Frostbite may occur with prolonged exposure to low temperatures. In most cases, this phenomenon is accompanied by general hypothermia of the body, which aggravates the situation.
The least protected areas are affected first - the face, ears, fingers and toes. It is quite natural that most people get frostbite during the cold season. At the same time, it is not at all necessary to be outside for several hours in a row at very low temperatures. If unfavorable factors coincide, frostbite can occur even at a temperature of 0 C. Adverse weather factors include: wind; high humidity; low degree of human protection from the cold.
When to suspect frostbite
If you go outside and feel that some part of your body that is exposed or poorly protected from the cold is freezing or already hurting, this does not always indicate frostbite. To do this, it is necessary that the air temperature be below minus 10°C with little humidity, or 0°C or lower - in combination with a wind of more than 5 m/s and high humidity. If a person’s clothing does not allow for normal heat exchange and prevents the removal of sweat, or is too light, or is wet, frostbite can develop even at +8°C.
Frostbite can affect the entire face or parts of it: cheeks, nose, ears. Doctors make the same diagnosis when hands in insufficiently warm gloves or feet in light or tight shoes, which in themselves impair blood circulation, are exposed to cold. If pain, numbness and a feeling of cold are felt throughout the body, this is called general hypothermia and is treated separately.
You are more likely to get frostbite if:
- the person went out hungry (he ate more than 8 hours ago);
- he is in the cold in a state of alcoholic intoxication (the blood vessels are dilated - more heat is lost);
- a person has to stand motionless for a long time or hold (carry) some object in the cold;
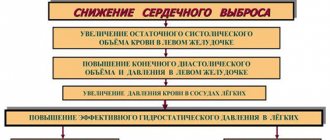
- a person suffers from diabetes mellitus or diseases in which there is a violation of general (heart failure, systemic vasculitis) or local (Raynaud's syndrome, obliterating atherosclerosis or endarteritis, varicose veins) blood circulation;
- he is physically exhausted (overworked or just suffered a serious illness);
- he lost some blood;
- this is a child, a pregnant woman (especially in the 3rd trimester) or an elderly person.
These people need to proceed to the algorithm described below at the slightest discomfort in the face and limbs.
The degree of frostbite (that is, the depth to which the cold influence has penetrated) can only be assessed in a warm room, but not immediately, but over several hours.
First aid for frostbite
In case of damage of any intensity, it is first necessary to deliver the victim to a warm room as soon as possible. If there is a possibility of re-frostbite, the damaged part of the body should not be allowed to thaw; otherwise, you should cover it carefully. Further measures depend on the degree of frostbite.
For frostbite of the first degree you need:
- warm the affected areas of the skin (by breathing, gentle rubbing with a soft woolen cloth or hands);
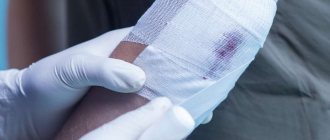
- apply a warming cotton-gauze bandage in several layers.
For frostbite of II–IV degree you need:
- exclude rapid warming (massage, rubbing);
- apply a heat-insulating bandage (bandage and cotton wool in several layers, you can use scarves, wool, shawls);
- fix the frostbitten limb;
- call an ambulance team.
It is recommended to give the victim a hot drink and food; you can take Aspirin, Analgin with Papaverine or No-shpa to improve blood microcirculation.
Actions to be performed while still on the street
The algorithm consists of several simple steps.
1. If you suspect frostbite on your face, immediately begin to warm yourself while walking to your destination, which is located indoors:
- put on a hood or hat if your ears are cold;
- if your nose is frostbitten, either pull up the collar of your sweater/jacket to hide your nose under it, or tie a scarf so that it covers your nose. You can cover your nose with gloved hands;
- the previous paragraph is also suitable for reducing the degree of tissue damage due to frostbite on the cheeks.
If your hands are very cold, put them in your own armpits (as if you were hugging yourself). If your feet are cold, start actively wiggling your toes.
2. If you are far from home or your destination, go to the nearest entrance, store, shopping center, pharmacy, clinic, educational institution or other premises. The best option: stay in the room for at least 10 minutes, drink hot tea or coffee there. If your feet are frozen and along the way you see a store where you can buy an extra pair of socks, be sure to do so: treatment for frostbite on your feet costs more than even a pair of woolen socks.
3. On the way to the room, move actively: you can wave your arms (as during exercise), clap your hands, run, or walk, stamping your feet (you can raise your legs high). This will help increase overall blood circulation and reduce the extent of local damage.
Do not rub snow on a frozen and reddened part of the body under any circumstances: this can cause additional damage to the tissues in which blood circulation is currently affected.
Mistake two: smearing something greasy
Also, many people think that they can lubricate the frostbitten surface with something greasy and nutritious so that the damaged surface can be restored faster.
“Fat forms a film that clogs pores and disrupts the natural thermoregulation of the skin. One of the main functions of the skin is thermoregulation, both warming and cooling. Fat forms a dense film that disrupts this process, and the superficial part of the skin will not work as it should,” notes Rustam Merdalimov.
What to do immediately upon arriving home
Frostbite is not a one-time process. Initially, low temperature leads to vasospasm, then the blood supply is reversibly disrupted. If the cold continues to act, blood clots form in these vessels, and blood circulation can be completely stopped. Products of dying tissue enter the bloodstream and cause poisoning of the body.
The entire process of frostbite is divided into 2 periods:
- hidden : begins on the street and continues for some time after warming up;
- reactive (explicit) : appears only after warming for 6-12 hours.
By the appearance of the frostbitten area in the reactive period, it will become clear what degree of cold burn you have. And in order for fabrics:
- warmed up faster;
- pathological changes did not spread deeper than what had already happened in the cold (this can happen to underlying tissues when they are cooled by a large array of highly chilled tissues from above),
- it became clear how serious everything was,
You need to do the following in a warm room:
- if your hands or feet are frostbitten, start moving them to restore blood circulation;
- the second thing to do is take off cold or wet clothes;
- find an alcohol thermometer and start pouring warm water into a basin or bowl, making sure it is 26-28°C;
- simultaneously put a kettle of water on the fire or turn on the electric kettle;
- in case of frostbite on the nose, ears, cheeks or cheekbones, while water is being collected, apply a warm palm to the affected area;
- when the water has accumulated, dip the affected area into it: if your fingers are frostbitten, immerse your hands in it for 10 minutes, do the same with your feet. If your ears, nose or cheeks are frozen, soak a clean cloth in this water and apply to the affected areas;
- the temperature of the water with which you warm the affected area must be gradually and very carefully increased: it should reach 37 degrees in 40 minutes;
- if there is no warm water, you can:
- or wrap the areas in foil, the shiny side inward;
- or wrap the frostbitten area in a thermal blanket;
- or cover the diseased area with a heating pad, first checking that the temperature it creates at the minimum level does not exceed 30°C. Then, as in the case of water, you will need to gradually increase the temperature;
- d) alternatively, you can immediately resort to point 10, and after it follow point 9;
- At the same time as you warm the affected area, start drinking warm and sweet tea. If you have frostbitten fingers, it is better to pour the tea into a bowl so that you can hold it with your palm rather than bend your fingers;
- After warming up, apply a heat-insulating bandage to the frostbitten area. It consists of 5 layers:
- closer to the skin - gauze;
then - a large piece of cotton wool (especially in case of frostbite of the ear, the cartilage of which has a rather poor blood supply);
- gauze again;
- oilcloth or polyethylene;
- wool fabric.
- You may feel either cold or hot, so wrap yourself in a warm, dry blanket and drink another cup of warm sweet tea.
If one or both ears are frostbitten, fixation with a bandage or woolen cloth is carried out around the head;
What not to do if you have frostbite
- warm the frostbitten area near the fire, touch it to the battery, put it under hot water;
- apply greasy ointments (this should be done before going outside, and not after an accident has occurred);
- If blisters appear on the skin soon after warming up, they should not be opened. You can only apply a sterile bandage (if you have a sterile bandage or sterile wipes at home), and then consult a doctor;
- rub with snow, ice and even mittens: this will further injure the vessels of the affected area;
- drink alcohol;
- rub the frostbitten area with alcohol. If you apply it and rub it gently, the heat will evaporate from the surface of the skin. If you rub the frostbitten area with alcohol, you can damage the fragile vessels in this area.
What should you not do if you have frostbite?
Absolutely forbidden:
- rub the frostbitten surface with snow or a hard cloth (there is a high probability of injury and subsequent infection of the damaged skin);
- expose the frostbite site to intense heat (using a hot bath, heating pad, heater, etc.);
- rub damaged skin with oil, fat, alcohol, as this can complicate the course of the disease;
- open the blisters yourself and remove necrotic tissue.
Actions that are important to complete within the next 6-12 hours
If within an hour the frostbitten area has warmed up, but the skin on it has acquired a bluish or red-purple tint and has swollen a little, and the area itself has begun to hurt, do not be alarmed. This is the first degree of frostbite. It can be treated at home. For pain, take any painkiller to which you are not allergic: Ibuprofen, Analgin, Diclofenac. This medicine can be taken several times on the first day, but so that the maximum dosage (as indicated in the instructions) is not exceeded.
If you experience the symptoms described, it does not mean that the danger has completely passed. You must continue to monitor the frostbitten area. If on the 2nd day 1 or more blisters appear at the site of swelling, this is degree 2 frostbite. Bubbles cannot be opened. You need to consult a combustiologist (these are specialists working in burn departments of multidisciplinary hospitals) or a general surgeon at a clinic.
What to do after frostbite, if 2 hours have already passed and you do not feel the affected area (it seems to be numb), or the skin on it remains white, you need to contact a surgeon at the clinic or a doctor at the burn center. This could be 3rd or even 4th degree frostbite. They must be treated in a hospital: only there is it possible to administer medications using IVs that:
- can improve blood supply to the affected area, thereby reducing the affected area;
- will help dissolve blood clots in the affected area;
- will prevent suppuration of frostbitten tissues or reduce its severity.
Unfortunately, medications that can do this efficiently only exist in the form of injections or droppers. In addition, the hospital will monitor your condition and your wound around the clock. If it turns out that you have stage 4 frostbite, when the damage has affected all layers of soft tissue, measures will be immediately taken to remove dead tissue and stop the spread of necrosis even deeper or further (for example, from fingers to hands).
In the hospital, a person’s blood will also be taken to determine the degree of his immune protection against tetanus (the test is called “Blood for antibodies to tetanus”) and without waiting for the test result (especially if the ADS vaccination was performed more than 5 years ago or there is no information about when it was carried out similar vaccination), he will be given the necessary antitetanus drug. This will help avoid the development of tetanus, an infectious disease with a high mortality rate, since frostbite creates optimal conditions for the development of tetanus bacteria in the wound.
Actions to be completed the next day
The next day it will be more clear what degree of frostbite a person has:
- If no bubbles appear - 1st degree. Only the skin is affected.
- When blisters (or one bubble) filled with transparent contents appear on purple or bluish-colored skin, and the area itself is very painful – grade 2. The skin and partially subcutaneous tissue are affected.
- If the affected area remains pale and cold, the sensitivity on it is reduced or absent, and against this background, blisters filled with bloody contents appear - grade 3. If your fingers or toes are frostbitten, their nails peel off and then do not grow back. Grade 3 indicates damage to the skin, subcutaneous tissue and muscles.
- When the skin becomes bluish-marbled or even black, swollen, does not feel touch or even needle pricks, and the joints under such tissues do not move (“do not obey”), this is the 4th degree of frostbite. All layers of muscle are affected, as well as tendons and possibly bones.
Help for frostbite can be provided to yourself (or a relative) at home only in the first two stages. Stages 3 and 4, which you can accurately determine on the second day after frostbite, are treated only in a hospital. Staying at home in these cases is dangerous: you can develop gangrene, get tetanus or blood poisoning; from a large number of decaying tissues that are absorbed into the blood, acute renal failure can develop - a condition no less fatal than the others.
So, what to do if your fingers or other areas are frostbitten during stage 1-2 of frostbite:
- if pain is felt, take painkillers (Diclofenac, Ibuprofen, Dexalgin and others) without exceeding the maximum permitted dosage. You need to take these tablets after meals. If you suffer from gastritis or peptic ulcer, you must take Omeprazole (Omeza), Nolpaza, Pantoprazole or Ranitidine while taking painkillers;
- if nothing hurts, but you measured your temperature and it turned out to be above 38°C, take Paracetamol. If you are already taking a painkiller, it will reduce the temperature, and taking two similar drugs at once increases their toxic effect on the kidneys and gastrointestinal mucosa;
- To speed up the restoration of normal blood flow in the damaged area, take No-shpu (Drotaverine) or Papaverine. They will dilate blood vessels, which will provide better nutrition to diseased areas;
- In parallel with taking No-shpa or Papaverine, you will need to use drugs for several days that will destroy blood clots that have formed in the frostbitten area. These are ointments “Lioton”, “Gepatrombin”, heparin gel. If you do not take painkillers or antipyretics (this is one group of drugs), you can use Aspirin at a dose of 75 or 100 mg once a day after meals to prevent the formation of blood clots;
- for itching, antihistamines are needed: “Fenistil”, “Erius”, “Diazolin”;
- to speed up the process of impulse transmission from nerve to muscle in damaged areas, B vitamins are needed: Neurorubin, Milgamma, Neurovitan. Nicotinic acid is also used in tablet form.
All medications have contraindications, so consult your doctor before taking them.
Local treatment is also necessary. So, to speed up healing with the 1st degree of frostbite, treat the areas with Bepanten (Dexpanthenol) cream, and when going outside or if you need to wash frostbitten hands, apply an emollient to them an hour before: “Physiogel”, “Mustella stelatopia” or any other drug. If you are treating frostbite of the 2nd degree, treat the blisters with an antiseptic without alcohol (Chlorhexidine, Miramistin, a weak solution of potassium permanganate) or with alcohol (a solution of brilliant green or fucorcin). Apply Levomekol ointment around them. When the bubble opens on its own, you can treat the entire affected surface with Levomekol.
Be sure to lightly massage the affected area. You can do this while you apply the cream or ointment. Massage movements bypass the area of opened blisters; they can be performed with sticks wrapped in sterile cotton wool.
What not to do
Having noticed that frostbite has occurred on the toes, you need to act, observing the above procedure for providing assistance. You should not make mistakes that can aggravate the damage and provoke complications.
Common ones are:
- rubbing your fingers with lumps of snow;
- warming up in hot water or near a fire;
- lubricating frostbitten areas with medical alcohol, vegetable oil or fat;
- intensive massage;
- drinking alcohol to stay warm.
Even if mild frostbite occurs, you should consult your doctor and follow his instructions during therapy.
Actions to be completed in a week
Recovery from 1st degree frostbite occurs within 5-7 days, without scar formation, but goes through the peeling stage. All this time you:
- take B vitamins and xanthinol nicotinate preparations (if approved by your doctor);
- if there are no contraindications, take Aspirin for 5-7 days;
- lubricate the affected skin with Bepanten (if your hands are very dry and flaky, you can no longer use the cream, but the thicker Bepanten ointment);
- treat itching with antihistamines;
- massage the affected areas.
If frostbite has reached degree 2, when recovery lasts about 2 weeks, treatment is as follows:
- taking painkillers with a gradual reduction in dosage;
- local treatment with Levomekol;
- taking B vitamins;
- if the itching is severe, you can not only take an antihistamine, but also apply Fenistil-gel or Psilo-balm to the itchy areas (if it is not the area under the opened blister). If this does not help, contact your surgeon, who may recommend a topical hormonal medication;
- you need to massage the affected area, bypassing the wounds formed after opening the blisters.
At grade 3, the wound will take more than a month to heal, most of which you must spend either in a hospital or as a day hospital with daily examinations by a combustiologist or surgeon. Treatment will be carried out using injections and droppers, as well as professional treatment of the wound with special solutions. After healing, scars form, which can subsequently be treated with Contractubex or other recommended drugs.
Frostbite of the 4th degree must be treated in a hospital, where, if necessary, either amputation is performed, or only the removal of dead tissue without removing the underlying bone. Treatment takes more than a month only in a hospital. The doctor will tell you how to be treated later, depending on the current situation and concomitant diseases.
Please note that frostbitten areas will need to be protected much more carefully from both high and low temperatures over the coming year to achieve complete tissue healing.
Causes of frostbite of extremities
Frostbitten hands, fingers or feet can be caused by the following factors:
- Tight shoes, wet clothes.
- Increased air humidity.
- Presence of wind.
- Forced immobility at low temperatures.
- Diseases of the heart and blood vessels.
- Physical fatigue.
- Chronic vascular diseases of the extremities.
- Significant blood loss.
- General relaxation due to a significant dose of alcohol.
- Smoking.
- Asthenic condition after infections.
- Previously suffered frostbite.
When to see a doctor
This should be done as soon as possible in such situations:
- when warm, lips have a bluish tint;
- an elderly person or child was injured;
- the victim lost consciousness;
- breathing becomes heavy or extremely weak;
- human body temperature – either below 34°C or above 38°C;
- heart rate more than 100 per minute or less than 60 per minute;
- the victim’s consciousness is confused, he expresses delusional ideas;
- 2 hours after complete warming, the frostbitten area remains cold and insensitive, or blisters filled with blood have already appeared on it;
- nausea or vomiting developed;
- convulsions appeared;
- the amount of urine has decreased despite the fact that you drink 30 ml/kg/day;
- the frostbitten area is larger than the area of your own palm (1 palm = 1% of the body surface).
The first mistake is to rub it with snow
It would seem that the snow outside is at hand, and the first thing that comes to mind is to actively rub it on the damaged area to “disperse the blood.” In reality, experts say, there is no need to do this. “First of all, snow is a solid form of water. It has a crystalline form, and when rubbed on the skin, it acts like an abrasive. That is, there is a high chance of damaging the surface layers of the skin. It's actually like fine sandpaper. Secondly, snow is also cold and can itself cause hypothermia. Well, plus everything, the snow, especially in large cities, can be called clean very conditionally,” says Rustam Merdalimov.