontrolled use of penicillins can lead to the growth of microorganisms insensitive to them and chronicity of the disease.
In the list of antibiotics, representatives of the penicillin series occupy the largest share. All of them are used strictly as prescribed by a doctor, as they have many contraindications and can cause negative reactions, including death.
Article design: Vladimir the Great
Long-acting penicillin preparations
Long-acting penicillin preparations, or so-called depot penicillins, include benzylpenicillin novocaine salt and benzathine benzyl penicillin , as well as combination preparations created on their basis.
Side effects of long-acting penicillin preparations
- Allergic reactions.
- Pain, infiltrates at the injection site.
- She (Hoigne) syndrome is ischemia and gangrene of the extremities due to accidental injection into an artery.
- Nicholau syndrome is an embolism of the blood vessels of the lungs and brain when injected into a vein.
Prevention of vascular complications: strict adherence to the insertion technique - intramuscularly into the upper outer quadrant of the buttock using a wide needle, with the patient in a horizontal position. Before insertion, it is necessary to pull the syringe plunger towards you to make sure that the needle is not in the vessel.
Indications for use
- Infections caused by microorganisms highly sensitive to penicillin: streptococcal (GABHS) tonsillopharyngitis; syphilis (except neurosyphilis).
- Prevention of anthrax after contact with spores (benzylpenicillin novocaine salt).
- Year-round prevention of rheumatic fever.
- Prevention of diphtheria, streptococcal cellulitis.
Benzylpenicillin novocaine salt
With intramuscular administration, the therapeutic concentration in the blood is maintained for 12-24 hours, but it is lower than with the introduction of an equivalent dose of benzylpenicillin sodium salt. The half-life is 6 hours.
It has a local anesthetic effect and is contraindicated if you are allergic to procaine (Novocaine). In case of overdose, mental disorders are possible.
Benzathine Benzylpenicillin
It acts longer than benzylpenicillin novocaine salt, up to 3-4 weeks. After intramuscular administration, peak concentrations are observed after 24 hours in children and after 48 hours in adults. The half-life is several days.
Pharmacokinetic studies of domestic drugs benzathine benzylpenicillin, conducted at the State Research Center for Antibiotics, showed that when used, the therapeutic concentration in the blood serum remains for no more than 14 days, which requires their more frequent administration than the foreign analogue, Retarpen.
Antibacterial agents for sinusitis
The disease has characteristic symptoms; treatment with antibiotics can reduce the severity of the symptom complex and speed up the patient’s recovery. Treatment of sinusitis with antibiotics is necessary for the bacterial form of the pathology. In the chronic form of the disease, regular use of medications helps prevent the spread of infection to healthy areas. In this case, medications are prescribed etiotropically, with preliminary bacterial culture.
There are several forms of medications:
- suspensions;
- pills;
- capsules;
- injection.
Antibiotic nasal drops and sprays, ointments, and creams for external use are available for sale. Almost all antibacterial medications are able to penetrate the mucous membranes.
Combination penicillin preparations
Bicillin-3, Bicillin-5.
Isoxazolylpenicillins (antistaphylococcal penicillins)
Isoxazolylpenicillin drug – Oxacillin.
The first isoxazolylpenicillin with antistaphylococcal activity was methicillin, which was later discontinued due to lack of advantages over newer analogues and nephrotoxicity.
Currently, the main drug of this group in Russia is oxacillin. Nafcillin, cloxacillin, dicloxacillin and flucloxacillin are also used abroad.
Oxacillin
Activity spectrum Oxacillin is resistant to penicillinase, which is produced by more than 90% of S. aureus strains. Therefore, they are active against penicillin-resistant S. aureus (PRSA) and a number of strains of S. epidermidis resistant to natural penicillins, amino-, carboxy- and ureidopenicillins. This is the main clinical significance of this drug.
At the same time, oxacillin is significantly less active against streptococci (including S. pneumoniae). It has virtually no effect on most other penicillin-sensitive microorganisms, including gonococci and enterococci.
One of the serious problems is the spread of strains (especially nosocomial) of S. aureus that are resistant to isoxazolylpenicillins and, based on the name of the first of them, received the abbreviation MRSA (raeticillin-resistant S. aureus). In fact, they are multidrug-resistant, since they are resistant not only to all penicillins, but also to cephalosporins, macrolides, tetracyclines, lincosamides, carbapenems, fluoroquinolones and other antibiotics.
Side effects
- Allergic reactions.
- Gastrointestinal tract - abdominal pain, nausea, vomiting, diarrhea.
- Moderate hepatotoxicity - increased activity of liver transaminases, especially when administered in high doses (more than 6 g/day); As a rule, it is asymptomatic, but can sometimes be accompanied by fever, nausea, vomiting, and eosinophilia (liver biopsy shows signs of nonspecific hepatitis).
- Decreased hemoglobin level, neutropenia.
- Transient hematuria in children.
Indications for use
Confirmed or suspected staphylococcal infections of various localizations (with sensitivity to oxacillin or a slight risk of spreading methicillin resistance):
- skin and soft tissue infections;
- bone and joint infections;
- pneumonia;
- infective endocarditis;
- meningitis;
- sepsis.
Aminopenicillins
Aminopencillins include ampicillin and amoxicillin . Compared to natural penicillins and isoxazolylpenicillins, their antimicrobial spectrum is expanded to include some gram-negative bacteria of the family Enterobacteriaceae and H. influenzae.
Ampicillin
Differences from penicillin in the spectrum of antibacterial activity
- It acts on a number of gram(-) bacteria: E. coli, P. mirabilis, salmonella, shigella (the latter are resistant in many cases), N. influenzae (strains that do not produce β-lactamases).
- More active against enterococci (E. faecalis) and listeria.
- Slightly less active against streptococci (GABHS, S. pneumoniae), spirochetes, and anaerobes.
Ampicillin has no effect on gram-negative pathogens of nosocomial infections, such as Pseudomonas aeruginosa (P. aeruginosa), Klebsiella, Serration, Enterobacter, Acinetobacter, etc.
It is destroyed by staphylococcal penicillinase, therefore inactive against most staphylococci.
Side effects
- Allergic reactions.
- Gastrointestinal disorders - abdominal pain, nausea, vomiting, most often diarrhea.
- “Ampicillin” rash (in 5-10% of patients), according to most experts, is not associated with an allergy to penicillin.
The rash is maculopapular in nature, is not accompanied by itching and may go away without stopping the drug. Risk factors: infectious mononucleosis (rash occurs in 75-100% of cases), cytomegaly, chronic lymphocytic leukemia.
Indications for use
- Acute bacterial infections of the upper respiratory tract (otitis media, rhinosinusitis - if necessary, parenteral administration).
- Community-acquired pneumonia (if parenteral administration is necessary).
- Urinary tract infections (UTI) - cystitis, pyelonephritis (not recommended for empirical therapy due to the high level of pathogen resistance).
- Intestinal infections (salmonellosis, shigellosis).
- Meningitis.
- Infectious endocarditis.
- Leptospirosis.
Warnings and Precautions
Ampicillin can only be dissolved in water for injection or 0.9% sodium chloride solution. Freshly prepared solutions must be used. When stored for more than 1 hour, the activity of the drug sharply decreases.
Amoxicillin
It is an ampicillin derivative with improved pharmacokinetics.
Spectrum of antibacterial activity
According to the antimicrobial spectrum, amoxicillin is close to ampicillin (the microflora exhibits cross-resistance to both drugs).
- amoxicillin is the most active among all oral penicillins and cephalosporins against S. pneumoniae, including pneumococci with intermediate levels of resistance to penicillin;
- has a slightly stronger effect on E. faecalis than ampicillin;
- clinically ineffective against Salmonella and Shigella, regardless of the results of in vitro susceptibility testing;
- highly active in vitro and in vivo against H. pylori.
Similar to ampicillin, amoxicillin is destroyed by β-lactamases.
Side effects
- Allergic reactions.
- "Ampicillin" rash.
- Gastrointestinal tract - mostly moderate abdominal discomfort, nausea; diarrhea is observed much less frequently than when using ampicillin.
Indications for use
- Upper respiratory tract infections - acute otitis media, acute rhinosinusitis.
- Lower respiratory tract infections - exacerbation of chronic obstructive pulmonary disease (COPD), community-acquired pneumonia.
- Urinary tract infections - cystitis, pyelonephritis (not recommended for empirical therapy due to the high level of pathogen resistance).
- Eradication of H. pylori (in combination with antisecretory drugs and other antibiotics).
- Tick-borne borreliosis (Lyme disease).
- Prevention of infective endocarditis.
- Prevention of anthrax (in pregnant women and children).
Warnings
Cannot be used in the treatment of shigellosis and salmonellosis. Amoxicillin preparations - Ampicillin-AKOS, Ampicillin-Ferein, Ampicillin sodium salt, Amoxicillin, Amoxicillin Sandoz, Amosin, Ospamox, Flemoxin Solutab, Hiconcil.
Indications for use
An antibiotic of the penicellin series, regardless of its form, causes death:
- streptococci;
- staphylococci;
- enterococci;
- listeria;
- Helicobacter pylori;
- Neisseria;
- clostridium;
- corynebacteria.
They are recommended for bacterial infections caused by pathogenic agents sensitive to them, including diseases such as:
- inflammation of the paranasal sinuses, bronchi and lungs;
- angina;
- otitis;
- blood poisoning;
- syphilis;
- gonorrhea;
- cystitis;
- pyelonephritis;
- salmonellosis;
- peptic ulcer of the digestive tract associated with Helicobacter pylori (penicillins are prescribed in combination with other antimicrobial agents);
- infections of soft tissues and skin, including erysipelas, infected wounds and burns;
- inflammation of the meninges;
- scarlet fever;
- Lyme disease;
- endocarditis;
- anaerobic infections such as tetanus and gas gangrene;
- anthrax;
- osteomyelitis.
Penicillins are used to prevent bacterial complications during surgery, as well as exacerbation of rheumatism.
Carboxypenicillins
Carboxypenicillins include carbenicillin (discontinued and no longer in use) and ticarcillin (part of the ticarcillin/clavulanate combination drug).
Their main advantage for a long time was their activity against P. aeruginosa, as well as some gram-negative bacteria resistant to aminopenicillins (Enterobacter, Proteus, Morganella, etc.). However, to date, carboxypenicillins have practically lost their “anti-pseudomonas” value due to the high level of resistance of Pseudomonas aeruginosa and many other microorganisms to them, as well as poor tolerability.
They have the greatest neurotoxicity among penicillins and can cause platelet aggregation disorders, thrombocytopenia, and electrolyte imbalances—hypernatremia, hypokalemia.
Inhibitor-protected penicillins
The main mechanism for the development of bacterial resistance to β-lactam antibiotics is their production of special enzymes, β-lactamases, which destroy the β-lactam ring, the most important structural element of these drugs that ensures their bactericidal effect. This protective mechanism turns out to be one of the leading ones for such clinically important pathogens as S. aureus, H. influenzae, M. catarrhalis, K. pneumoniae, B. fragilis, and many others.
Taking a simplified approach to the systematization of β-lactamases produced by microorganisms, they can be divided into several types, depending on the direction of action:
1) penicillinases that destroy penicillins;
2) cephalosporinases that destroy cephalosporins of the first and second generations;
3) extended spectrum β-lactamases (ESBLs), combining the properties of the first two types and, in addition, destroying cephalosporins of the III and IV generations;
4) metallo-β-lactamases, which destroy almost all β-lactams (except monobactams).
In order to overcome this resistance mechanism, compounds that inactivate β-lactamases were obtained: clavulanic acid (clavulanate), sulbactam and tazobactam.
On this basis, combination preparations have been created containing a penicillin antibiotic (ampicillin, amoxicillin, piperacillin, ticarcillin) and one of the β-lactamase inhibitors.
Such drugs are called inhibitor-protected penicillins.
As a result of the combination of penicillins with β-lactamase inhibitors, the natural (primary) activity of penicillins against many staphylococci (except MRSA), gram-negative bacteria, non-spore-forming anaerobes is restored, and their antimicrobial spectrum is expanded due to a number of gram-negative bacteria (Klebsiella, etc.) with natural resistance to penicillins.
It should be emphasized that β-lactamase inhibitors overcome only one of the bacterial resistance mechanisms. Therefore, for example, tazobactam cannot increase the sensitivity of P. aeruginosa to piperacillin, since resistance in this case is caused by a decrease in the permeability of the outer membrane of the microbial cell to β-lactams.
Amoxicillin+clavulanate
The drug consists of amoxicillin and potassium clavulanate. The ratio of components in preparations for oral administration ranges from 2:1, 4:1 and 8:1, and for parenteral administration - 5:1. Clavulanic acid, used as a potassium salt, is one of the most powerful inhibitors of microbial β-lactamases. Therefore, amoxicillin in combination with clavulanate is not destroyed by β-lactamases, which significantly expands the spectrum of its activity.
Spectrum of antibacterial activity
Amoxicillin + clavulanate acts on all microorganisms sensitive to amoxicillin. Additionally, unlike amoxicillin:
- has higher antistaphylococcal activity: acts on PRSA and some strains of S. epidermidis;
- acts on enterococci producing (3-lactamases;
- active against gram(-) flora producing (3-lactamase (N. influ enzae, M. catarrhalis, N. gonorrhoeae, E. coli, Proteus spp., Klebsiella spp., etc.), except for ESBL producers;
- has high antianaerobic activity (including B. fragilis). Does not affect gram(-) bacteria resistant to aminopenicillins: P. aeruginosa, Enterobacter, Citrobacter, Serration, Providence, Morganella.
Side effects
Like Amoxicillin. In addition, due to the presence of clavulanate, in rare cases (usually in older people), hepatotoxic reactions (increased transaminase activity, fever, nausea, vomiting) are possible.
Indications for use
- Bacterial infections of the upper respiratory tract (acute and chronic rhinosinusitis, acute otitis media, epiglottitis).
- Bacterial infections of the lower respiratory tract (exacerbation of COPD, community-acquired pneumonia).
- Biliary tract infections (acute cholecystitis, cholangitis).
- Urinary tract infections (acute pyelonephritis, cystitis).
- Intra-abdominal infections.
- Infections of the pelvic organs.
- Skin and soft tissue infections (including wound infections after bites).
- Bone and joint infections.
- Perioperative antibiotic prophylaxis.
Amoxicillin+sulbactam
The drug consists of amoxicillin and sulbactam in ratios of 1:1 and 5:1 for oral administration and 2:1 for parenteral administration. The spectrum of activity is close to amoxicillin + clavulanate. Sulbactam, in addition to inhibiting β-lactamases, exhibits moderate activity against Neisseria spp., M. catarrhalis, Acinetobacter spp. Side effects
Same as Amoxicillin.
Indications for use
- Bacterial infections of the upper respiratory tract (acute and chronic rhinosinusitis, acute otitis media, epiglottitis).
- Bacterial infections of the respiratory tract (exacerbation of COPD, community-acquired pneumonia).
- Infections of the gallbladder (acute cholecystitis, cholangitis).
- UTI infections (acute pyelonephritis, cystitis).
- Intra-abdominal infections.
- Infections of the pelvic organs.
- Skin and soft tissue infections (including wound infections after bites).
- Bone and joint infections.
- Perioperative antibiotic prophylaxis.
It has an advantage over amoxicillin + clavulanate for infections caused by Acinetobacter.
Ampicillin+sulbactam
The drug consists of ampicillin and sulbactam in a ratio of 2:1. The prodrug sultamicillin, which is a compound of ampicillin and sulbactam, is intended for oral administration. During absorption, hydrolysis of sultamicillin occurs, and the bioavailability of ampicillin and sulbactam exceeds that when taking an equivalent dose of regular ampicillin.
Ampicillin + sulbactam is similar in most parameters to amoxicillin + clavulanate and amoxicillin + sulbactam.
Indications for use
- Bacterial infections of the upper respiratory tract (acute and chronic rhinosinusitis, acute otitis media, epiglottitis).
- Bacterial infections of the respiratory tract (exacerbation of COPD, community-acquired pneumonia).
- Infections of the gallbladder (acute cholecystitis, cholangitis).
- Infections of the bladder (acute pyelonephritis, cystitis).
- Intra-abdominal infections.
- Infections of the pelvic organs.
- Skin and soft tissue infections (including wound infections after bites).
- Bone and joint infections.
- Perioperative antibiotic prophylaxis.
It has an advantage over amoxicillin + clavulanate for infections caused by Acinetobacter.
Warning
When administered intramuscularly, the drug should be diluted with a 1% lidocaine solution.
Ticarcillin+clavulanate
A combination of carboxypenicillin ticarcillin with clavulanate in a ratio of 30:1. Unlike inhibitor-protected aminopenicillins, it acts on P. aeruginosa (but many strains are resistant) and surpasses them in activity against nosocomial strains of enterobacteria.
Spectrum of antibacterial activity
- Gram-positive cocci: staphylococci (including PRSA), streptococci, enterococci (but inferior in activity to inhibitor-protected aminopenicillins).
- Gram-negative rods: representatives of the family Enterobacteriaceae (E. coli, Klebsiella spp., Proteus spp., Enterobacter spp., Serratia spp., C. diversus, etc.); P. aeruginosa (but not superior to ticarcillin); non-fermenting bacteria - S. maltophilia (superior to other β-lactams in activity).
- Anaerobes: spore-forming and non-spore-forming, including B. fragilis.
Side effects
- Allergic reactions.
- Neurotoxicity (tremor, seizures).
- Electrolyte disturbances (hypernatremia, hypokalemia - especially in patients with heart failure).
- Impaired platelet aggregation.
Indications for use
Severe, predominantly nosocomial infections of various locations:
- lower respiratory tract infections (pneumonia, lung abscess, pleural empyema);
- complicated urinary tract infections;
- intra-abdominal infections;
- pelvic organ infections;
- skin and soft tissue infections;
- bone and joint infections;
- sepsis.
Piperacillin+tazobactam
Combination of ureidopenicillin piperacillin with tazobactam in a ratio of 8:1. Tazobactam is superior to sulbactam in terms of β-lactamase inhibition and is approximately equivalent to clavulanate. Piperacillin + tazobactam is considered the most powerful inhibitor-protected penicillin.
Spectrum of antibacterial activity
- Gram-positive cocci: staphylococci (including PRSA), streptococci, enterococci.
- Gram-negative rods: representatives of the family Enterobacteriaceae (E. coli, Klebsiella spp., Proteus spp., Enterobacter spp., Serratia spp., C. diversus, etc.); P. aeruginosa (but not superior to piperacillin); non-fermenting bacteria - S. maltophilia.
- Anaerobes: spore-forming and non-spore-forming, including B. fra-ilis.
Side effects
The same as Ticarcillin + clavulanate.
Indications for use
Severe, predominantly nosocomial infections of various localizations caused by multidrug-resistant and mixed (aerobic-anaerobic) microflora:
- lower respiratory tract infections (pneumonia, lung abscess, pleural empyema);
- complicated urinary tract infections;
- intra-abdominal infections;
- pelvic organ infections;
- skin and soft tissue infections;
- bone and joint infections;
- sepsis.
Classification
There are 4 groups of penicillins.
The first group includes:
- Natural antimicrobial agents that are destroyed by penicillinases, so they are characterized by a narrow spectrum of antibacterial activity. These are medications such as benzylpenicillin and phenoxymethylpenicillin.
- Semi-synthetic antibiotics such as methicillin, nafcillin, oxacillin. They are not destroyed by penicillinases, therefore they have a wider spectrum of antimicrobial activity.
- Aminopenicillins, such as ampicillin, amoxicillin. They are characterized by a wide spectrum of action.
The second and third groups include carboxypenicillins. These are drugs such as Ticarcillin and Carbenicillin. The fourth generation includes amidinopenicillins and ureidopenicillins, which have a wide antibacterial spectrum.
Inhibitor-protected penicillins that are not destroyed by β-lactamases, such as Amoxiclav, Augmentin, are often prescribed.
Preparations of inhibitor-protected penicillins
(Amoxicillin + clavulanate) - Amocombe, Amoxiclav, Amoxivan, Arlet, Augmentin, Bactoclav, Betaclave, Verclave, Klamosar, Medoclav, Panclave 2X, Rapiclav, Fibell, Flemoclav Solutab, Foraclave, Ecoclave.
(Amoxicillin + sulbactam) - Trifamox IBL, Trifamox IBL DUO.
(Ampicillin + sulbactam) - Ampisid, Libaccil, Sultasin.
(Ticarcillin + clavulanate) – Timentin.
(Piperacillin + tazobactam) - Santaz, Tazocin, Tazrobida, Tacillin J.