Haemophilus influenzae (hemophilus influenza, hemophilus influenzae) is the causative agent of an acute inflammatory process in the human body, in which purulent foci - abscesses - form in the tissues of the nervous and respiratory systems. The clinical picture of the pathology is in many ways similar to the signs of a common cold, and the microbe has a large number of varieties. These features make it difficult to diagnose the infection and make it dangerous in epidemic terms. Medicine knows only the most severe cases of the disease.
Haemophilus influenzae lives in the upper respiratory tract of healthy people. Under normal conditions, it does not cause harm to health. When the immune system is weakened, these harmless microorganisms are activated and become the cause of a number of troubles.
Haemophilus influenzae has several equivalent names: Pfeiffer bacillus, Afanasyev-Pfeiffer bacillus. Haemophilus influenzae, influenza bacillus. Koch was the first to discover hemophilic bacteria. The microbe received its name thanks to the discovery of two scientists - Afanasyev and Pfeiffer. They independently isolated Haemophilus influenzae from the lung tissue of a person who died during the influenza pandemic. Currently, medical scientists continue to study the properties and characteristics of the bacterium, since it is a common cause of purulent meningitis in young children.
The pathology mainly affects children from 6 months to 5 years. Their body temperature rises, a runny nose, pain and sore throat, cough, and severe headache appear. The disease usually develops in autumn-winter and early spring, when the body's immune system is weakened and cannot fully perform its protective functions. Diagnosis consists of a physical examination and laboratory tests. Treatment of hemophilus influenzae infection is conservative, etiotropic, antimicrobial.
Diseases caused by Haemophilus influenzae usually have a favorable prognosis and do not threaten the lives of patients. With timely and correct treatment, neurological complications develop in only 30% of cases. The mortality rate is also low - 5%. Thanks to active immunization of the population, the incidence is 25 cases per 100,000 people. Currently, the treatment of infection is becoming a general medical problem, which is associated with the increasing resistance of Haemophilus influenzae to most antibiotics.
Etiology
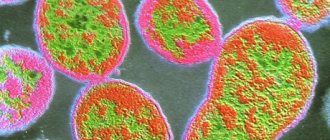
Haemophilus influenzae is a small polymorphic coccobacilli that can exist in 2 forms: acapsular and capsular. In the first case, the cell consists of a jelly-like cytoplasm surrounded by a soft lipid membrane. Such microbes are not pathogenic and are part of the normal microflora of the nasopharynx of healthy people. The capsule covering the bacterium on top of a soft lipid membrane consists of carbohydrates and proteins, is durable and protects the microbe from the effects of immunocompetent cells.
The capsule is one of the pathogenicity factors of Haemophilus influenzae, ensuring its penetration into the epithelial cells of the mucous membrane, lymph and blood. It suppresses the phagocytic activity of leukocytes. Pili ensure fixation of the pathogen on the cells of the ciliated epithelium. Additional pathogenicity factors include IgA proteases that break down secretory immunoglobulins. Enzymes produced by the microorganism destroy the protective antibodies of the mucous membrane, which also promotes adhesion, invasion and the development of the infectious process. When the bacterial capsule is destroyed, a powerful toxin is released into the blood - the cause of shock and death in patients.
These asporogenous rod-shaped bacteria are nonmotile. They are Gram-stained red and are located singly, in pairs or in clusters in the smear.
Microbiologists currently identify more than fifteen varieties of Haemophilus influenzae. They are divided into seven biotypes based on cultural properties and six capsule types based on antigenic properties.
Haemophilus influenzae is a facultative anaerobe. It grows on nutrient media containing fresh blood. For the growth and reproduction of the bacillus, factors contained in red blood cells are required: heat-labile Y and heat-stable X. The bacterium has K and O antigens.
The influenza bacillus is unstable in the external environment, sensitive to most antibiotics of the main groups and to the most common disinfectants. It dies when boiled, exposed to sunlight, radiation and when dried.
Where does Haemophilus influenzae come from?
At the end of the 19th century, the Pfeiffer bacillus was first isolated from patients during the active development of influenza.
This was the basis for believing that the microorganism is the cause of the development of viral infections. Almost 30 years later, it was established that the diseases are non-viral and that Haemophilus influenzae requires the presence of one of the blood factors at the time of reproduction. The microorganism is not a type of exotic bacteria that can only be imported from certain countries. Haemophilus influenzae is a natural inhabitant of the body of every person; it is a representative of the normal microflora of the oropharynx.
They are classified as opportunistic. The favorite habitat of Haemophilus influenzae is the mucous membranes of the upper respiratory tract. They attach to epithelial cells using special formations - flagella. These same structures promote stronger adhesion to the cells of the mucous membranes, penetrating between which microbes lead to the development of diseases.
Haemophilus influenzae is transmitted by airborne droplets from an infected person to a healthy person. But not in all cases this contributes to the occurrence of illnesses; this requires certain conditions.
Epidemiology
Haemophilus influenzae infection - anthroponosis. It lives only in the human body, mainly on the mucous membrane of the respiratory tract. In 90% of cases, microbes are isolated from the nasopharynx of healthy people. Normally, in children and adults, the amount of Haemophilus influenzae should not exceed 104 colony-forming units. These bacteria, along with staphylococci, are part of the normal human microflora.
A healthy carriage usually lasts several months and often persists even with high doses of antibiotics. Symptoms of the pathology are completely absent. The bacteria carrier feels absolutely healthy, but at the same time is dangerous in terms of epidemics.
The spread of infection is carried out by an aerosol mechanism, which is carried out by airborne droplets. The pathogen enters the external environment during severe coughing, sneezing, talking along with secretions from the respiratory tract. The risk of infection is greatest for persons located within a radius of three meters or less from a sick person. Children become infected from adult carriers in the first years of life. Transmission of the pathogen through household contact is extremely rare due to its low stability in the environment. Infection is possible through towels, toys, dishes and other household items contaminated with bacteria.
The risk group for hemophilus influenzae infection is:
- Patients with agammaglobulinemia,
- Persons who have undergone splenectomy
- Patients taking cytotoxic drugs
- Children of the first years of life,
- Formula-fed babies
- premature babies,
- Preschool workers
- Aged people,
- Cancer patients,
- Children living in orphanages
- Persons with congenital or acquired immunodeficiency,
- Children attending nurseries and kindergartens,
- Representatives of non-European races.
It is dangerous for this contingent to come into contact with patients with hemophilus influenzae infection. Children between 6 and 12 months are most vulnerable. At this time, the immune system ceases to be supported by the mother's antibodies and begins to function independently. Hemophilus influenzae infection in infants, due to their imperfect immunity, often ends in generalization of the process, followed by coma and death.
diseases that can be caused by H. Influenzae
The bacterium H. Influenzae is the cause of various infectious forms. It affects the membranes of the brain, lung tissue, nasopharynx, blood, subcutaneous fat, and bones. In children, hemophilus influenzae infection usually occurs in the form of meningitis, epiglottitis, and cellulitis. Pneumonia is more common in adults and older people. In addition, the following diseases of hemophilic etiology are distinguished: purulent arthritis, septicemia, otitis media, osteomyelitis, sinusitis, pericarditis, pleurisy, sepsis. Haemophilus influenzae often causes nosocomial infections in people undergoing hospital treatment.
After an infection, a strong immunity is formed, which prevents repeated cases of infection in adulthood.
Classification
Haemophilus influenzae exists in several forms, which will differ in the nature of their course and symptoms.
Thus, such a microorganism causes:
Separately, it is worth highlighting such a form as carriage. In such cases, despite the presence of Haemophilus influenzae, symptoms are completely absent, and the person feels completely healthy. However, even with this, the infected person is dangerous to others - this lies in the fact that he constantly releases the pathogen into the environment.
Pathogenesis
The entrance gate of infection is the mucous membrane of the nasopharynx. The pathology is characterized by long-term persistence of the pathogen in the area of the infection gate. This is the latent stage of the disease. When the general resistance of the body decreases, it becomes manifest. An increase in the total microbial mass and the addition of a viral infection are conditions that accelerate this process. Epiglottitis, otitis, and sinusitis are associated with this localization of the pathogen.
The infection spreads lymphogenously or hematogenously through the surrounding tissues, causing the development of bacteremia, septicemia and inflammatory processes in the bronchi, lungs, and adipose tissue. In severe cases, hematogenous dissemination of microbes occurs with damage to joints, bones and internal organs.
Haemophilus influenzae penetrates the blood and persists asymptomatically until the number of microbial cells reaches its maximum. The bacillus then penetrates the blood-brain barrier into the central nervous system and causes the development of purulent meningitis.
Factors contributing to the development of hemophilus influenzae infection:
- Smoking,
- Alcoholism and drug addiction,
- Long-term antibiotic therapy
- Nervous tension and emotional outbursts,
- Hypo- or hyperthermia,
- Poor living conditions,
- Unfavorable environmental situation.
Forms of the disease
Based on their clinical manifestations, the following types of hemophilus influenzae infection are distinguished:
- acute pneumonia;
- purulent arthritis;
- purulent meningitis;
- inflammation of the epiglottis (epiglottitis);
- septicemia;
- cellulite (inflammation of the subcutaneous tissue);
- other diseases (otitis, sinusitis, pericarditis, pleurisy).
Haemophilus influenzae infection is one of the leading causes of pneumonia and meningitis in children
Symptoms
The duration of the incubation period is not precisely determined. It is believed that it is 2-4 days. All this time the patient is dangerous to others. At the initial stage, the symptoms of hemophilus influenzae infection are similar to colds. The disease in most cases proceeds like a common ARVI. But it happens that the infection becomes the cause of more serious diseases with specific manifestations.
Clinical signs of pathology are determined by the localization of the pathological process. Intoxication and catarrhal syndromes are characteristic of any clinical form of infection. In patients, the temperature rises to 40 degrees, chills, cephalalgia, rhinitis, discomfort in the throat, wet cough, fatigue, lethargy, rumbling and pain in the abdomen, stool disorders, flatulence, pain in muscles and joints occur.
- If the primary source of infection is located in the ear, otitis media develops. Patients complain of throbbing and shooting pain in the ear, hearing loss, and the appearance of mucopurulent discharge.
- With sinusitis, there is discomfort in the nose, bursting pain in the projection of the affected sinus, purulent nasal discharge, impaired nasal breathing, and decreased sense of smell.
- Inflammation of the tissue is manifested by swelling of the face, mainly the cheeks, hyperemia or cyanosis of the skin, pain and fever.
- Epiglottitis is the most severe form of hemophilus influenzae infection, characterized by severe chills, cyanosis, shortness of breath, tachycardia, hypersalivation, stridor, and retraction of the pliable areas of the chest. Patients are in a forced position. The pain makes it difficult to swallow even liquid food. Rapidly progressing croup can lead to the death of the patient from asphyxia.
- Conjunctivitis in newborns is manifested by redness of the eyes, swelling of the eyelids, profuse lacrimation, and the appearance of purulent secretion in the corners of the eyes.
- Arthritis affects the large joints of the upper and lower extremities. The disease is accompanied by redness of the skin, swelling and local hyperthermia.
- Patients with pneumonia complain of chest pain, cough with purulent sputum, and fever.
- Meningitis is manifested by profuse vomiting without previous nausea, fever, chills, loss of consciousness, convulsions, meningeal signs, focal neurological symptoms, lethargy, adynamia, and rapid exhaustion of patients. Less commonly, stupor develops, and in some cases coma.
- Osteomyelitis causes severe pain in the limb, swelling of the tissue over the affected bone and redness of the skin.
- With septicemia - splenomegaly, hypotension, tachycardia, hemorrhages on the skin, lack of appetite, stool disturbances. Patients sleep a lot and restlessly. The disease has a rapid and even lightning-fast course. It often ends in infectious shock and death of the patient.
Haemophilus influenzae can cause simultaneous damage to several organs: meningitis in patients is often combined with arthritis, cellulitis, and epiglottitis.
Hemophilus influenzae infection is a serious medical problem due to the variety of clinical forms, frequent generalization of the process, the development of severe complications and a high risk of death.
Symptoms of hemophilus influenzae infection
Since H. influenzae is an opportunistic bacterium, doctors have no way to reliably determine the incubation period of the infection it causes. If there are predisposing factors, for example, acute respiratory infections, it is believed that the climax occurs 2–5 days from the moment of penetration of Haemophilus influenzae into the submucosal layer of the membrane.
Common symptoms of acute Hib infection:
- body temperature up to 40° C;
- fever;
- weakness;
- malaise;
- headache.
The chronic or latent form of hemophilus influenzae infection becomes protracted with vague symptoms. Signs of exacerbation include a sore throat, low-grade fever, coughing, and inflammation of the nasal mucosa.
Systemic diseases septicemia and sepsis, which arise due to the penetration of the Afanasyev-Pfeiffer bacillus into the blood, develop at lightning speed, are accompanied by septic shock, and end in death. Children from 6 to 12 months are more often susceptible to pathology.
The primary symptoms of meningitis resemble those of ARVI: fever, runny or stuffy nose, sore throat when swallowing, watery eyes, cough. Later, a person notices lethargy or excitability, migraines, convulsions, muscle paralysis, delirium, a rash on the body, frequent vomiting, confusion of thoughts begin.
The patient's posture changes - the head is thrown back, and the knees are tucked towards the stomach.
Meningitis can be accompanied by blood poisoning and inflammation of other organs. The consequences of the pathology are irreversible hearing impairment, intractable central nervous system diseases, and death. Meningitis most often affects children under 9 months.
With pneumonia, a person feels pain in the chest; it is characterized by general intoxication, dry cough, and high fever. Pathology most often begins with lack of appetite, weakness, and sleep disturbances. An x-ray shows either a focal or lobar form of Haemophilus influenzae pneumonia, and in 70% of cases it is accompanied by pleurisy. The infection most often develops in adults and can be complicated by otitis media and pericarditis.
Epiglottitis, in addition to general symptoms, is accompanied by pain when swallowing, loss of voice, difficulty breathing and profuse salivation. Children over 2 years of age are susceptible to the disease. In 90% of cases, inflammation is accompanied by blood poisoning - bacteremia. The infection develops acutely, with high fever, severe intoxication, swelling of the epiglottis covering the entrance to the trachea, and the membranes in the larynx, which often leads to asphyxia and respiratory arrest.
With septic arthritis, swelling of the tissue in the joint area appears, pain when moving, and the skin over it becomes hot and red. A complication of hemophilus influenzae infection can be osteomyelitis, purulent damage to bone and cartilage tissue.
Panniculitis or cellulitis often begins as nasopharyngitis, accompanied by mild intoxication, an increase in local temperature and swelling of the body area, a change in the color of the epidermis - it acquires a cyanotic (bluish) tint. Subcutaneous tissue often becomes inflamed in infants of the first year of life. The pathological focus is localized on the face or limbs.
With Haemophilus influenzae infection, otitis media often develops. Signs of inflammation: weakness, fever, migraine, noise and pain in the ear, flow of orange-red fluid if the eardrum ruptures.
Diagnostics
Infectious disease doctors and pediatricians are involved in the diagnosis and treatment of hemophilus influenzae infection. They examine patients, listen to complaints and study the results of laboratory and instrumental examinations. After collecting anamnesis and assessing the condition of the skin, doctors measure blood pressure, temperature and pulse. Often additional consultation with an ENT doctor, gynecologist, surgeon, neurologist, ophthalmologist, or pulmonologist is required.
Laboratory research:
- General analysis of blood and urine - to determine signs of inflammation,
- PCR – to detect pathogen DNA,
- Culture of sputum, cerebrospinal fluid or throat discharge - to isolate the pathogen,
- Serological tests - to determine antibodies in the blood,
- Immunodiagnostics – detection of the capsular antigen of Haemophilus influenzae using ELISA.
Instrumental measures are carried out to confirm the expected diagnosis and identify existing complications. The most common and informative are: ultrasound, radiography, CT and MRI.
Microbiological examination of clinical material is the main diagnostic method that allows one to isolate the rod from a patient. Upper respiratory tract discharge, pus from the ear, sputum, cerebrospinal fluid, joint fluid, and blood are delivered to the bacteriological laboratory for analysis. The biomaterial is studied under a microscope and inoculated on nutrient media. For inoculation, chocolate agar with growth factors is used. After isolating a pure culture and identifying the pathogen, a test for antibiotic resistance is performed.
Diagnosis of hemophilus influenzae infection
The main role in differentiating pathology is played by laboratory testing of biomaterial to detect and identify the pathogen. There is no special preparation for the procedures. For the analysis, you need blood from a vein, purulent discharge, a swab from the nasal mucosa, and sputum. For hemophilic meningitis, cerebrospinal fluid will be required for examination, and for arthritis, joint fluid will be required.
Methods for identifying Haemophilus influenzae:
- bacterioscopic;
- bacteriological;
- test for the presence of B-capsule antigen;
- immunofluorescence reaction;
- counter immunoelectrophoresis;
- linked immunosorbent assay;
- PCR.
When differentiating, attention is paid to the lack of ability to destroy red blood cells and the presence of influenza bacilli DNA particles in the blood. Laboratory technicians also perform an antibiogram.
Treatment
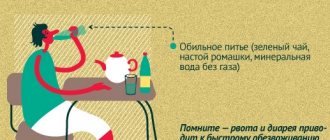
Patients with severe and moderate forms of infection are hospitalized in the hospital for the entire febrile period. Experts recommend staying in bed, avoiding salty foods, and drinking at least 2 liters of water per day.
Drug treatment of hemophilus influenzae infection:
- Etiotropic therapy – broad-spectrum antibiotics from the group of cephalosporins “Ceftriaxone”, “Ceftazidime”, macrolides “Erythromycin”, “Azithromycin”, penicillins “Amoxiclav”, “Augmentin”, fluoroquinolones “Ciprofloxacin”, “Ofloxacin”.
- Detoxification and dehydration therapy - diuretics "Furosemide", "Hypothiazide", anti-inflammatory drugs "Dexamethasone", "Prednisolone", saline solutions.
- Symptomatic therapy – antipyretics “Nurofen”, “Paracetamol”; expectorants "Ambroxol", "ACC"; immunomodulators “Likopid”, “Imunorix”; desensitizing agents “Zodak”, “Zirtec”; vitamin and mineral complexes.
The course of treatment averages ten days, but may vary depending on the form of the disease and the resistance of the pathogen.
The prognosis for hemophilus influenzae infection is ambiguous. Timely identification of the pathogen and adequate therapy allow for a quick and complete recovery. With the development of severe complications, the prognosis becomes serious, often unfavorable.
Complications of diseases caused by haemophilus influenzae:
- Persistent hearing loss
- Hydrocephalic-hypertensive syndrome,
- Septic shock
- Blindness,
- Suffocation,
- cerebral edema,
- Mental disorders,
- Empyema,
- Defects of a newborn,
- Spontaneous miscarriage in pregnant women,
- Death.
Treatment of hemophilus influenzae infection
Until the pathogen's resistance to antimicrobial drugs is confirmed, the patient is prescribed empirical therapy, that is, based on previous experience. After receiving the information, the drugs and dosage are adjusted.
When treating hemophilus influenzae infection, the following drug groups are used:
- antibiotics (2nd–3rd generation cephalosporins, macrolides);
- combination of a beta-lactam antibiotic with inhibitors (Biseptol, penicillins + Clavulanic acid);
- antiseptics;
- glucocorticosteroids;
- expectorants;
- antipyretics;
- painkillers.
Haemophilus influenzae remains resistant to Lincomycin, Oxacillin and Oleandomycin, so they are not used. Antibiotics Chloramphenicol and Tetracycline are also prescribed with caution due to their relative unsafety for the body.
Prevention
Currently, specific prevention of hemophilus influenzae infection has been developed and introduced into the practice of clinicians. Timely vaccination is the optimal means of protection against infections caused by this pathogen. The vaccine consists of fragments of a bacterial capsule and does not contain a live pathogen. Due to this, it is administered to children and people with reduced immunity.
There are several foreign and domestic vaccines:
- "Akt-Hib"
- "Hiberix"
- "Pentaxim"
- "Infanrix Hexa"
- “Haemophilus influenzae type b conjugate dry vaccine.”
The vaccines listed above have been licensed. A specific drug name is used against each type of Haemophilus influenzae. The vaccine is given to children under 5 years of age, as well as to persons at risk.
Nonspecific prevention consists of strengthening the immune system. Emergency prevention is carried out after contact with a sick person. To do this, doctors recommend taking a course of antibiotics.
Prevention and prognosis
Specific preventive measures include vaccination against Haemophilus influenzae. It is best to carry out this procedure for children aged from 3 months to 2 years. Today the most effective vaccines are:
- "Akt-Hib";
- "Hiberix";
- "Pentaxim";
- "Infanrix Hexa";
- “Haemophilus influenzae type b conjugate dry vaccine.”
Vaccination can also be prescribed by the attending physician according to individual indications for each patient. Additional preventive measures include strengthening the immune system.
The prognosis of the pathological influence of Haemophilus influenzae will be dictated by the form of the infectious process. In persons from the main risk group, mortality is observed in 20% of cases, and complications develop in 35%.
Haemophilus influenzae (hemophilus influenza, hemophilus influenzae) is the causative agent of an acute inflammatory process in the human body, in which purulent foci - abscesses - form in the tissues of the nervous and respiratory systems. The clinical picture of the pathology is in many ways similar to the signs of a common cold, and the microbe has a large number of varieties. These features make it difficult to diagnose the infection and make it dangerous in epidemic terms. Medicine knows only the most severe cases of the disease.
Haemophilus influenzae lives in the upper respiratory tract of healthy people. Under normal conditions, it does not cause harm to health. When the immune system is weakened, these harmless microorganisms are activated and become the cause of a number of troubles.