Lactase deficiency: signs and help for the baby
In our country, 2-3 adults per 100,000 population and 8-9 children fall ill with meningococcal infection every year. The World Health Organization (WHO) is closely monitoring the disease, and for good reason. The fact is that the mortality rate from meningococcal infection remains very high: every tenth sick adult and every third child under five years of age dies in the world. Children under one year of age die especially often.
Classification
According to clinical manifestations, meningococcal infection is divided into the following types:
- Localized - meningococcal carriage (asymptomatic presence of meningococcus on the nasopharyngeal mucosa), nasopharyngitis.
- Generalized - meningitis, meningoencephalitis, acute, typical, chronic forms of meningococcemia, as well as a mixed generalized form (meningitis and meningococcemia).
- Rare forms - meningococcal arthritis (synovitis), polyarthritis, pneumonia, endocarditis, iridocyclitis.
According to the severity of the disease, it is divided into mild, moderate-severe, and severe forms. Separately, there is a hypertoxic form of meningococcal infection, which is also called the “lightning killer”. The patient's condition quickly deteriorates: the temperature rises to +40 C, a rash appears before our eyes, convulsions appear, blood pressure drops, and the person may lose consciousness. The lack of emergency medical care leads to infectious-toxic shock, coma and inevitable death.
Bacteria living in the nasopharynx
The statistics are impressive: 20% of people are carriers of the causative agent of meningococcal infection! Every fifth! So far, scientists have not figured out why in most cases the bacterium is limited to “registration” on the mucous membrane of the nose and pharynx, but does not penetrate into the blood and does not cause a typical disease. However, it is clear that it is this huge legion of carriers that allows the infection to survive and spread.
Fact: in the nasopharynx of one person, meningococci live for 2-3 weeks, in rare cases longer, then disappear, only to appear again after some time.
The meningitis bacterium (meningococcus) is called Neisseria, more precisely, Neisseria meningitidis. It is quite large - standing out when talking, sneezing and coughing, it does not fly far, it “falls” almost next to the wearer. Neisseria quickly dies when exposed to the sun, drying out and temperatures below room temperature. Weak disinfectants, for example, half-percent hydrogen peroxide, cope with the infection in a couple of minutes. Meningococcus loves to bask in warm, damp mucus - it is quite comfortable there.
Symptoms
Meningococcal infections have pronounced symptoms with the exception of mild forms of nasopharyngitis and meningococcal carriage. In the latter case, the person can be called conditionally healthy, since there are no complaints or clinical signs. The carrier, usually an adult, poses a threat to his environment, especially to children who are seriously susceptible to infection. On average, according to statistics, the carriage period is from 15 to 20 days.
Symptoms of acute nasopharyngitis
- Low-grade fever.
- Nasal congestion causing nasal speech.
- Sore throat, swelling, pain when swallowing.
- Paleness of the skin.
- Loss of energy, loss of appetite, headache.
Sometimes the disease manifests itself as vestibular disorders, resulting in dizziness, tinnitus, and nausea. There is no sneezing or coughing; sometimes there may be mucopurulent discharge from the nose. In general, the symptoms resemble acute respiratory infections, so it is important to carry out a differential diagnosis. On days 5–7, recovery occurs or the disease transitions to a generalized form.
Meningococcemia (meningococcal sepsis)
- Sudden onset of the disease, accompanied by a rise in temperature to +40 C.
- Severe headaches, photophobia, convulsions, vomiting.
- A pink or pink-red papular-type rash appears within 1–2 days. Spots of various sizes from 5 to 20 mm.
- Rigidity of the neck muscles - it is impossible to press the chin to the chest.
- Brudzinski's sign. When trying to pull his head to his chest, the patient involuntarily bends and pulls his legs towards his stomach.
- Kernig's sign. Alternately, the legs of the patient lying on his back are raised and bent at an angle of 90° at the knee joint. An attempt to return them to their original position fails, as muscle tone increases.
Of all the listed signs, hemorrhagic rashes are the most obvious. 2 days after their appearance, they become pigmented, forming ulcers and necrosis. In severe situations, pathological changes can lead to dry gangrene and subsequent amputation.
Meningococcal meningitis
- Rapid rise in body temperature to +40 °C.
- Severe headaches triggered by movement, touch, bright lights and loud noises.
- Repeated vomiting, independent of food intake, without relief.
- Low blood pressure, rapid pulse, shortness of breath.
The patient often assumes the fetal position - lying on his side with his hands tucked in, his legs clasped at the knees. Characteristic symptoms such as a stiff neck, Brudzinski's sign, and Kernig's sign may or may not be present. The disease is characterized by a high mortality rate; without proper treatment it reaches 50%. Survivors may show consequences of the infection: paresis, deafness, intellectual impairment, hydrocephalus.
Hypertoxic (fulminant) form of meningococcal infection
- Sudden rise in temperature to +40 C or more.
- The skin is cold, sticky with sweat. The patient has a fever and may have convulsions.
- Numerous hemorrhagic rashes appearing before the eyes. Small spots quickly merge into large hemorrhages of a purplish-cyanotic color. Skin changes resemble cadaveric spots.
- Blood pressure is low.
The hypertoxic form develops extremely quickly, within a few hours. Brain swelling occurs, accompanied by severe headaches, dizziness, vomiting, and loss of consciousness. This leads to infectious-toxic shock, a condition requiring immediate resuscitation. Without timely treatment, the patient may die.
Symptoms
Symptoms accompanying meningococcal infection vary depending on the form of the disease. The clinical picture during carriage is often absent. Manifestations of acute nasopharyngitis include:
- Pain in the head area (localized mainly in the frontoparietal zone).
- Dry cough.
- Catarrhal phenomena in the nasopharynx (stingling, swelling, pain).
- Nasal congestion (scanty purulent mucous discharge from the nasal passages is rarely possible).
Less commonly, symptoms such as hyperesthesia (skin sensitivity disorder - numbness, tingling), myalgia (muscle soreness), and dizziness occur. This form of the disease in adult patients is accompanied by deterioration of health, weakness, malaise, loss of appetite, and sleep disturbance.
Signs of meningococcal meningitis include pain in the head, increased body temperature, and repeated bouts of vomiting that do not lead to relief. Symptoms of meningococcal infection in infants and young children include increased restlessness, unreasonable, frequent crying, and seizures, which indicates the severity of the condition and requires immediate treatment. Other signs of meningococcal infection in children:
- A rash on the skin of a specific nature, distributed throughout the body (buttocks, legs, thighs).
- Increased sensitivity (intolerance) to bright light.
- Catarrhal phenomena in the area of the nasopharyngeal mucosa (swelling of the mucous membrane, nasal congestion, soreness, itching in the throat).
- Pale skin tone.
- Bulging of the fontanelle (in infants).
- Psychomotor agitation alternating with retardation and lethargy.
- Throwing the head back (in infants).
- Positive pathological symptoms and reflexes (Kernig, Brudzinsky, decreased, hyporeflexia of abdominal reflexes).
- Tachycardia (muffled heart sounds, systolic murmurs).
- Decreased blood pressure values.
If swelling of the brain tissue occurs, there are signs of damage to the cranial nerves. During a visual examination, hyperemia (redness), hyperplasia (enlargement) of lymphoid follicles located in the pharynx (posterior wall) is revealed.
Meningococcemia (sepsis) is characterized by a rapid course with the formation of secondary foci of infectious lesions in different parts of the body. A stable body temperature often reaches 39-41°C and lasts for 2-3 days. Then the indicators decrease, sometimes to normal values (in shock). During this period, body temperature indicators do not reflect the real severity of the patient’s condition.
At the same time, signs are observed: muscle soreness in the back and limbs, lack of appetite, feeling of thirst, feeling of dry mouth, pale or bluish tint of the skin. In young children (under 5 years of age), bowel disorders often occur. A striking characteristic of meningococcemia is rashes on the skin. The rash appears 5-15 hours after the onset of the disease. Sometimes rashes are detected on the 2nd day.
The rash occurs as a result of exposure to endotoxin, which is formed during the life of bacteria during meningococcal infection. Endotoxin destroys the walls of small blood vessels, which leads to the appearance of numerous foci of hemorrhage that form specific “stars” on the skin. The elements have irregular shapes and different sizes.
Hemorrhages in the area of internal organs lead to the formation of foci of necrosis. The rash with meningococcemia at the first stage of development of the disease looks like an exanthema (papular rashes with the formation of papules - nodules that rise above the general surface of the skin) or enanthema (rashes on the mucous membranes of the mouth, nose, pharynx, less often the eyes), later it takes on the appearance of purpura - typical hemorrhagic rashes.
The red coloration of the elements of the skin rash is given by red blood cells that have penetrated outward from damaged vessels (usually capillaries). The sizes of the elements can vary from 1 to several millimeters in diameter. Over time, areas of tissue necrosis (death) form in place of the purpura. Areas of necrosis are subsequently rejected with the formation of poorly healing ulcers in their place. In the area of the extremities, the depth of the ulcers can reach large sizes, up to exposure of the bones (gangrene).
Foci of necrosis are most often localized in the area of the shells of the ears, nose, and terminal phalanges of the toes and hands. In addition to damage to the skin, cases of joint damage (arthritis, polyarthritis) are common. Arthritis develops during the 2nd week of the disease. Meningococcal sepsis more often (up to 90% of cases) occurs in conjunction with meningitis. Meningococcemia in children requires emergency medical care.
Diagnosis of meningococcal infection
The choice of laboratory material for analysis depends on the form of the disease; it can be blood, nasopharyngeal mucus, cerebrospinal fluid, scrapings from a hemorrhagic rash, purulent discharge from the meninges.
For nasopharyngitis and asymptomatic carriers, nasopharyngeal secretions are collected using a special swab. The material must be taken from the back wall of the throat behind the soft palate.
For cerebrospinal meningitis, CSF (cerebrospinal fluid) is collected. It is collected by puncture in an amount of 2 - 5 ml into a sterile tube. They are immediately sown on a nutrient medium or urgently, observing the temperature regime, sent to the laboratory. At the time of collection of cerebrospinal fluid, the presence of pus can be visually determined; in this case, the cerebrospinal fluid will be cloudy. In some cases, bacteria can only be detected under a microscope.
When collecting biomaterial posthumously, pus from the membranes of the brain is most often taken for analysis. The study is necessary to clarify the diagnosis. If meningococcal disease is confirmed, the circle of contacts should be identified to prevent the spread of infection.
Blood and serum tests are optional. It allows you to assess the severity of the condition, as well as detect antibodies to meningococcus. Based on urine test data, kidney function can be determined. To make a diagnosis and assess the extent of damage to the body, instrumental diagnostic methods such as echocardiography, x-ray, ultrasound of the brain and abdominal organs, Doppler examination of blood vessels, ophthalmoscopy, and magnetic resonance imaging are used.
Types of laboratory diagnosis of meningococcal infection
Bacterioscopic examination (RA, PCR). Determines the presence of meningococci, serogroup and their concentration. Allows differentiation from other bacteria that cause inflammation of the brain and spinal cord. The crop is sown for 18 to 24 hours in a thermostat at +37 C, with a high CO2 content (up to 10%). Neisseria meningitidis is determined by detecting the production of acetic acid as a result of the fermentation of glucose and maltose.
The serological method (ELISA, RIA) is based on the detection and determination of the concentration of IgM antibodies. The titer increases significantly at the onset of meningococcal infection in generalized forms. The concentration decreases during the period of remission, IgG antibodies begin to predominate over IgM immunoglobulins. In patients who have recovered from the disease, specific bactericidal antibodies are detected in the blood serum: agglutinins and hemagglutinins.
Regardless of the type of biomaterial, it requires urgent analysis since the pathogen dies outside the human body. Laboratory diagnostics includes microscopy, biological culture, and requires not only identification of the pathogen, but also determination of antibiotic sensitivity.
Treatment
When treating meningococcal infection, regardless of the degree of manifestation of the disease and its form, the doctor considers the patient’s condition as mortally dangerous. This is especially true for children, because more than half of them go through intensive care. The patient is hospitalized for emergency diagnostics. Antibiotics can be prescribed only after laboratory tests.
Depending on the serotype, the basis of treatment may be drugs such as penicillin, ampicillin, chloramphenicol. In epidemiological conditions with limited resources, ceftriaxone is preferred. Antibiotics are the basis of treatment, however, antipyretic, anticonvulsant and decongestant drugs, infusion, detoxification and oxygen therapy medications are used together with them. In this way, complex treatment of meningococcal infection is carried out with individual selection of drugs, under the constant supervision of a doctor. Therapy for complicated generalized forms can last for a month, and rehabilitation can take several years.
Epidemiological surveillance
Surveillance, from case detection to investigation and laboratory confirmation, is critical to the control of meningococcal meningitis. Main objectives of surveillance:
- detection and confirmation of disease outbreaks;
- detection and confirmation of disease outbreaks;
- assessing the burden of disease;
- monitoring antibiotic resistance profiles;
- monitoring the circulation, spread and evolution of individual meningococcal strains (clones);
- assessing the effectiveness of strategies to control meningitis, in particular preventive vaccination programs.
Complications and consequences
During illness, the following complications may occur:
- cerebral edema;
- hydrocephalus;
- hemorrhagic cerebral stroke;
- acute renal failure;
- paralysis and other dysfunctions.
Against the background of meningococcal infection, herpes, otitis media, and meningococcal pneumonia can develop. Severe disease can cause the development of asthenic syndrome, expressed in general weakness and periodic headaches. Lead to arterial hypertension, hearing loss, epilepsy and hemiparesis (paralytic damage to one side of the body). Patients who have had meningococcal infection often experience apathy and depression.
List of sources
- Koroleva I.S., Beloshitsky G.V. Meningococcal infection and purulent bacterial meningitis. - M.: Publishing house "Medical Information Agency", 2007;
- Bogadelnikov I.V. Differential diagnosis of infectious diseases in children. - Simferopol, 2007;
- Differential diagnosis of infectious diseases / [Kazantsev A.P., Zubik T.M., Ivanov K.S., Kazantsev V.A.]. - M.: MIA, 1999;
- Izvekova I.Ya., Arbekova V.P. Meningococcal infection // Textbook. - Novosibirsk. - 2005;
- Tatochenko V.K. Immunoprophylaxis-2004. - M. - 2004;
- Sorokina M.N., Ivanova V.V., Skripchenko N.V. Bacterial meningitis in children. M.: Medicine; 2003.
Disease Prevention
Post-infectious immunity. After an illness, a strong immunity develops that protects against re-infection. However, it occurs only in the serogroup of bacteria that caused the disease. In total, there are 12 types of meningococcal groups.
- Vaccination. 3 types of vaccines have been developed:
- Polyvalent polysaccharides (invented 30 years ago).
- Mono- and polyvalent conjugate vaccines (used since 1999).
- New monovalent conjugate vaccine MenA (developed in 2010-2011).
As much as possible, the drug can cover only 4 serogroups: A, C, Y and W. Unfortunately, such a vaccine has not yet been developed to protect against all types of infection.
The meningococcal vaccine is not included in the childhood vaccination schedule. You can only get vaccinated yourself. It should be carried out before traveling to countries at risk and for epidemiological reasons, i.e. during an epidemic when the serotype is known.
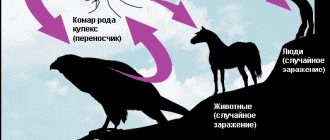
Causes and risk factors
The causative agent of meningococcal infection is the gram-negative microorganism Neisseria meningitidis, which belongs to diplococci, i.e., round, bean-shaped bacteria that form a pair. Meningococcus does not have flagella and cannot move, but has a capsule that provides it with protection from phagocytosis when it enters the body. Does not create a dispute. This type of infection is anthroponotic, which means it is transmitted only from person to person. Meningococcus is very unstable in the external environment; its lifespan outside the human body is about half an hour. It is transmitted by airborne droplets, the source of infection is a sick person or an asymptomatic carrier. There are 12 known serotypes of the pathogen, some of which (A, B, C, W, X and Y) can cause epidemic outbreaks.
Susceptibility to meningococci is quite high and the infection is widespread, however, when infected, not everyone gets sick, but only people with weakened immune systems - for this reason, children are more susceptible to the disease, due to the insufficient maturity of the immune system.
In most patients, meningococcal infection causes acute nasopharyngitis, which in its course is not much different from a common acute respiratory infection. When airborne particles containing Neisseria meningitidis are inhaled, the pathogen enters the nose and/or mouth, spreads through the nasopharynx and causes inflammation, which, although acute, usually resolves within a few days. However, in some people, the infection penetrates other organs and systems, affecting them, and in severe cases takes on a severe generalized form. Meningococci are able to overcome the blood-brain barrier, entering the brain and affecting the meninges (meningitis), and sometimes the brain tissue itself (meningoencephalitis).
The main risk factor, therefore, is a decrease in the body's defenses. The complicated epidemic situation and overcrowding, especially in children's institutions, are also important.
There is some seasonality of incidence - the risk of getting sick increases in the spring months, although it is not zero throughout the year.
After an illness, a fairly stable immunity is formed, but it is group-specific, which means resistance to only one serotype of the pathogen. Repeated cases of the disease are extremely rare, however, they cannot be excluded when infected with meningococcus of a different serotype.
Advantages of JSC "SZDCM"
Laboratory tests are extremely important in the treatment, especially of such serious diseases. It is important to get not only the fastest, but also the most accurate and detailed result.
At your service:
- Laboratory with technological equipment.
- Qualified and friendly staff.
- Fast analysis and several options for obtaining results.
Medical centers and terminals are located in places with convenient transport links in St. Petersburg, Leningrad region, Veliky Novgorod, Staraya Russa, Okulovka and Pskov.