The medical term anal incontinence is used to describe a disorder characterized by fecal incontinence and the patient's inability to control bowel movements. Most often, it is observed in young children under the age of five, but it also occurs in adults due to injuries, neoplasms and a number of pathological conditions.
Fecal incontinence in adults can manifest itself in varying degrees: from leakage during the passage of gas to complete incontinence. The problem is familiar to 7% of the population and is the cause of serious emotional stress and even the development of depressive conditions. A person feels a loss of control over his body, feels humiliated and cannot adapt to society.
Causes of fecal incontinence in the elderly
What does old age bring?
For many men, with age, the urge to empty the intestinal walls becomes uncontrollable. Feces pass involuntarily, at any time and before visiting the toilet.
The mechanism of development of the pathology is due to a failure in the regulation of the brain center, which ceases to respond to conditioned reflexes, maintain intestinal tone, and retain feces in the rectum until the right moment comes.
It is in old people (unlike women) that pathology more often progresses, when the average sphincter pressure can reach 125 mm/Hg/st, remaining in tension constantly (during wakefulness, sleep).
Normally, mechanoreceptors stimulate the act of defecation in the rectal canal, causing the Valsava reflex and sending signals to the brain that it is time to go to the toilet. With encoporesis, fecal accumulations begin to pass involuntarily. Self-control over the process of defecation is partially (completely) lost. Affected men become unable to hold stones. As a result, gases and stools (hard, liquefied) begin to pass spontaneously.
The main provoking factor is defecation disorder, which is observed in men over 65 years of age.
Other reasons:
Weak from drugs
- chronic constipation;
- abuse of laxatives;
- coelenteric surgery undergone the day before;
- impaired sensitivity of the rectal area;
- hemorrhoids (terminal stage);
- prolonged diarrhea;
- degradation of the nervous system.
Reference! Uncontrollable bowel movements often affect people who have suffered a stroke, multiple sclerosis, brain injury, Parkinson's disease or Alzheimer's disease. The reason can be a congenital anomaly of the pelvic part, obesity, or rectal cancer.
Sphincter incompetence and fecal incontinence in young men can be observed due to stress, fear, depression, and sudden changes in mood. In old people, this is a consequence of damage to the anal apparatus, dysfunctional disorder of the pelvic floor.
complications
Fecal incontinence may lead to further problems as a result of symptoms
- irritation of the skin around the anus,
- emotional and social stress such as fear,
- embarrassment,
- social isolation,
- loss of self-esteem,
- fear
- or depression,
- inability to engage in physical activity,
Anorectal diseases
Stool incontinence in men occurs with external hemorrhoids, when hemorrhoidal cones begin to fall out. The sphincter muscles no longer completely cover the anus. The result is spontaneous leakage of liquid diarrhea with mucus or at the wrong time before a planned trip to the toilet.
Other diseases of the anorectal area:
Intestinal disorders
- Tumor (malignant, benign) of the rectum, sigmoid colon.
- Paraproctitis in case of formation of a fistula, abscess in the perianal area.
- Coccydynia is a consequence of injury to the sacrococcygeal region, causing severe pain in the gluteal region and perineum. A clear sign of the disease is paroxysmal pain, not associated with the urge to defecate.
- Proctitis is inflammation of the mucous membrane of the rectal canal, accompanied by pain. Forms of the disease: catarrhal, ulcerative, fibrous, purulent, necrotic.
Infectious diseases caused by sexually transmitted infections can cause stone incontinence, when patients begin to experience particular discomfort in the anorectal area, constipation alternating with diarrhea, or constant difficulties during bowel movements.
Decreased rectal muscle tone
Normally, in healthy men, the intestine stretches perfectly and retains feces within the limits of what is possible. If muscle tone decreases, the walls of the rectum become inelastic. The muscles no longer adequately stretch and hold stones, causing fecal incontinence.
Causes of decreased muscle tone:
- diarrhea, intestinal disorders;
- Crohn's disease;
- ulcerative nonspecific colitis;
- anorectal surgery;
- radiation therapy.
Dysfunctional pelvic floor disorder
Stool incontinence in men can be a consequence of dysfunction of the muscles (nerves) of the pelvic floor. At the same time, the sensitivity and self-compressive ability of the muscles decreases.
Dysfunctional disorder is a whole complex of pathologies of the pelvic organs, the reasons why in older men:
Accompanying illnesses
- atherosclerosis;
- encephalitis;
- brain tumor;
- Alzheimer's disease;
- weakness of the sphincter muscles;
- nocturnal enuresis;
- prostatitis;
- trauma to the urinary system;
- constipation
The result of provoking factors is a false urge to defecate or uncontrolled passage of feces. The pelvic floor is constantly in a relaxed state or sags, falls out, and the rectum protrudes out of the anus.
How is it diagnosed?
When diagnosing encopresis, the doctor interviews the patient. Knowledge of the characteristics of the course of the disease will help the specialist more accurately determine the type of disorder and prescribe individual treatment. To do this, the doctor may ask the patient the following details about the sensitive problem:
- factors under which defecation occurs;
- duration and frequency of incontinence;
- presence of urge to have a bowel movement;
- stool consistency;
- volume of stool and presence of gases.
At the appointment, the doctor will examine and interview the patient
The development of encopresis can also be influenced by psychological factors or brain damage. Therefore, the doctor will definitely ask the patient about recent emotional turmoil, head injuries, confusion or disorientation in space. The specialist must also know everything about the patient’s diet, bad habits, medications and lifestyle.
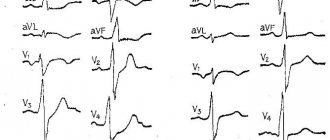
The next stage of diagnosis will be instrumental studies. These include:
- anorectal manometry to determine the sensitivity and contractility of the anal sphincter;
- endorectal sonography, which allows to identify sphincter defects, their tone or pressure in the anal canal;
- MRI of soft tissues of the pelvic area;
- defectography aimed at identifying the volume of feces held back by the intestines and the characteristics of the process of its emptying;
- electromyography, which reveals malfunctions in the nervous system;
- sigmoidoscopy and ultrasound of the rectum, calculating anatomical features or pathological neoplasms in this part of the intestine.
The range of diagnostic measures also includes blood, urine and stool tests. This information is sufficient to prescribe treatment for a patient with encopresis.
First of all, therapy will be aimed at eliminating concomitant pathologies or factors that caused this disorder.
Types of fecal incontinence in older people
Encocution in the elderly has several varieties, differing in symptoms and frequency of intervals of fecal leakage.
Doctors distinguish between incontinence:
- partial, when feces pass out when excessive pressure is applied to the sphincter of the anorectal zone during moments of coughing, sneezing, or lifting heavy objects;
- regular and occurring in severe conditions in older people due to heart attack, stroke, Alzheimer's disease.
Encocution has 4 stages of development:
- Stage 1 – failure to retain accumulated gases inside the rectum.
- Stage 2 - no retention of gases or loose stools.
- Stage 3 - failure to retain gases, liquid and even solid stones.
Reference! Each type of pathology occurs in its own way, so before undergoing treatment, patients must undergo a thorough diagnosis.
What gaskets to use
If earlier encopresis meant constant wearing of diapers, today these products have been replaced by specialized pads with a ureteral catheter. They are conveniently fixed and placed in shorts, which makes life much easier for older people. Also, the positive features of such gaskets include:
- absorption of unpleasant odors using an absorbent layer;
- preventing the proliferation of pathogenic microorganisms due to the antibacterial layer;
- hypoallergenic due to the absence of latex;
- breathability due to the “breathable” component.
Gaskets will help avoid awkward situations
In pharmacies you can find Seni V brand products from a Polish manufacturer. Encopresis is always accompanied by urinary incontinence. Regular diapers are not able to cope with two problems at the same time. Therefore, pad manufacturers advise placing their inserts in a diaper, thereby providing reliable protection from awkward situations. Products of this brand with a catheter are used separately from diapers, facilitating the patient’s movements.
Read more about the treatment of urinary incontinence in adults >>
Products come in two sizes - maxi and normal. They differ in the volume of absorbent surface. The principle of putting them on is similar to regular diapers. But when using them, it is necessary to provide the presence of fixing panties or a urinary catheter.
These products also have their drawbacks. The pads do not have an insulating layer that prevents moisture from reaching the extremities.
We train the intimate muscles of the pelvic floor, Kegel exercises
Physical exercises
It is Kegel exercises that gradually begin to restore the lost functions of the rectal apparatus, train the sphincter and pelvic floor muscles. The complex is developed together with a doctor. The essence of the therapy is squeezing and unclenching the anal sphincter after inserting a rubber tube lubricated with Vaseline into the rectum. The main goal is to train a weakened anal sphincter and muscle to retain feces before going to the toilet.
The course of therapy is 3-8 weeks. Duration of 1 session – 1-16 minutes. Doctors recommend performing up to 5 sessions daily. Additionally, strengthen the muscles of the gluteal region and pump up the abdominal muscles by performing other physical exercises.
diagnostics
The diagnosis is made based on
- story,
- physical examination
- and instrumental exams.
It may be helpful to keep a bowel diary to aid diagnosis. It is a matter of recording the details of fecal evacuation on a daily basis. The physician may provide a form to fill out, or the subject may create their own form on which to write down the details.
The doctor's questions may cause embarrassment and reluctance. However, the doctor will not be upset or surprised. The more the subject can provide details and examples related to his problem, the more easily the clinician can help. Talking honestly and openly about the problem with your doctor makes diagnosis much easier.
Treatment of stool incontinence
Encocution requires an integrated approach to treatment. At the initial stage, when there is slight gas incontinence, it is enough to regularly empty the intestines, review the diet to normalize the functions of the digestive organs and exercise regularly. At stages 2-3 of fecal incontinence, medications and alternative methods are prescribed. In advanced cases, surgical intervention is required.
Medicines can stop prolonged diarrhea, increase sensitivity in the sphincter, improve the condition of the anal muscles, and make men feel better with severe anorectal pain:
Doctor's recommendations
- painkillers (Diphenoxylate, Codeine) to reduce intestinal motility and increase muscle tone;
- drugs to minimize water in feces (Polysorb, Metamucil, Kaopectate);
- anticholinergics containing belladonna, atropine to slow down peristalsis and reduce intestinal secretion;
- tranquilizers, sedatives, sedatives to regulate behavior in psychological disorders in patients leading to uncontrolled bowel movements;
- vitamin complexes (Furazolidone, Imodium).
Medicines are prescribed only by the attending physician based on the results of the diagnosis, the general well-being of the patients, and the type of fecal incontinence.
Reference! Antidiarrheal drugs (Imodium, Loperamide, Proserin) by injection have proven themselves well if loose, watery stools are bothering you.
Other non-drug methods of influence:
- Electrical stimulation
- Biofeedback is a technique using special devices with sensors. The patient begins to hold the external sphincter in a tense state. The received data is displayed on the monitor. The goal of treatment is to achieve long-term contraction of the anal muscles, conscious control over the process of bowel movements.
If medicinal, non-medicinal methods of treatment become useless for fecal incontinence in men, then the only way out is surgery. Especially if the incompetence of the anal sphincter is caused by oncology, a tumor in the rectum.
Surgery methods:
Surgical treatment
- Sphincteroplasty used for rupture (injury) of the muscle ring. The main thing is to achieve sphincter reconstruction.
- An operation by suturing the sphincter muscles to the anus.
- Installation of an artificial sphincter, in which a girdle cuff and an air pump are attached to the anus. The main goal is to keep the anus closed until you go to the toilet and have a bowel movement.
- Colostomy with excision of the affected colon, collection of feces in a colostomy (special bag), opening of the anus and suturing to the anterior wall of the peritoneum.
Psychotherapy plays a significant role in stone incontinence in the elderly, since in old age the pathology is often caused by psychological disorders. The technique is aimed at training a conditioned reflex that is responsible for events and signals the situation in which defecation should occur. Additionally, patients must strictly adhere to the regime of visiting the toilet, at approximately the same time: in the morning after sleep or after eating.
What to do first: lifestyle changes
Comprehensive treatment of fecal incontinence in the elderly always begins with changes in the patient's lifestyle. Before drug therapy, exercise therapy and dietary changes, to cope with the complexities of this disorder, the following tips will help the patient:
- Empty your bowels before each time you leave the house.
- It is better to leave the house 1-2 hours after eating.
- The patient's bag should always contain wet wipes and a change of underwear.
- It is recommended to replace regular underwear with disposable underwear.
- You should always plan your route outside the house in advance, inquiring about the location of the toilet rooms.
Also, to get rid of the unpleasant odor of gases or feces, you can purchase special medications at pharmacies.
Fecal incontinence in the elderly
Unfortunately, fecal incontinence, cortical dysfunction, and psychiatric disorders are common in older men. This is an acquired condition when bowel movements become involuntary up to 5-6 times a day. To obtain beneficial results, the relatives of a sick man suffering from nervous disorders and decreased memory should play a significant role. The help of loved ones is invaluable in attention, hints, and commands when the patient needs to visit the toilet, adhering to the established regime.
Often, old people lose partial (complete) mobility and, for physical (neuroparalytic) reasons, do not feel the urge to defecate. It may be necessary to monitor diaper changes in advance and train them to show reactions to going to the toilet after eating, immediately after waking up.
A big role in stool incontinence is given to a diet with foods containing plant fiber to increase the volume of softened fecal deposits. It is important to exclude alcoholic and carbonated drinks, coffee, milk, spices, salt, and smoked foods. You need to drink at least 2 liters of clean liquid per day.
It is important to protect elderly patients from stress, anxiety, and negative situations. Constantly train the sphincter and pelvic floor muscles through simple exercises.
When to see a doctor
It is recommended to consult a doctor if:
- You are experiencing fecal leaks that cannot be checked,
- panties get dirty without feeling the need to defecate,
- traces of feces are lost during flatulence,
- the disorder affects the patient's life from a social/psychological perspective.
Please note that an occasional episode, perhaps during intestinal distress due to diarrhea, is not a cause for concern and can happen to anyone; Although some subjects may cope with mild or sporadic incontinence problems, it is helpful to consult a physician if urinary incontinence is altering quality of life or causing emotional or social distress.