Lamivudine is an antiviral drug that has an inhibitory effect on the replication process of HIV strains. It stops the vital activity of the pathogen by blocking the DNA chain during reverse transcription of the immunodeficiency virus. The product is sold under several trade names. Lamivudine may help with hepatitis B.
Having penetrated into the affected cells, Lamivudine is converted into active 5-triphosphate. It is excreted from the body after 19 hours as part of urine. The drug does not affect metabolic metabolism, the structure of mitochondrial and nuclear DNA. The maximum concentration of the active substance is recorded 1 hour after taking Lamivudine, its bioavailability is 85%. The medicine is often included in a combination treatment complex along with Zidovudine and other nucleotide-type inhibitors.
Lamivudine
If Lamivudine is taken with food, bioavailability will decrease markedly. The absorption value will not change. Therefore, when choosing this order of administration, there is no need to adjust the daily intake. Lamivudine penetrates the placental barrier and quickly binds to plasma proteins. HIV cannot be prevented by vaccination. The virus is highly resistant and variable, so its resistance to Lamivudine can develop in a short time. After this, the medicine will not be as effective.
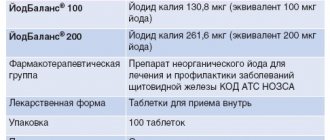
Compound
One film-coated tablet contains:
- active ingredient – lamivudine 150 mg;
- excipients: microcrystalline cellulose – 123.50 mg; sodium carboxymethyl starch – 5.00 mg, magnesium stearate – 1.50 mg;
- shell composition: opadry white (hypromellose, titanium dioxide, macrogol-4000, polysorbate-80) 7 mg.
pharmachologic effect
- Antiviral agent, nucleoside reverse transcriptase inhibitor. Penetrating into cells, it is metabolized to 5-triphosphate, which inhibits HIV reverse transcriptase, which leads to inhibition of viral replication.
- It is active against strains resistant to zidovudine, and when used in combination with it, it slows down the development of viral resistance to zidovudine (in patients who have not previously been treated).
- It has a higher therapeutic index in vitro than zidovudine (weaker than zidovudine, it inhibits bone marrow progenitor cells, and also has a less pronounced cytotoxic effect on peripheral blood lymphocytes, lymphocytic and monocyte-macrophage cell lines).
- It has little effect on the metabolism of cellular deoxynucleotides and the DNA content in the mitochondria of undamaged cells.
- Lamivudine is highly active against hepatitis B virus (HBV) in all cell lines tested and in all experimentally infected animals.
Instructions for use
The prescription of Lamivudine is allowed only by a specialist with experience in treating HIV infection.
Lamivudine is administered orally regardless of food intake (before, during or after meals).
To ensure accurate dosing of the drug, it is recommended to swallow the tablets completely without dividing them.
For the treatment of children and those patients who have difficulty swallowing tablets, another dosage form (oral solution) is intended.
Patient categories:
- Adults and adolescents weighing more than 30 kg:
The recommended dose is 300 mg per day. You can prescribe 150 mg 2 times a day or 300 mg per day in one dose.
- Elderly patients:
Currently, there is insufficient data on the pharmacokinetics of lamivudine in this category of patients, however, special attention should be paid to this category of patients due to the age-related decrease in renal excretory function and changes in blood counts.
- Patients with impaired renal function:
In patients with moderate to severe renal impairment, plasma concentrations are increased due to decreased clearance of lamivudine. Therefore, with a creatinine clearance of 30–50 ml/min, the dose of the drug is 150 mg once a day.
In adolescents weighing more than 30 kg with impaired renal function, the same dose reduction regimen is recommended depending on the creatinine clearance value as in adults. In case of renal failure and creatinine clearance <30 ml/min, it is necessary to use another dosage form - an oral solution.
Lamivudine
The use of the drug as monotherapy is not recommended.
HIV transmission
Patients should be warned that treatment with antiretroviral drugs does not prevent the risk of transmitting HIV to others through sex or blood transfusions. Therefore, patients should take appropriate precautions.
Opportunistic infections
Patients receiving lamivudine or other antiretroviral drugs may develop opportunistic infections or other complications of HIV infection, so patients should be closely monitored by a physician experienced in treating patients with HIV-associated diseases.
Renal dysfunction
In patients with moderate to severe dysfunction, the concentration of the drug in the blood plasma is increased due to decreased clearance of the drug, so dose adjustment is required.
Triple therapy with nucleoside analogues
A high incidence of lack of virological response and the emergence of resistance at an early stage has been reported when the drug is co-administered with tenofovir disoproxil fumarate and abacavir, as well as with tenofovir disoproxil fumarate and didanosine in a once-daily dosing regimen.
Pancreatitis
Rare cases of pancreatitis have been described in patients taking the drug. However, it has not been established whether this complication is caused by medications or the underlying disease - HIV infection. Treatment with the drug should be stopped immediately if clinical symptoms or laboratory data indicating the development of pancreatitis (abdominal pain, nausea, vomiting or increased levels of biochemical markers) appear. You should stop taking the drug until the diagnosis of pancreatitis is excluded.
Lactic acidosis and severe hepatomegaly with steatosis
There are reports of the development in patients (mainly women) of lactic acidosis, severe hepatomegaly with steatosis, including death, due to antiretroviral therapy with nucleoside analogues in the form of individual drugs, including the drug and its combinations.
Clinical signs of developing lactic acidosis are: general weakness, anorexia, rapid unexplained weight loss, gastrointestinal and respiratory disorders (shortness of breath and tachypnea).
Caution should be exercised when using the drug to treat any patient (especially obese women) with hepatomegaly, hepatitis, or other known risk factors for liver disease and hepatic steatosis (including use of certain medications and alcohol use). Patients coinfected with hepatitis C and patients receiving treatment with alpha interferon and ribavirin may be at particular risk. The use of the drug should be discontinued if clinical or laboratory signs of lactic acidosis or hepatotoxicity (which include hepatomegaly and steatosis) appear, even in the absence of a significant increase in aminotransferase activity.
Lipodystrophy
Some patients receiving combination antiretroviral therapy may experience redistribution and/or accumulation of subcutaneous fat, including central obesity, dorsocervical fat deposition ('buffalo hump'), decreased subcutaneous fat on the face and extremities, and breast enlargement , increasing the concentration of lipids in the serum and the concentration of glucose in the blood, both separately and together.
Although all drugs in the classes of protease inhibitors and nucleoside reverse transcriptase inhibitors can cause one or more of the above adverse reactions associated with a common syndrome often called lipodystrophy, accumulating evidence suggests that there are differences among individual members of these drug classes in the ability to cause these adverse reactions. reactions.
It should also be noted that lipodystrophy syndrome has a multifactorial etiology: for example, the stage of HIV infection, advanced age and duration of antiretroviral therapy play an important, possibly synergistic role in the development of this complication.
The long-term consequences of these adverse events are still unknown.
During the clinical examination, attention should be paid to signs of redistribution of subcutaneous fat. Serum lipid concentrations and blood glucose concentrations should be closely monitored. If lipid metabolism is disrupted, appropriate treatment is prescribed.
Immune reconstitution syndrome
If HIV-infected patients with severe immunodeficiency have asymptomatic opportunistic infections or their residual effects at the time of initiation of antiretroviral therapy, such therapy may lead to increased symptoms of opportunistic infections or other serious consequences. These reactions usually occur within the first weeks or months after starting antiretroviral therapy. Typical examples are cytomegalovirus retinitis, generalized or focal infection caused by mycobacteria, and pneumonia caused by Pneumocystis jiroveci (P. carinii). The appearance of any symptoms of inflammation requires immediate examination and, if necessary, treatment.
Autoimmune diseases (such as Graves' disease, polymyositis and Guillain-Barré syndrome) have been observed in the setting of immune reconstitution, but the timing of initial manifestations varies and the disease can occur many months after the start of therapy and have an atypical course.
Co-infection with HIV and viral hepatitis B or C.
Patients with chronic hepatitis B or C who are receiving combination antiretroviral therapy are at increased risk of developing severe and potentially fatal liver side effects. In case of combined use with other antiviral drugs for the treatment of hepatitis B and C, you should follow the appropriate instructions for the medical use of these drugs.
In vitro studies have shown that ribavirin can reduce the phosphorylation of pyrimidine nucleoside analogues such as the drug. Although data on the pharmacokinetic interaction of ribavirin with the drug are not available, cases of liver decompensation (sometimes fatal) have been reported in patients infected with HIV-1 with concomitant hepatitis C receiving antiretroviral therapy for the treatment of HIV-1 and alpha-interferon with and without ribavirin. ribavirin. Patients receiving the drug and interferon alpha with and without ribavirin should be closely monitored for drug interaction toxicity, particularly hepatic decompensation, neutropenia, and anemia. If clinical toxicities, especially hepatic decompensation, worsen, reduce doses or discontinue interferon alfa, ribavirin, or both.
Clinical studies and post-marketing surveillance data suggest that some patients with concomitant hepatitis B virus (HBV) may experience clinical or laboratory evidence of relapse of hepatitis after discontinuation of the drug, which may have more severe consequences in patients with uncompensated liver disease . After completing drug therapy in patients with co-infection caused by HIV and hepatitis B virus, it is necessary to monitor biochemical indicators of liver function and markers of hepatitis B virus replication.
Mitochondrial dysfunction
In vitro and in vivo studies have shown that nucleoside and nucleotide analogues are capable of causing varying degrees of mitochondrial damage. Cases of mitochondrial dysfunction have been reported in HIV-negative children receiving nucleoside analogues in utero and/or after birth. The main adverse reactions were hematological disorders (anemia, neutropenia), metabolic disorders (hyperlactatemia, hyperlipasemia). These adverse reactions are often transient. Some late-onset neurological disorders (increased muscle tone, seizures, behavioral disturbances) have been reported. Whether these neurological disorders are transient or permanent is currently unknown. Any child, even HIV-negative, exposed in utero to nucleoside and nucleotide analogues should undergo clinical and laboratory evaluation to rule out mitochondrial dysfunction if signs or symptoms are detected. These data do not change current national recommendations for the use of antiretroviral therapy in pregnant women to prevent vertical transmission of HIV infection.
Liver diseases
Patients with pre-existing liver dysfunction, including active chronic hepatitis, have an increased incidence of liver dysfunction during combination antiretroviral therapy and should be monitored according to established practice. Consideration should be given to suspending or discontinuing treatment if worsening liver disease occurs in such patients.
Osteonecrosis
Despite the fact that the etiology of this disease is multifactorial (including the use of glucocorticosteroids, alcohol consumption, severe immunosuppression, high body mass index), cases of osteonecrosis most often occurred in patients in the late stages of HIV infection and/or those taking combination antiretroviral therapy for a long time. Patients should consult a doctor if they experience joint pain and stiffness or difficulty moving.
Prevention after possible HIV infection
According to international recommendations, if infection is likely through the blood of an HIV-infected person, for example, through an injection needle), it is necessary to urgently (within 1-2 hours from the moment of infection) prescribe combination therapy with zidovudine and lamivudine. In case of a high risk of infection, a drug from the group of protease inhibitors should be included in the antiretroviral therapy regimen. Prophylactic treatment is recommended for 4 weeks. There is insufficient data on the effectiveness of preventive treatment after accidental HIV infection, and no controlled studies have been conducted.
Despite the rapid initiation of treatment with antiretroviral drugs, the possibility of seroconversion cannot be excluded.
Impact on the ability to drive vehicles, operate machinery and engage in other activities that require increased concentration
No special studies have been conducted on the effect of the drug on the ability to drive vehicles and operate machinery. However, based on the pharmacological properties of the drug, such an effect is unlikely. However, when assessing a patient’s ability to drive vehicles or perform work that requires increased attention and speed of psychomotor reactions, one should take into account his general condition, as well as the nature of adverse reactions.
Prescription during pregnancy and lactation
There is currently insufficient data on the safety of lamivudine during pregnancy. Studies have shown that lamivudine crosses the placenta.
Lamivudine should be used during pregnancy only if the expected benefit to the mother outweighs the potential risk to the fetus.
Although results from animal experiments cannot always be extrapolated to humans, data from studies in rabbits suggest a possible risk of spontaneous abortion in early pregnancy.
In newborns and children under 1 year of age, whose mothers took drugs from the group of nucleoside reverse transcriptase inhibitors during pregnancy and childbirth, cases of a slight transient increase in the concentration of lactic acid in the serum, apparently due to mitochondrial dysfunction, have been described.
The clinical significance of transient increases in serum lactic acid concentrations has not been established. In addition, very rare cases of developmental delay, seizures and other neurological disorders have been reported. However, the connection of these complications with the use of nucleoside reverse transcriptase inhibitors during pregnancy and its effect on postnatal development has not been proven.
Therefore, HIV-infected women are still advised to take antiretroviral drugs during pregnancy to prevent vertical transmission of HIV.
According to experts, all HIV-infected women should avoid breastfeeding if possible to avoid transmitting the virus to the baby through breast milk. After oral administration, lamivudine is excreted in breast milk; Moreover, its concentration in breast milk is practically no different from its concentration in serum (1-8 μg/ml).
Because HIV and lamivudine pass into breast milk, women taking lamivudine are not recommended to breastfeed.
Release form
Lamivudine is available in tablet form. The pills are packaged in blister packs. They are made from varnished aluminum foil and polyvinyl chloride film. One blister can contain from 10 to 20 tablets. After their placement, the plates are laid out in cardboard packs (from 2 to 6 blisters per package).
Lamivudine must be accompanied by instructions for use. The medication is kept in a place inaccessible to children and pets. The air temperature should not exceed +25 degrees Celsius. The shelf life of the drug is 2 years. Lamivudine can be purchased with a doctor's prescription from a hospital pharmacy.
Drug interactions
Interaction studies have been conducted in adult patients only:
- The likelihood of metabolic interaction of lamivudine with other drugs is extremely low, since lamivudine is very poorly metabolized, binds to plasma proteins to a small extent and is excreted primarily by the kidneys unchanged.
- Lamivudine is excreted from the body primarily by active tubular secretion through the organic cation transport system. The possibility of interaction of lamivudine with drugs that have the same elimination mechanism, for example trimethoprim, should be taken into account. Other drugs (eg, ranitidine, cimetidine) are only partially eliminated by this mechanism and do not interact with lamivudine. Drugs that are eliminated primarily by active renal secretion via the organic anion transport system or by glomerular filtration do not appear to have clinically significant interactions with lamivudine.
- Zidovudine. With simultaneous use of lamivudine and zidovudine, a moderate increase in plasma zidovudine concentrations is observed. Zidovudine does not affect the pharmacokinetics of lamivudine.
- Trimethoprim/sulfamethoxazole . Concomitant use of trimethoprim/sulfamethoxazole (co-trimoxazole) at a dose of 160/800 mg increases the plasma concentration of lamivudine by approximately 40% (due to interaction with trimethoprim). However, in the absence of renal impairment, a dose reduction of lamivudine is not required. Lamivudine does not affect the pharmacokinetics of trimethoprim and sulfamethoxazole. The simultaneous use of lamivudine with high doses of co-trimoxazole, prescribed for the treatment of Pneumocystis pneumonia and toxoplasmosis, is not recommended.
- Zalcitabine. When administered concomitantly with lamivudine and zalcitabine, lamivudine may inhibit intracellular phosphorylation of the latter. Therefore, this combination of drugs is not recommended.
- Cladribine. When administered concomitantly with lamivudine and cladribine, lamivudine may inhibit the intracellular phosphorylation of cladribine. Therefore, this combination of drugs is not recommended.
- Interferon and ribavirin . There is no data on possible pharmacokinetic and pharmacodynamic interactions when ribavirin and lamivudine are co-administered, however, fatal cases of liver failure have been reported in patients with co-infection (HIV and hepatitis C) receiving antiretroviral therapy together with interferon alfa and ribavirin.
- Emtricitabine. When used concomitantly, lamivudine may slow down the intracellular phosphorylation of emtricitabine. In addition, the mechanism of resistance to both lamivudine and emtricitabine is associated with a mutation in the same codon of the reverse transcriptase gene (M184V), and therefore the therapeutic effectiveness of these drugs in combination therapy may be limited. The use of lamivudine in combination with emtricitabine or fixed-dose combinations containing emtricitabine is not recommended.
Special instructions for the use of Lamivudine
The use of lamivudine does not prevent the possibility of infection through sexual contact or through blood. There is no experience with the use of lamivudine in children under 3 months of age. Despite the lack of direct indications of teratogenic effects and changes in reproductive function, lamivudine should be prescribed to pregnant women only after analyzing the expected effect for the woman and the risk to the fetus. If it is necessary to use lamivudine during lactation, breastfeeding should be discontinued. In children with impaired renal function, it is recommended to adjust the dosage regimen in the same proportions as in adults. Given that lamivudine is excreted almost exclusively by the kidneys, no dose adjustment is required in persons with impaired liver function. However, lamivudine should be used with caution in patients with liver cirrhosis caused by the hepatitis B virus, given the risk of hepatitis after discontinuation of lamivudine. If abdominal pain, nausea, vomiting or increased levels of pancreatic enzymes in the blood plasma occur, lamivudine should be discontinued and its use should not be resumed until the diagnosis of pancreatitis has been ruled out. During treatment, one should keep in mind the possibility of secondary infections caused by saprophytic microorganisms.