Release form and composition
Dosage forms:
- Film-coated tablets: almost white or white, round, biconvex shape (10 pieces in a blister, 5 blisters in a cardboard pack);
- Solution for intravenous (i.v.) administration: colorless transparent liquid (10 ml in colorless glass ampoules with a breaking point, 5 ampoules in a blister pack, 2 packs in a cardboard box).
1 tablet contains:
- Active ingredient: propafenone hydrochloride – 150 mg or 300 mg, which corresponds to a propafenone content of 135.7 mg or 271.05 mg;
- Auxiliary components: hypromellose 5, corn starch, granulated microcellulose, copovidone, magnesium stearate, croscarmellose sodium, macrogol 6000, sodium lauryl sulfate, dimethicone emulsion with silicon dioxide, titanium dioxide.
1 ml of solution contains:
- Active ingredient: propafenone hydrochloride – 3.5 mg;
- Auxiliary components: dextrose (glucose) monohydrate, water for injection.
Indications for use
Film-coated tablets The use of Propanorm is indicated for the prevention and treatment of arrhythmic pathologies:
- Paroxysmal rhythm disturbances (Wolf-Parkinson-White syndrome, supraventricular - fibrillation and atrial flutter);
- Ventricular and supraventricular extrasystole;
- Atrioventricular re-entry (mechanism of repeated reverse impulse entry) tachycardia.
In addition, tablets are prescribed for the prevention of sustained monomorphic ventricular tachycardia.
Solution for intravenous administration The solution is prescribed for the relief of paroxysms of atrial fibrillation, atrial flutter, supraventricular tachycardia, Wolff-Parkinson-White syndrome, ventricular tachycardia (in the absence of disturbances in the contractile function of the left ventricle).
Overdose of the drug Propanorm, symptoms and treatment
May manifest as anorexia, a feeling of fullness in the stomach, nausea, vomiting, impaired taste sensitivity, headache, decreased visual acuity, extrapyramidal disorders, coma, confusion, amnesia. Orthostatic reactions, bradycardia, AV node conduction disturbances (AV block, increased QRS complex) , ventricular tachycardia, atrial flutter, AV dissociation, sinus node weakness, cardiac arrest may occur; Symptoms of heart failure may occur and intensify, and seizures may develop. If symptoms of overdose appear, reduce the dose or discontinue the drug. Treatment : sodium lactate and potassium chloride are administered intravenously. Sometimes it becomes necessary to administer glucagon, epinephrine and use cardiac pacing.
Contraindications
- Severe arterial hypotension, severe bradycardia;
- Significant disturbance of water and electrolyte balance (including potassium metabolism);
- Severe form of chronic obstructive pulmonary disease (COPD);
- Concomitant use of ritonavir;
- Sick sinus syndrome;
- Atrioventricular block II-III degree;
- Pronounced changes in the myocardium of organic origin: refractory chronic heart failure with a left ventricular ejection fraction less than 35%, cardiogenic shock (not including arrhythmic shock);
- Breastfeeding period;
- Age up to 18 years;
- Hypersensitivity to the components of the drug.
In addition, the use of tablets is contraindicated:
- Violation of intraatrial conduction;
- Distal or bundle branch block in the absence of a pacemaker;
- Myasthenia;
- Uncontrolled chronic heart failure;
- Severe form of chronic heart failure in the decompensation stage.
Additional contraindications to the use of solution for intravenous injection:
- Acute coronary syndrome;
- Brugada syndrome;
- Myasthenia gravis;
- Impaired conduction of excitation between the atria and ventricles, intraventricular, sinoatrial blockade in patients without a pacemaker;
- Prolongation of the QT interval;
- Simultaneous use of tricyclic antidepressants, cisapride, phenothiazines, bepridil, macrolides for oral administration (drugs that prolong the QT interval).
Propanorm should be prescribed with caution for mild to moderate COPD, patients with an installed artificial heart pacemaker, and the elderly.
Besides:
- Tablets: renal and/or liver dysfunction, myasthenia gravis;
- Solution: bronchial asthma, organic myocardial damage, arterial hypotension, renal and/or liver failure, hyper- and hypokalemia.
The use of tablets and solution during pregnancy is indicated only for health reasons (especially in the first trimester), provided that the expected benefit from therapy for the mother exceeds the potential threat to the fetus.
Directions for use and dosage
Film-coated tablets The tablets are taken orally, after meals, swallowed whole and washed down with a sufficient amount of water.
The doctor prescribes and adjusts the dosage regimen individually, taking into account clinical indications.
The usual daily dose is 450 mg (150 mg 3 times a day every 8 hours). To achieve the desired therapeutic effect, an increase in the initial dose every 3-4 days to 600 mg per day (in 2 divided doses) or up to a maximum daily dose of 900 mg in 3 divided doses may be indicated.
The loading dose for relieving paroxysmal atrial fibrillation is 600 mg once.
If, while using Propanorm, the frequency and severity of arrhythmia increases, it is recommended to reduce the dose or temporarily discontinue the drug.
Patients with a body weight of less than 70 kg or over the age of 70 years are prescribed a reduced dose; use should begin in a hospital setting under the control of blood pressure (BP) and electrocardiography (ECG).
The dosage regimen for patients with impaired liver function should be 1/5-1/3 of the usual dose; for patients with impaired renal function (with creatinine clearance less than 10%), the initial dose is reduced by 2 times.
Solution for intravenous (IV) administration The solution is intended for IV jet or drip administration.
For infusion solution, only 5% glucose solution can be used!
Long-term infusion should be carried out 3-5 minutes after intravenous administration of the drug.
The dosage regimen is determined by the doctor based on electrocardiography data and the patient’s clinical condition individually.
Recommended dosage:
- IV jet administration: slowly - the drug is administered over 10 minutes at the rate of 1.5-2 mg per 1 kg of patient weight. To achieve a clinical effect, this dose can be re-administered after 90-120 minutes;
- Short-term infusion: over 60-180 minutes at a rate of 0.5-1 mg of the drug per minute - at the rate of 0.5-2 mg per 1 kg of weight. To achieve a clinical effect, the procedure can be repeated after 60-120 minutes;
- Long-term infusions: up to 560 mg per day, which is equivalent to 160 ml of Propanorm solution.
The daily dose should not exceed 560 mg.
For the treatment of severe arrhythmia, the use of short-term and long-term infusions is indicated.
The procedure for administering the drug should be carried out under careful monitoring of the patient's condition; in case of a significant change in heart rate (HR), expansion of the QRS complex by more than 25% or prolongation of the QT interval by more than 20%, the infusion must be stopped immediately!
In case of impaired renal and/or liver function, the use of even normal therapeutic doses can cause the accumulation of propafenone hydrochloride in the body. In this category of patients, the use of titrated doses of the drug under careful monitoring of ECG and concentrations of the active substance in the blood plasma is indicated.
After diluting the solution for intravenous administration in a 5% glucose solution, the stability (physical and chemical) of the drug is maintained for 72 hours at a temperature of 25 °C. But from a microbiological point of view, it is necessary to prepare the solution before direct use. If necessary, the solution ready for infusion can be used within the next 24 hours, provided that its storage temperature does not exceed 2-8 °C.
Propanorm®
The chemical and physical stability of the drug Propanorm® after dilution in a 5% glucose solution is maintained at 25 ° C for 72 hours. However, from a microbiological point of view, the prepared solution must be used immediately. In this case, it is recommended to use the drug no later than 24 hours under storage temperature conditions of 2-8 ° C, and only if the dilution of the solution was carried out under controlled aseptic conditions.
Proarrhythmogenic effect
Propafenone hydrochloride may cause new or worsen heart rhythm disturbances. This proarrhythmogenic effect ranges from an increase in the frequency of premature ventricular contractions (ventricular extrasystoles) to the development of ventricular tachycardia (including polymorphic ventricular tachycardia of the “pirouette” type) and ventricular fibrillation. Some of these arrhythmias are life-threatening and may require resuscitation to prevent death.
Considering the likely proarrhythmogenic effect of the drug, treatment with Propanorm® is recommended only as prescribed and under the supervision of a physician.
During the course of treatment, especially at the beginning of therapy, it is necessary to conduct ECG monitoring and clinical examination for early detection of side effects, assessment of the effectiveness of the drug and the advisability of continuing therapy. Before prescribing the drug, disturbances in water and electrolyte balance must be eliminated.
It is recommended that previous antiarrhythmic therapy be discontinued before starting treatment. The period between discontinuation of a previously prescribed antiarrhythmic drug and the prescription of Propanorm® should be at least 5 half-lives of the corresponding antiarrhythmic drug.
Treatment should be carried out by a cardiologist experienced in the treatment of relevant cardiac arrhythmias. When treating paroxysmal ventricular tachyarrhythmias, the patient should be under close cardiac monitoring (including ECG monitoring and blood pressure control) in a specialized department equipped with a defibrillator and other equipment to provide emergency medical care.
Discontinuation of treatment should be considered if any of the following ECG changes occur:
1) widening of the QRS complex or prolongation of the QT interval by more than 25% of the original;
2) prolongation of the PQ interval by more than 50% of the original;
3) prolongation of the QT interval over 500 ms or
4) increase in the frequency or severity of arrhythmias.
Brugada syndrome
The use of the drug Propanorm® can reveal the asymptomatic course of Brugada syndrome and cause Brugada-like changes on the ECG. Therefore, after starting drug therapy, an electrocardiological examination should be performed to exclude Brugada syndrome and Brugada-like changes on the ECG.
In patients with verified Brugada syndrome, the use of Propanorm® is contraindicated (see section “Contraindications”).
Supraventricular cardiac arrhythmias
There is a risk of conversion of paroxysmal atrial fibrillation to atrial flutter with atrioventricular conduction (conduction to the ventricles) of 2:1 or 1:1. The use of propafenone in patients with isolated atrial flutter or paroxysmal supraventricular tachycardia has not been studied.
Experience with the use of propafenone in patients with sick sinus syndrome is limited, and therefore the use of Propanorm® is contraindicated (except for patients with a functioning pacemaker).
Some patients with atrial flutter have developed 1:1 conduction of impulses when treated with propafenone, leading to an increase in ventricular rate. In such cases, it is possible to simultaneously use drugs that increase the functional refractory period of the atrioventricular connection.
Ventricular heart rhythm disturbances
Due to the risk of proarrhythmogenic effects, the use of Propanorm® in patients with less severe (non-life-threatening) ventricular arrhythmias is not recommended, even if these disorders are accompanied by symptoms that are unpleasant for the patient.
The use of Propanorm® is indicated only for patients in whom, in the opinion of the physician, the potential benefits outweigh the possible risks.
The effect of propafenone therapy on mortality in patients with ventricular arrhythmias has not been established.
Cardiac conduction disorders
Propafenone slows cardiac conduction, which can lead to a dose-dependent prolongation of the PQ interval, widening of the QRS complex, the development of first or higher degree atrioventricular block, bundle branch block and intraventricular conduction disturbances. The occurrence of cardiac conduction disturbances during therapy with Propanorm® requires a dose reduction or discontinuation of the drug (except in cases where the heart rate is adequately controlled by a pacemaker).
Heart failure
Propafenone has a negative inotropic effect on the myocardium, has beta-blocking activity and can cause decompensation of heart failure.
As with other class 1C antiarrhythmic drugs, serious side effects may occur in patients with significant organic changes in the myocardium when taking Propanorm®.
Myocardial infarction
The effectiveness and safety of the use of propafenone in patients with recent myocardial infarction have not been sufficiently studied, and therefore the use of Propanorm® in such patients is contraindicated (see section “Contraindications”). There are no results from controlled clinical studies confirming the beneficial effect of Propanorm® on survival or the incidence of sudden death in patients who have suffered myocardial infarction.
Effect on pacing threshold
The drug may increase the pacing and detection thresholds of a pacemaker or implanted cardioverter-defibrillator. During propafenone therapy and after its cessation, the parameters of these devices should be regularly checked and, if necessary, reprogrammed.
Obstructive pulmonary diseases
Propanorm®, like other drugs with beta-blocking action, should be used with extreme caution in patients with obstructive pulmonary diseases such as bronchial asthma and chronic obstructive pulmonary disease (COPD). In severe obstructive pulmonary diseases, the use of Propanorm® is contraindicated (see section “Contraindications”).
Liver dysfunction
Propafenone is actively metabolized in the liver. In severe liver dysfunction, the bioavailability of propafenone increases to 70% (compared to 3% - 40% in patients with normal liver function). In 8 patients with moderate or severe hepatic impairment, the mean elimination half-life was approximately 9 hours. In cases of liver dysfunction, there is also a decrease in systemic clearance of the drug and a decrease in binding to plasma proteins. This leads to excessive accumulation of propafenone hydrochloride.
In patients with impaired liver function, Propanorm® should be used with caution. The dose of the drug should be reduced. It is recommended to regularly monitor clinical and electrocardiographic parameters for signs of excessive pharmacological effects and/or side effects until an individualized dosage regimen can be determined.
In the post-registration period, cases of the development of liver damage associated with the use of propafenone drugs have been described. Some patients had hepatocellular liver disease, other cases were associated with cholestasis, and some were of a mixed nature. In some cases, liver damage was detected only by a biochemical blood test, while others manifested with clinical symptoms.
In one case, recurrence of liver damage was observed after resumption of propafenone, with a favorable outcome after discontinuation of therapy.
Agranulocytosis
Cases of agranulocytosis have been described in patients receiving propafenone. As a rule, agranulocytosis developed during the first 2 months of use of propafenone; upon discontinuation of therapy, the white blood cell count usually returned to normal within 14 days. Unexplained fever or decreased white blood cell counts, especially during the first 3 months of therapy, require careful evaluation to identify possible agranulocytosis or granulocytopenia.
If agranulocytosis is suspected, you should immediately stop taking Propanorm®. Patients should be warned to seek immediate medical attention if any signs of an infectious disease (eg, fever, sore throat, or chills) occur.
Myasthenia gravis
Propanorm® may worsen the condition of a patient with myasthenia gravis, and therefore the use of Propanorm® in such patients is contraindicated (see section “Contraindications”).
Increased titer of antinuclear antibodies
Positive antinuclear antibody titers have been recorded in patients receiving propafenone. They were reversible after cessation of treatment and may disappear even with continued use of propafenone. These laboratory values were generally not associated with clinical symptoms. However, there is one published case of drug-induced lupus erythematosus (with recurrence of symptoms after restarting the drug); the disease resolved completely after cessation of therapy.
Patients who develop abnormal antinuclear antibodies should be carefully evaluated. If elevated antinuclear antibody titers persist or increase, discontinuation of therapy should be considered.
Spermatogenesis disorder
A clinical evaluation of spermatogenesis in healthy volunteers was carried out. A decrease in ejaculate volume and a decrease in sperm count have been demonstrated. Follicle-stimulating hormone (FSH) and testosterone levels in the blood were also slightly reduced. Both values remained within the laboratory's normal reference range. A decrease in spermatogenesis has also been observed in animal experiments. The clinical significance of these results remains uncertain.
Side effects
Film-coated tablets
- Cardiovascular system: ventricular tachyarrhythmias, atrioventricular (AV) dissociation, bradycardia, worsening heart failure (with reduced left ventricular function), angina pectoris, sinoatrial (SA) block, intraventricular conduction disorders, AV block, supraventricular tachyarrhythmias, against the background of high doses – orthostatic hypotension;
- Nervous system: dizziness, headache; rarely – diplopia, convulsions, blurred vision;
- Digestive system: dry mouth, changes in taste, bitterness in the mouth, decreased appetite, nausea, heaviness in the epigastric zone, constipation, diarrhea; rarely - functional liver disorder, cholestasis, cholestatic jaundice;
- Genitourinary system: decreased potency, oligospermia;
- Allergic reactions: skin itching, rash, redness of the skin, exanthema, lupus-like syndrome, urticaria;
- Laboratory indicators: the appearance of antinuclear antibodies, agranulocytosis, leukopenia, increased duration of bleeding, thrombocytopenia;
- Other: bronchospasm, weakness, hemorrhagic skin rashes.
Solution for intravenous administration
- Cardiovascular system: very often – palpitations, conduction disturbances; often - bradycardia, with reduced contractile function of the left ventricle - worsening of the course of heart failure; SA block, AV block, ventricular tachyarrhythmias, intraventricular conduction disorders, supraventricular tachyarrhythmias, when taken in high doses - a significant decrease in blood pressure (including postural and orthostatic hypotension); rarely – proarrhythmias (increased heart rate (tachycardia), ventricular fibrillation); frequency unknown – worsening of chronic heart failure;
- Nervous system: very often – dizziness; often – fainting; uncommon – confusion, anxiety, headache, paresthesia, ataxia; rarely – blurred visual perception, diplopia; frequency unknown - extrapyramidal symptoms, seizures;
- Digestive system: often – dry mouth, dyspeptic disorders, taste disturbance; uncommon – cholestasis, liver disease, hepatitis, jaundice; frequency unknown - gagging;
- Mammary glands and genital organs: rarely – impotence; frequency unknown – transient decrease in sperm count;
- Connective tissues and musculoskeletal system: rarely - syndrome with symptoms of systemic lupus erythematosus;
- Laboratory tests: uncommon – thrombocytopenia, increased activity of liver enzymes (alkaline phosphatase, alanine aminotransferase, aspartic aminotransferase); rarely – agranulocytosis, leukopenia; frequency unknown - granulocytopenia;
- Allergic reactions: uncommon - rash, itching, redness of the skin, urticaria;
- Other: bronchospasm, weakness, arthralgia.
Side effects of the drug Propanorm
When taking Propanorm in a high dose, anorexia, a feeling of fullness in the stomach, nausea, vomiting, impaired taste, dry mouth, and in isolated cases - dizziness, headache, weakness, decreased visual acuity, sleep disturbance, extrapyramidal disorders, coma, confusion may occur. , memory loss. Allergic reactions are sometimes noted. Elderly patients may experience orthostatic reactions, sometimes bradycardia, AV node conduction disturbances (AV block, increased QRS complex) , ventricular extrasystole and tachycardia, atrial flutter, AV dissociation, sinus node weakness, cardiac arrest; angina attacks, symptoms of heart failure may occur or worsen. Cholestasis, decreased potency, anemia, hemorrhagic rash, neutropenia, increased bleeding time, leukopenia, and thrombocytopenia are extremely rarely noted. The composition of peripheral blood is normalized after discontinuation of the drug.
special instructions
The entire period of therapy should be accompanied by regular ECG monitoring, monitoring the activity of liver transaminases, electrolyte balance (especially the level of potassium concentration in the blood).
If there are electrolyte imbalances, they should be corrected before starting the drug.
Due to the increased risk of arrhythmogenic activity of propafenone, treatment should be started in a hospital setting.
The use of Propanorm for the treatment of ventricular arrhythmias has a more effective effect than class IA and IB antiarrhythmic drugs.
The bioavailability of the drug in patients with liver failure is 70% higher than usual, so they should be prescribed a reduced dose and regularly monitor laboratory parameters.
In patients with an artificial cardiac pacemaker, special care should be taken when determining the indications and dose of the drug.
With long-term use of anticoagulants and hypoglycemic agents, the patient requires regular clinical monitoring and careful monitoring of laboratory parameters.
During the use of the solution, Brugada-like changes may appear on the ECG and the asymptomatic course of Brugada syndrome may be diagnosed. Therefore, the administration of the drug should be accompanied by an electrocardiological examination.
If third-degree AV block, SA block, or frequently recurring extrasystole occurs while taking propafenone, therapy should be discontinued.
Due to the risk of proarrhythmogenic effects, the use of the drug is indicated only as directed and under the supervision of a physician.
Propanorm affects the ability to concentrate attention and the speed of psychomotor reactions, therefore during the treatment period the patient should refrain from driving vehicles and machinery.
Drug interactions
With simultaneous use of Propanorm:
- Lidocaine enhances the cardiodepressive effect of the drug, so this combination is contraindicated;
- Propranolol, indirect anticoagulants, metoprolol, cyclosporine increase their concentration in blood plasma;
- Digoxin increases the risk of developing glycoside intoxication;
- Warfarin enhances its effect against the background of blocking metabolism;
- Local anesthetics increase the risk of damage to the central nervous system;
- Tricyclic antidepressants, beta-blockers can enhance the antiarrhythmic effect of the drug;
- Amiodarone increases the likelihood of pirouette-type tachycardia;
- Quinidine, cimetidine help increase the concentration of propafenone in the blood plasma by 20%;
- Rifampicin, by accelerating metabolism, reduces the therapeutic effect of the drug (dose adjustment is required).
With concomitant therapy with drugs that inhibit bone marrow hematopoiesis, the risk of myelosuppression increases.
The likelihood of developing side effects of Propanorm increases when combined with drugs that have a negative inotropic effect or suppress the AV and SA nodes.
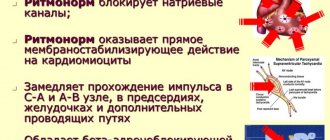
Pharmacological properties of the drug Propanorm
Propafenone hydrochloride (1-[2-[2-hydroxy-3-propylamino)propoxy]phenyl]-3-phenyl-1-propanone hydrochloride) is a class Ic antiarrhythmic drug with a moderate β-adrenergic blocking effect. It has a direct membrane-stabilizing effect on myocardiocytes, inhibits fast sodium channels, reduces the maximum rate of depolarization of myocardiocytes and their excitability. Slows down impulse conduction in the atria, AV node, especially in the His bundle system and Purkinje fibers. Propafenone increases the P-R and slightly increases the QRS. In the presence of additional conduction pathways, their refractory period increases and completely blocks the conduction of excitation in both the antegrade and retrograde directions. The drug increases the effective refractory period of the AV node and ventricles. Absorption when taken orally is almost complete (95%). The maximum concentration in blood plasma is achieved after 2–3 hours. Propanorm exhibits dose-dependent bioavailability. Almost completely (85–97%) binds to proteins in blood plasma and internal organs (liver, lungs, etc.). It undergoes biotransformation in the liver using the cytochrome P450 system, the activity of which is determined genetically. There are 2 main phenotypes - in most people (90%), biotransformation occurs quickly with the formation of active metabolites (5-hydroxypropafenone, N-depropylpropafenone, etc.). The half-life in such patients is 2–10 hours (average 5.5 hours). In the slow metabolizer phenotype, the first-pass effect through the liver is much less pronounced, with an elimination half-life of 10–32 hours (average 17.2 hours). The effect develops approximately 1 hour after oral administration, reaches its maximum severity after 2–3 hours and lasts 8–12 hours. The range of therapeutic concentrations of propafenone in blood plasma is 0.5–2 mg/l. About 10% of the drug is excreted in the urine in the form of metabolites, most of the dose (87%) is excreted in bile (in the form of propafenone glucuronides and sulfates).