Signicef - eye drops made in India, are prescribed in the treatment of infectious lesions of the organs of vision and are used as a means of prevention.
Safe for small children, but prohibited for pregnant and lactating women.
adverse reactions in 10% of patients , so treatment should be carried out under medical supervision.
Release form and composition
The drug is produced in the form of eye drops, which are a transparent light yellow solution (5 ml in plastic dropper bottles with a screw cap; in a cardboard box there is 1 dropper bottle and instructions for use of Signicef).
Composition per 1 ml drops:
- active ingredient: levofloxacin (in the form of levofloxacin hemihydrate) – 5 mg;
- auxiliary components: hypromellose, sodium hydroxide, benzalkonium chloride, hydrochloric acid, sodium chloride, water for injection.
Pharmacological group
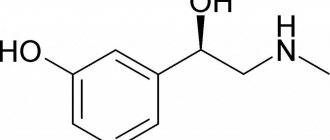
The drug represents the pharmacological group of antibacterial agents, fluoroquinolones. The main active component levofloxacin has an inhibitory effect on the functional activity of the enzyme DNA gyrase, as a result of which the process of replication and transformation of bacterial deoxyribonucleic acid is disrupted. The drug's activity is more pronounced against bacteria that are in the process of cell division. The result of exposure to levofloxacin is the death of various types of pathogenic and opportunistic bacteria (bactericidal pharmacological action). The drug has sufficient activity against a large number of bacteria, which include staphylococci, streptococci, intestinal, Pseudomonas aeruginosa, Klebsiella, chlamydia, salmonella, shigella, campylobacter, proteus.
After instillation of the ophthalmic solution, the active compound has a therapeutic effect in the tissues of the eye structures. It is absorbed into the blood, metabolized in the liver and excreted in the urine in the form of inactive breakdown products.
Pharmacological properties
Pharmacodynamics
Levofloxacin is a fluoroquinolone. It is the L-isomer of the racemic substance ofloxacin. The antibacterial effect of ofloxacin is associated primarily with the L-isomer.
Levofloxacin blocks the enzymes topoisomerase IV and DNA gyrase, disrupts the cross-linking of breaks and supercoiling of DNA, inhibits DNA synthesis and causes serious changes in morphology in the cytoplasm, membranes and cell walls of bacteria. In in vitro studies, the activity of levofloxacin against Pseudomonas aeruginosa, enterobacteria and gram-positive microorganisms was approximately 2 times higher than the activity of ofloxacin.
Signicef is effective against the following microorganisms:
- gram-negative aerobic bacteria: Haemophilus influenzae, Pseudomonas aeruginosa, Branhamella (Moraxella) catarrhalis, Neisseria gonorrhoeae;
- gram-positive aerobic bacteria: Streptococcus pneumoniae, Staphylococcus aureus, Streptococcus pyogenes;
- gram-negative anaerobic bacteria: Chlamydia trachomatis.
When using levofloxacin in the form of eye drops 5 mg/ml, the achieved Cmax (maximum concentration) of the active substance in the eye tissues is more than 100 times higher than the MIC (minimum inhibitory concentration) of the drug for organisms sensitive to it.
Pharmacokinetics
After Signicef is instilled into the eyes, the active substance is well preserved in the tear film. Its content in tear fluid very quickly reaches high values. For at least 6 hours, the concentration of levofloxacin is maintained at a level exceeding the MIC (minimum inhibitory concentration) of most pathogens sensitive to the drug and is 2 mcg/ml or less. Studies conducted on healthy volunteers showed that the average levels of the active substance measured 4 hours and 6 hours after instillation were 17 μg/ml and 6.6 μg/ml, respectively.
In blood plasma, the average concentration of levofloxacin 1 hour after instillation is about 0.86 ng/ml, and then during the first day it increases to 2.05 ng/ml. Cmax in plasma equal to 2.25 ng/ml was detected on the 4th day after two days of using levofloxacin every 2 hours (but not more than 8 times a day). Despite this, Cmax, which was achieved on the 15th day of therapy, was 1000 times or more lower than those concentrations that are recorded after taking levofloxacin orally.
Signicef eye drops 0.5% 5ml fl-cap 1 pc. in Cherepovets
Pharmacological action: Pharmacodynamics
Has a wide spectrum of action. Inhibits bacterial topoisomerase IV and DNA gyrase (type II topoisomerases) - enzymes necessary for replication, transcription, repair and recombination of bacterial DNA. In concentrations equivalent to or slightly higher than inhibitory concentrations, it most often has a bactericidal effect. In vitro
Resistance to levofloxacin, resulting from spontaneous mutations, is rare (10−9−10−10). Although cross-resistance has been observed between levofloxacin and other fluoroquinolones, some organisms resistant to other fluoroquinolones may be sensitive to levofloxacin.
Installed in vitro
and confirmed in clinical studies to be effective against gram-positive bacteria -
Enterococcus faecalis, Staphylococcus aureus
(methicillin-sensitive strains),
Staphylococcus epidermidis
(methicillin-sensitive strains)
, Staphylococcus saprophyticus, Streptococcus pneumoniae
(including multi-resistant strains -
MDRSP
*),
Streptococcus pyogenes
;
gram-negative bacteria - Enterobacter cloacae, Escherichia coli, Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Legionella pneumophila, Moraxella catarrhalis, Proteus mirabilis, Pseudomonas aeruginosa,
Serratia
marcescens
and other microorganisms -
Chlamydia pneumoniae, Mycoplasma pneumoniae.
Against most (≥90%) strains of the following microorganisms in vitro
The MIC of levofloxacin has been established (2 μg/ml or less), however, the effectiveness and safety of the clinical use of levofloxacin in the treatment of infections caused by these pathogens has not been established in adequate and well-controlled studies: gram-positive bacteria -
Staphylococcus haemolyticus, Streptococcus
(group C/F),
Streptococcus
(group G),
Streptococcus agalactiae, Streptococcus milleri
,
Streptococcus viridans
,
Bacillus anthracis
;
gram-negative bacteria - Acinetobacter lwoffii, Acinetobacter baumannii, Bordetella pertussis, Citrobacter (diversus) koseri, Citrobacter freundii, Enterobacter aerogenes, Enterobacter sakazakii, Klebsiella oxytoca, Morganella morganii, Pantoea (Enterobacter) agglomerans, Proteus vulgaris, Providencia rettgeri, Providencia s tuartii, Pseudomonas fluorescens
,
Yersinia pestis
;
gram-positive anaerobes - Clostridium perfringens.
May be effective against microorganisms resistant to aminoglycosides, macrolides and beta-lactam antibiotics (including penicillin).
* Strains with multiple resistance to antibiotics ( Multi-drug resistant Streptococcus pneumoniae
-
MDRSP
) include strains resistant to two or more of the following antibiotics: penicillin (with MIC ≥2 μg/ml), second generation cephalosporins (for example, cefuroxime), macrolides, tetracyclines and trimethoprim/sulfamethoxazole.
Clinical researches
Efficacy of levofloxacin in the treatment of community-acquired bacterial pneumonia (7-14 day dosing regimen)
studied in two prospective multicenter clinical studies.
The first randomized study, which included 590 patients with community-acquired bacterial pneumonia, compared the effectiveness of levofloxacin at a dose of 500 mg once daily orally or intravenously for 7–14 days and cephalosporins with a total treatment duration of 7–14 days; if the presence of an atypical pneumonia pathogen was suspected or confirmed, patients in the comparison group could additionally receive erythromycin or doxycycline. The clinical effect (cure or improvement) on days 5–7 after completion of levofloxacin therapy was 95% compared to 83% in the comparison group. In the second study, which included 264 patients who received levofloxacin 500 mg once daily orally or intravenously for 7–14 days, the clinical response was 93%. In both studies, the effectiveness of levofloxacin in the treatment of atypical pneumonia caused by Chlamydia pneumoniae, Mycoplasma pneumoniae
and
Legionella pneumoniae
was 96, 96 and 70%, respectively.
The degree of microbiological eradication in both studies was depending on the pathogen: H.influenzae
- 98%,
S.pneumoniae
- 95%,
S.aureus
- 88%,
M.catarrhalis
- 94%,
H.parainfluenzae
- 95%,
K.pneumoniae
- 100%.
Levofloxacin is effective for the treatment of community-acquired pneumonia caused by strains of Streptococcus pneumoniae
multidrug resistant
(MDRSP).
After microbiological evaluation
of MDRSP
isolates isolated from 40 patients, it was found that 38 patients (95%) achieved clinical (recovery or improvement) and bacteriological effect after completion of levofloxacin therapy. The degree of bacteriological eradication for different pathogens was: penicillin-resistant strains - 94.1%, strains resistant to 2nd generation cephalosporins - 96.9%, strains resistant to macrolides - 96.6%, strains resistant to trimethoprim/sulfamethoxazole - 89.5%, strains resistant to tetracyclines - 100%.
Efficacy and safety of levofloxacin in community-acquired bacterial pneumonia (5-day dosing regimen)
were evaluated in a double-blind, randomized, prospective, multicenter study in 528 outpatient and hospitalized adult patients with clinically and radiologically defined mild to severe community-acquired pneumonia, comparing levofloxacin 750 mg (IV or orally every day for five days) or at a dose of 500 mg (iv or orally daily for 10 days).
The clinical effect (improvement or recovery) was 90.9% in the group receiving levofloxacin 750 mg and 91.1% in the group receiving levofloxacin 500 mg. Microbiological effectiveness (degree of bacteriological eradication) of a 5-day dosing regimen depending on the pathogen: S. pneumoniae
- 95%,
Haemophilus influenzae
- 100%,
Haemophilus pararainfluenzae
- 100%,
Mycoplasma pneumoniae
- 96%,
Chlamydophila pneumoniae
- 87%.
Efficacy and safety of levofloxacin in the treatment of acute bacterial sinusitis
(5- and 10-14-day dosing regimens) caused by
Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis,
was evaluated in a double-blind, randomized, prospective, multicenter study in 780 outpatients who received levofloxacin 750 mg orally once daily. for 5 days or 500 mg for 10 days. The clinical effect of levofloxacin (complete or partial resolution of symptoms of acute bacterial sinusitis to the extent that further antibiotic therapy was not considered necessary) according to microbiological assessment was 91.4% in the group receiving levofloxacin 750 mg and 88.6% in the group receiving levofloxacin 750 mg and group receiving 500 mg levofloxacin.
Efficacy of levofloxacin in the treatment of complicated urinary tract infections and acute pyelonephritis (5-day dosing regimen)
was evaluated in 1109 patients in a randomized, double-blind, multicenter clinical trial in which patients received levofloxacin 750 mg IV or orally once daily for 5 days (546 patients) or ciprofloxacin 400 mg IV or 500 mg orally twice daily for 10 days (563 patients).
The effectiveness of levofloxacin was assessed after 10–14 days by the degree of bacteriological eradication and was, depending on the pathogen: Escherichia coli
- 90%,
Klebsiella pneumoniae
- 87%,
Proteus mirabilis
- 100%.
Efficacy and safety of levofloxacin in the treatment of complicated urinary tract infections and acute pyelonephritis (10-day dosing regimen)
evaluated a 10-day course of treatment with levofloxacin 250 mg orally once daily in 285 patients with uncomplicated urinary tract infections, complicated urinary tract infections (mild to moderate), and acute pyelonephritis (mild to moderate) in a randomized, double-blind, multicenter clinical trial. Microbiological effectiveness, measured by bacteriological eradication of microorganisms, was approximately 93%.
Efficacy of levofloxacin for infectious lesions of the skin and skin structures
studied in an open, randomized comparative study that included 399 patients who received levofloxacin at a dose of 750 mg/day (iv, then orally) or a comparison drug for (10±4.7) days. Surgical procedures for complicated infections (excision of dead tissue and drainage) shortly before the start or during antibacterial therapy (as part of complex therapy) were performed in 45% of patients receiving levofloxacin and 44% of patients in the comparison group. Among patients who were observed for 2–5 days after the end of drug therapy, the clinical effect was 116/138 (84.1%) in the group receiving levofloxacin and 106/132 (80.3%) in the comparison group.
The effectiveness of levofloxacin was also demonstrated in a multicenter randomized open trial in the treatment of nosocomial pneumonia
and in a multicenter, randomized, double-blind study in the treatment
of chronic bacterial prostatitis.
Eye drops
The clinical effect of levofloxacin 0.5% eye drops in randomized, double-blind, multicenter controlled trials in the treatment of bacterial conjunctivitis was 79% at the end of treatment (days 6–10). The degree of microbiological eradication reached 90%.
Pharmacokinetics
Absorption.
After oral administration, it is quickly and completely absorbed from the gastrointestinal tract; the absolute bioavailability of 500 mg and 750 mg tablets of levofloxacin is 99%. Cmax is reached within 1–2 hours. When taken simultaneously with food, the time to reach Cmax slightly increases (by 1 hour) and Cmax decreases slightly (by 14%), thus, levofloxacin can be prescribed regardless of food intake. After a single intravenous administration to healthy volunteers at a dose of 500 mg (infusion over 60 minutes), Cmax was (6.2 ± 1) μg/ml, at a dose of 750 mg (infusion over 90 minutes) - (11.5 ± 4 ) µg/ml. The pharmacokinetics of levofloxacin is linear and predictable with single and repeated oral and intravenous administration. Constant concentration in plasma is achieved after 48 hours when taking 500–750 mg 1 time per day. With repeated administration to healthy volunteers, the Cmax values were: for oral administration 500 mg/day - (5.7 ± 1.4) μg/ml, 750 mg/day - (8.6 ± 1.9) μg/ml; with intravenous administration, 500 mg/day - (6.4±0.8) µg/ml, 750 mg/day - (12.1±4.1) µg/ml. The plasma concentration profile of levofloxacin after intravenous administration is similar to that after oral administration at an equivalent dose.
Distribution.
The average Vd is 74–112 L after single and repeated doses of 500 and 750 mg.
Widely distributed in body tissues, penetrates well into lung tissue (concentration in the lungs is 2–5 times higher than the concentration in plasma). In vitro
, in the concentration range corresponding to clinical values (1–10 μg/ml), binding to plasma proteins (mainly albumin) is 24–38% and does not depend on the concentration of levofloxacin.
Metabolism and excretion.
Stereochemically stable in plasma and urine, does not convert to its enantiomer, D-ofloxacin. It is practically not metabolized in the body. It is excreted predominantly unchanged in the urine (about 87% of the dose within 48 hours), small amounts in feces (less than 4% within 72 hours). Less than 5% is determined in urine in the form of metabolites (desmethyl, nitric oxide), which have little specific pharmacological activity.
Terminal T1/2 from plasma is 6–8 hours after a single or repeated administration orally or intravenously. Total Cl is 144–226 ml/min, renal Cl is 96–142 ml/min, excretion is carried out by glomerular filtration and tubular secretion. Concomitant use of cimetidine or probenecid leads to a decrease in renal Cl by 24 and 35%, respectively, indicating secretion of levofloxacin by the proximal tubules. Levofloxacin crystals were not detected in freshly collected urine.
Special patient groups
Age, gender, race.
The pharmacokinetics of levofloxacin does not depend on the age, gender and race of patients.
After administration of 500 mg orally to healthy male volunteers, T1/2 averaged 7.5 hours compared to 6.1 hours in women; the differences were associated with the characteristics of renal function in men and women and were not of clinical significance.
Features of pharmacokinetics depending on race were studied by covariance analysis of data from 72 subjects: 48 representatives of the Caucasian race and 24 others; no differences were found in terms of total clearance and volume of distribution.
Elderly age.
The pharmacokinetics of levofloxacin in elderly patients does not differ significantly when individual differences in creatinine clearance values are taken into account. After a single oral dose of 500 mg levofloxacin, T1/2 in healthy elderly patients (66–80 years) was 7.6 hours compared to 6 hours in younger patients; the differences are explained by variability in renal function and are not clinically significant. No dose adjustment is required in elderly patients.
Kidney failure.
In patients with impaired renal function (Cl creatinine <50 ml/min), the clearance of levofloxacin is significantly reduced and T1/2 is increased; dose adjustment is required to prevent accumulation. Hemodialysis and long-term ambulatory peritoneal dialysis do not remove levofloxacin from the body and therefore do not require additional doses.
Liver failure.
Pharmacokinetic studies have not been conducted in patients with liver disease. Since the metabolism of levofloxacin is negligible, liver damage is not expected to influence pharmacokinetics.
Children
. After a single intravenous administration of levofloxacin at a dose of 7 mg/kg in children aged 6 months to 16 years, the drug was eliminated faster than in adult patients. Subsequent pharmacokinetic analysis shows that a dosing regimen of 8 mg/kg (not more than 250 mg per dose) every 12 hours in children 6 months - 17 years at steady state will achieve plasma AUC0-24 and Cmax values comparable to those in adults patients at a dose of levofloxacin 500 mg every 24 hours.
Pharmacokinetics of levofloxacin in patients with severe community-acquired pneumonia
does not differ from that in healthy volunteers.
Study of the pharmacokinetics of levofloxacin when used as 0.5% eye drops
was carried out on 15 healthy adult volunteers. Levofloxacin plasma concentrations were measured at various time points throughout the 15-day course of use. The average plasma concentration of levofloxacin 1 hour after instillation varied from 0.86 ng/ml on the first day to 2.05 ng/ml on the fifteenth day. Cmax of levofloxacin in plasma was 2.25 ng/ml and was achieved on the 4th day after 2 days of use every 2 hours (up to 8 times a day). The Cmax of levofloxacin achieved on day 15 was more than 1000 times lower than the concentration observed after oral administration of standard doses of levofloxacin.
In studies in healthy adult volunteers (n=30), the mean tear film concentrations of levofloxacin measured 4 and 6 hours after instillation were 17.0 mcg/mL and 6.6 mcg/mL, respectively (clinical significance unknown) .
Experimental toxicology and/or pharmacology
Levofloxacin and other fluoroquinolones have been shown to cause arthropathy in young growing animals of most species tested.
Oral administration of levofloxacin at a dose of 40 mg/kg/day in 3-month-old dogs resulted in clinically significant arthropathy and discontinuation of dosing on day 8 of the planned 14 days. Minor musculoskeletal clinical effects in the absence of gross pathological or histopathological abnormalities were observed with the lowest dose level of 2.5 mg/kg/day (approximately 0.2 times the pediatric dose based on AUC comparisons). Synovitis and articular cartilage lesions were observed at doses of 10 and 40 mg/kg (approximately 0.7 and 2.4 times the pediatric dose based on AUC comparisons). Gross articular cartilage pathology and histopathological changes persisted until the end of the 18-week recovery period in dogs treated with levofloxacin 10 and 40 mg/kg/day.
In animal experiments, administration of levofloxacin orally or intravenously to immature rats and dogs resulted in an increase in the incidence of osteochondrosis. Histopathological examination of weight-bearing joints in immature dogs exposed to levofloxacin revealed persistent cartilage lesions. Other fluoroquinolones also cause similar erosive changes in weight-bearing joints and other manifestations of arthropathy in immature animals of various species.
In immature dogs (4–5 months of age), oral administration at a dose of 10 mg/kg/day for 7 days or IV at a dose of 4 mg/kg/day for 14 days led to the development of arthropathy. Oral administration of 300 mg/kg/day for 7 days or intravenous administration of 60 mg/kg/day for 4 weeks caused arthropathy in immature rats.
In studies in mice, levofloxacin had phototoxic effects similar in severity to ofloxacin, but less pronounced compared to other fluoroquinolones.
Although crystalluria was observed in rats given IV in some studies, urinary crystals did not form in the bladder, were detected only after urination, and were not associated with nephrotoxicity.
In experiments on mice, the stimulating effect of fluoroquinolones on the central nervous system was enhanced when used simultaneously with NSAIDs.
When administered rapidly intravenously to dogs at a dose of 6 mg/kg or more, levofloxacin caused a hypotensive effect, presumably due to the release of histamine.
in vitro studies
and
in vivo
, levofloxacin within therapeutic concentrations did not have an inducing or inhibitory effect on enzyme systems, i.e., an enzyme-mediated effect on the metabolism of other drugs is not expected.
Carcinogenicity, mutagenicity, effect on fertility
In intravital biological studies in rats, levofloxacin did not exhibit carcinogenic properties when administered daily orally for 2 years at doses up to 100 mg/kg/day (1.4 times the MRDC (750 mg), based on body surface area). Levofloxacin, at any dosage regimen, did not reduce the time to development of UV-induced skin tumors in hairless albino mice (Skh-1) and thus did not exhibit photocarcinogenic properties under experimental conditions. The concentration of levofloxacin in the skin tissues of hairless mice was in the range of 25–42 μg/g when using the maximum dose in the photocarcinogenicity study (300 mg/kg/day). For comparison, in humans, the concentration of levofloxacin in skin tissues when administered at a dose of 750 mg averages 11.8 mcg/g with Cmax in plasma.
Did not show mutagenic properties in the following studies: Ames test on S. Typhimurium
and
E.Coli,
hypoxanthine-guanine phosphoribosyltransferase test in Chinese hamster ovary cells, micronucleus test in mice, dominant lethal mutation test in mice, unscheduled DNA synthesis test in rats, sister chromatid exchange test in mice.
Mutagenic activity was detected in in vitro
for chromosomal aberrations (on the CHL cell line) and sister chromatid exchange (on the CHL/IU cell line).
It had no effect on the fertility and reproductive function of rats when administered orally at a dose of 360 mg/kg/day (4.2 times the MRDC, based on body surface area) or intravenously at a dose of 100 mg/kg/day (in 1.2 times the MRFC, in terms of body surface area).
Side effects
Adverse reactions may occur in approximately 10% of patients.
Most often (in 1–10% of cases) there is a decrease in visual acuity and the appearance of mucous discharge in the form of strands.
Rarely (in 0.1–1% of cases), patients experience the following undesirable side effects: swelling of the eyelids, itching and burning in the eye, conjunctival hyperemia, erythema of the eyelids, blepharitis, discomfort in the eye, mucous discharge, severe swelling of the conjunctiva of the eyeball, dry eye syndrome, papillary growths on the conjunctiva, eye pain, conjunctival folliculosis, blurred vision, headache, photophobia, rhinitis, contact dermatitis, allergic reactions.
Applications and dosages
Eye drops are instilled into the lower conjunctival sac. To do this, the head is tilted back, the lower eyelid is pulled down, and instillation is carried out with the other hand using a dropper bottle. It is important not to touch the surface of the eye, as this can cause mechanical damage or infection of the tissue.
for adults
The average recommended therapeutic dose for adults is 1-2 drops, which are instilled into the conjunctival sac up to 8 times a day (usually every 2 hours) during the first 2 days. Then the frequency of instillation is reduced to 4 times a day. The average duration of therapy is 5 days.
for children
No dose adjustment is required for children over 1 year of age.
for pregnant women and during lactation
The medication is contraindicated.
special instructions
The drug must not be administered into the anterior chamber of the eye or subconjunctivally.
If other local ophthalmic agents are used simultaneously with Signicef eye drops, the minimum interval between instillations of the drugs should be 15 minutes.
The drops contain benzalkonium chloride as a preservative, so they should not be used while wearing soft (hydrophilic) contact lenses. Benzalkonium chloride can be absorbed by contact lenses, cause discoloration, and also adversely affect eye tissue when wearing lenses.
When instilling Signicef, you should not touch the tip of the dropper bottle to the cornea of the eye, as this leads to contamination of the bottle and solution.
Impact on the ability to drive vehicles and complex mechanisms
No data available.
Indications for use
Why is the drug prescribed:
- for the treatment of non-infectious and infectious diseases;
- for carrying out preventive measures after laser and surgical operations on the eyes.
The drug effectively copes with conjunctivitis, keratitis, and blepharitis. Can be used in the complex treatment of barley.
The ophthalmic drug is approved for the treatment of patients from 1 year of age.
Reviews about Signitsef
Patients who have used the drug claim that it is effective, helps with conjunctivitis of various origins, and has a wide spectrum of action. Therefore, almost all reviews about Signicef are very good. It quickly relieves inflammation, does not cause discomfort when instilled, and is easy to use. The drops are available and the price is quite reasonable. One bottle is enough for a course of treatment.
Among the disadvantages, in some cases there is a ban on the use of drops during pregnancy and lactation, as well as some adverse reactions (for example, a burning sensation).
Analogs
The best similar drugs include Oftaquix, L-Optic Rompharm, Diklo-F.
These drugs have identical effects and indications for use to the original. They differ in cost, contraindications and adverse reactions.
Brief description of analogues:
- Oftaquix. French analogue based on levofloxacin. Prescribed in the treatment of ophthalmic diseases, contraindicated during pregnancy, lactation, and the body's immunity to the elements of the composition.
Adverse reactions occur extremely rarely; they manifest themselves mainly in the form of burning in the eyes and decreased clarity of vision. It is not advisable to use the drug in patients under 18 years of age.
You can buy a bottle of drops for about 280 rubles.
- Diklo-F. A similar drug made in India, based on diclofenac. Used in the treatment of infectious and non-infectious eye diseases.
Prohibited for use in case of ulcerative and erosive lesions of the stomach, hematopoietic disorders, or the body's immunity to the elements of the composition. At the moment, there is no accurate data on the effect of the drug on the health of a pregnant woman and the development of the baby, so the drug is prescribed with caution during pregnancy and lactation. Approved for the treatment of children from the age of twelve. When using the drug, the patient may experience headache, discomfort in the eyes, and swelling of the eyelids.
The approximate cost of a bottle of drops is 160 rubles.
- L-Optic . Ophthalmic product produced in Romania. Like the original, it is based on the substance levofloxacin. A powerful antimicrobial drug prescribed in the treatment of infections affecting the organs of vision. Approved for use in children over 1 year of age; at the discretion of the physician, it can be used in the treatment of eye diseases in pregnant and lactating women. Contraindicated only in case of hypersensitivity to the composition. Adverse reactions may occur in the form of burning in the eyes, mucus formation, and lacrimation. Many patients experienced increased sensitivity to light.
Approximate cost: 195 rubles.
It is necessary to remember: you can replace one drug with another only after consultation with an ophthalmologist!
Signicef is a highly effective ophthalmic drug, sold only with a prescription from an ophthalmologist.
Occasionally causes adverse reactions, the occurrence of which should be reported to the attending physician.