Pneumococcal infection is a complex of pathologies that develop mainly in children and manifest themselves with a variety of clinical symptoms. This is an acute anthroponosis with an airborne pathogen transmission mechanism, caused by pneumococcus and affecting the ENT organs, lungs and central nervous system . Thanks to mass vaccination of the population and the introduction of pneumococcal vaccine into the National Immunization Program, the incidence of pneumococcal infection has significantly decreased and the number of carriers of Streptococcus pneumoniae has decreased.
The group of pneumococcal infections includes inflammatory diseases of the lungs, meninges, middle ear, endocardium, pleura, joints and other organs.
Pneumonia is the most common clinical form of pathology , which is a complication of other diseases - influenza, measles, otitis media, ARVI. Pneumococcal pneumonia is one of the most common causes of child mortality. Epidemics and pandemics of influenza have always been characterized by the severe condition of patients and a large number of deaths caused by pneumococcal pneumonia. Antibacterial control of infection has only been effective for a short time. Gradually, the bacteria lost their sensitivity to antibiotics and became completely resistant to most of them. There is a need to create and develop vaccines.
Today, pneumococcal infection leads the world in the development of diseases of the upper respiratory tract and bronchopulmonary pathology. In our age of high technology, mortality from these pathologies still remains high. The pneumococcal vaccine will help prevent the development of serious illnesses that can cause life-threatening complications.
Etiology
The causative agent of the infectious process is pneumococcal bacterium. The main carrier of the infection is an already infected person. Therefore, if one person in the family becomes ill, the pneumococcal infection can quickly spread to the rest of the family members.
The risk group includes the following categories of people:
- children under 2 years old;
- have suffered from chronic infectious or inflammatory diseases;
- with diabetes and other diseases that cause metabolic disorders;
- survivors of cancer;
- people over 65 years old;
- persons with alcohol and drug addiction.
Most often, pneumococcal infection occurs in children and the elderly. This is due to the fact that the immune system is too weak, and a person’s susceptibility to infection is high.
Pneumococcal infection can provoke the development of the following diseases:
- meningitis;
- pneumonia;
- otitis;
- blood poisoning.
Prevention of pneumococcus
Prevention of pneumococcus includes the following recommendations:
- Follow the rules of personal hygiene - do not forget to wash your hands and brush your teeth more often;
— During epidemics of acute respiratory infections, after going outside, rinse your nose and oropharynx with a slightly salted solution;
— Strengthen your immune system;
— Try to eat foods enriched with vitamins and microelements;
— In cold weather, dress warmly to avoid hypothermia;
— Do wet cleaning at home 2-3 times a week, ventilate the room more often;
— Don’t forget to clean the filters of air conditioners, air purifiers, and vacuum cleaners;
— Move more, toughen up (if there are no contraindications);
- Avoid stress;
— Don’t forget to get proper rest, get enough sleep;
— Do not leave possible foci of infection to chance - inflamed tonsils, dental caries;
— During acute respiratory infections, avoid places with large crowds of people, especially indoors;
— If there are sick people at home or at work, do not share dishes or personal hygiene items with them.
— Follow the rules for the prevention of acute respiratory viral infections and acute respiratory infections;
— Individuals at risk of pneumococcal infection and children are recommended to receive the pneumococcal conjugate vaccine (PCV).
General symptoms
Symptoms of pneumococcal infection depend on the location of the infectious process. On average, the incubation period can last from 1 to 3 days. It all depends on the general state of health, the etiological factor and the age of the person. If we consider the clinical picture in general, we can distinguish the following symptoms:
- unstable body temperature;
- rash on the body;
- neurological disorders;
- headache;
- labored breathing;
- chills, fever;
- dyspnea;
- photophobia.
Symptoms of pneumococcal infection
Pneumococcal infection in children can be accompanied by the following symptoms:
- moody state, irritability;
- refusal to eat, loss of appetite;
- nausea;
- a sore throat.
Due to the fact that the symptoms clearly indicate influenza or ARVI, patients do not seek medical help in a timely manner. Therefore, there is a significant risk of complications. Pneumococcal infection in children requires immediate medical intervention and correct treatment.
Factors favorable for the development of pneumococcal infection include the following:
- systematic hypothermia;
- frequent exposure to stressful situations;
- respiratory infections;
- hypovitaminosis.
At the first symptoms, you should immediately consult a doctor. If treatment is started in a timely manner, significant complications can be avoided. There is no need to wait until the infection reaches a critical point of development in the body. Such a delay is fraught with serious complications in the functioning of the kidneys, liver, and cardiovascular system.
The effectiveness of vaccine prevention
The effectiveness of any preventive measure, including CAP, is the degree to which the desired result is achieved through the implementation of this measure in the absence of side effects or their presence within established limits. The epidemiological, economic and social effectiveness of VP are highlighted.
The epidemiological effectiveness of CAP is determined by the degree of its influence on the epidemic process and is manifested in reducing morbidity and preventing the occurrence of new cases of infection among the population. When considering the epidemiological effectiveness of an event, it is customary to evaluate its potential and actual effectiveness.
The potential effectiveness of the VP is assessed by 2 main indicators: the efficiency index and the efficiency coefficient, or security indicator.
The index of the effectiveness of VP against a particular infection is the ratio of morbidity rates in the group of those vaccinated and those not vaccinated with this drug. It shows how many times the incidence rate of vaccinated individuals is lower than that of unvaccinated individuals.
The effectiveness coefficient characterizes the proportion of vaccinated individuals whose protection from infection was ensured by vaccination with this drug. The effectiveness coefficient is the most preferable indicator, since it shows only the effect of vaccination, without the influence of other preventive factors that may occur in the control and experimental groups.
The actual epidemiological effectiveness of CAP is determined by the actual reduction and prevention of morbidity as a result of CAP with a specific drug according to a specific regimen. The actual epidemiological effectiveness of VP is assessed during the period of its mass use. Assessing the actual effectiveness of EP is not a one-time study, but an ongoing analysis during epidemiological surveillance of infection, being a component of operational and retrospective epidemiological analyses.
The potential epidemiological effectiveness of VAP depends primarily on the immunogenicity of the vaccine, as well as on the choice of vaccination tactics and vaccination schedule.
The actual epidemiological effectiveness, assessed in real practical healthcare conditions with mass CAP, is usually lower than the potential effectiveness tested with optimal organization. The actual effectiveness is largely determined by the quality of the drug used and the quality of the organization and conduct of the event. The greater the difference between potential and actual effectiveness, the more reasons to doubt the quality of the means and measures and strengthen control over the EP. However, differences in effectiveness may be due to other reasons, for example, changes in the epidemiological situation, the evolution of the epidemic process of infection, which require changes in vaccination tactics.
The epidemiological effectiveness of VP PI has been assessed in numerous studies. Evidence in favor of the epidemiological effectiveness of vaccination is the decrease in the incidence of PIs in general and individual infections, primarily iPIs, recorded in various regions of the world.
Pneumococcal pneumonia
Pneumococcal infection can cause pneumonia. The following symptoms may occur:
- chills, shortness of breath, shallow breathing;
- temperature – up to 40 degrees;
- muscle weakness;
- arrhythmia or tachycardia;
- pain in the chest area when coughing;
- cough with purulent mucous discharge.
If the disease is provoked by pneumococcal infection, then a distinction is made between focal and lobar pneumonia. The croupous form of the disease is much more severe. There is a significant risk of complications:
- pulmonary failure;
- pleurisy;
- abscess development.
The focal form, with timely treatment, does not cause significant complications. But the infiltration period lasts somewhat longer - up to 4 weeks.
Causes and pathogenesis of the disease
Pneumococcus most often causes inflammation of most of the lung lobe, and sometimes the entire lobe. But often pneumococcus becomes the root cause of focal pneumonia.
The medical literature describes four pathological phases of the course of lobar pneumococcal pneumonia.
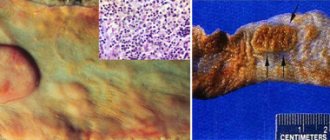
1. Flushing phase, microbial swelling, redness. It is characterized by significant filling of blood vessels and strong exudation of serous fluid. Pneumococci are detected in the exudate. This phase lasts 12-72 hours.
2. Red hepatization phase. It is characterized by complete filling of the alveoli with exudate in that part of the lung that is affected by the disease. Moreover, plasma proteins (fibrinogen) are determined in the exudate, and, as a consequence of diapedesis, the number of red blood cells is increased. The area of the lung in which there is inflammation is airless, dense, acquires a reddish color and looks like the liver. The duration of this period is 1-3 days.
3. Gray hepatization phase. In this phase, significantly more leukocytes are detected in the exudate from the alveoli (mostly neutrophils), but red blood cells are significantly reduced in number. The lung, as before, is dense, grayish-yellow on the section, the granularity of the lung is very noticeable. As a result of microscopic tests, an increase in neutrophilic leukocytes and phagocytosed pneumococci is determined. This phase lasts 2-6 days.
4. Resolution phase. At this time, exudate is steadily dissolving in the alveoli. The reason for this is the influence of macrophages and leukocytes. Fibrin dissolves slowly, and the lung tissue ceases to be granular. Over time, the lung tissue regains its airiness. How long this period will last will depend on how widespread the inflammatory process is, the reactivity of the body, as well as the methods of therapy and how intensive the treatment is.
But you need to keep in mind that the disease does not always go through all these stages sequentially. Most often, in the affected lobe of the lung there are signs of several stages in combination with each other, or signs of one of the phases predominate. It is important to remember that in the case of pneumonia, pathological changes occur not only in the alveoli and interstitial tissue. The pleura, regional lymph nodes, and lymphatic vessels are affected. When diagnosed with “focal pneumonia,” the inflammation process covers a segment or lobule. At the same time, zones of compacted affected tissue alternate with areas of vicarious emphysema. Mostly serous exudate is found. It can often be purulent and contain small amounts of fibrin.
Pneumococcal meningitis
Meningitis caused by pneumococcal infection is characterized by the following symptoms:
- body temperature rises sharply to 40 degrees;
- shortness of breath, difficulty breathing even at rest;
- headache;
- muscle pain;
- nausea and vomiting;
- confused consciousness.
In some cases, partial paralysis may be added to the general list of symptoms. In more severe clinical cases, the patient may fall into a coma.
In children, symptoms are accompanied by almost continuous crying. You should immediately consult a doctor or call an ambulance. Treatment of meningitis requires only qualified medical care and hospital care.
If the patient is not provided with timely medical care, the development of serious complications and even death is possible.
Radiology data
During the stage of compaction or hepatization, the most striking changes in the lung tissue are determined. Lobar pneumonia is characterized by very intense darkening of the lobe of the lung. During a tomographic examination, inflammatory infiltration is observed, and the bronchi are clearly visible against its background. This symptom reliably distinguishes between pneumonia and pulmonary atelectasis. Local consolidation or focal shadow reveals focal pneumococcal pneumonia.
Pneumococcal sepsis
Pneumococcal sepsis is one of the most complex diseases caused by this infection. The clinical picture in this case is as follows:
- unstable body temperature;
- weakness;
- severe headaches;
- enlarged spleen.
The last symptom quite often goes unnoticed by the patient, so the person does not consult a doctor in a timely manner.
Since blood poisoning occurs with toxins, a person may be in a state of shock. Often the general clinical picture is accompanied by neurological disorders. Pneumococcal sepsis can cause serious complications in the functioning of the cardiovascular system, kidneys and liver.
Laboratory research
The most obvious and indicative changes are in the results of a general blood test. Most often, leukocytosis is strongly manifested - leukocytes increase to 20-30x109 / l, it is determined that the level of neutrophils is much higher than normal, the leukocyte formula is very shifted to the left (to myelocytes and promyelocytes). During the peak of the disease, eosinophils disappear, much less than the norm of lymphocytes and platelets. When the final stage comes, the number of lymphocytes, eosinophils and platelets returns to normal. An increase in ESR is very significant. A biochemical blood test shows symptoms of inflammation: slightly higher levels of a- and y-globulins, seromucoid, sialic acids, fibrin, haptoglobin.
Complications
Diseases caused by pneumococcal infection can have serious complications.
For pneumococcal meningitis it is:
- cerebral edema;
- disorders of brain activity.
Not an exception is the cessation of cardiac and pulmonary activity, which entails death.
As for sepsis caused by pneumococcal infection, almost any complications are possible. The lethal outcome is 50% of the total number of patients.
It should also be taken into account that after suffering an illness caused by a pneumococcal infection, the patient’s immunity is too weakened. The latter does not exclude re-infection.
Diagnostics
Pneumococcal infection requires careful and rapid diagnosis. This is due to the fact that bacteria of this type die very quickly in the open air.
After examining the patient and clarifying the medical history, additional diagnostic methods are carried out. The standard program includes the following:
- general examination of urine and blood;
- bacteriological tests;
- throat swab;
- cerebrospinal fluid puncture;
- CT;
- MRI;
- Ultrasound of the chest.
Cerebrospinal fluid puncture
In the event that the above research methods are not enough to make a final diagnosis, differential diagnosis is carried out.
Based on the results obtained, the specialist can determine the disease and prescribe the correct treatment.
Treatment
Several methods are used to treat pneumococcal infection:
- etiotherapy - based on the use of antibacterial drugs;
- pathogenetic infusion therapy;
- symptomatic.
If the course of treatment is based on pathogenetic infusion therapy, then the following drugs are prescribed:
- cardioprotectors;
- mucolytics;
- diuretics;
- medications for general strengthening of the immune system.
Symptomatic therapy includes taking the following medications:
- antihistamines;
- anti-inflammatory;
- antipyretics;
- analgesics.
In addition to taking medications, treatment involves bed rest (inpatient) and diet. There are no special restrictions on the diet. The main thing is that the patient’s diet during treatment and rehabilitation is balanced - with a full range of vitamins and essential minerals.
Timely treatment is already half the success. Therefore, you should seek medical help in a timely manner and do not ignore the doctor’s instructions.
Folk remedies
Before using traditional medicine recipes, you must consult your doctor. Such treatment methods can only act as auxiliaries against the background of primary drug therapy. If the doctor approves, then in addition to taking medications, you can use the following folk remedies:
- Pour 200 ml of water into the pan and add 100 g of raisins. Bring the liquid to a boil, simmer over low heat for another 10 minutes. Next, strain the solution, squeeze the raisins through cheesecloth. Use the product throughout the day. Repeat daily until recovery.
- Mix equal parts of the following herbs: St. John's wort, oregano, birch buds, cyanosis root, angelica and elecampane, motherwort, meadowsweet, eucalyptus and dill seeds. Grind the ingredients, then pour two tablespoons of the mixture into 0.5 liters of boiling water, let it brew, then strain. Drink ¼ glass up to 3 times a day.
- Prepare 2 tbsp. l. thyme herbs. Steam them with a glass of boiling water, cover and leave for about 3-4 hours. Strain before use. Drink 1 tbsp. l. three times throughout the day.
- Mix 2 tbsp. l. dried raspberries, lingonberries and rose hips. Pour a glass of boiling water over the ingredients and simmer in a water bath for 15 minutes. Drink half a glass in the morning and evening. The product should be warm.