Possible adverse reactions
Amiodarone can cause a lot of adverse reactions such as:
- sinus bradycardia and vasculitis or thrombophlebitis, progression of myocardial failure, etc.;
- nausea-oral reactions, stool disorders, epigastric heaviness;
- hyper- or hypothyroidism;
- Dyspnea and cough, alveolitis or interstitial pneumonia, apnea and bronchospasm, pulmonary fibrosis;
- cephalgia or depression, dizziness and hallucinations, tremor and neuropathy;
- uveitis or retinal microdetachment;
- decreased potency, alopecia, myopathy or hyperhidrosis, rashes and photosensitivity.
The drug may interact with other medications, causing undesirable reactions, so you must first check the compatibility of Amiodarone.
Contraindications
WE RECOMMEND THE ARTICLE!
Nitrosorbide is used for maintenance and recovery therapy after angina and heart attack. Read more >>
The drug also has its own contraindications, which include conditions like:
- thyrotoxicosis and hypothyroidism;
- cardiogenic shock or hypokalemia;
- bradycardia or collapse;
- arterial hypotension or weak sinus syndrome;
- AV blockade or sinoatrial blockade of 2 and 3 degrees in the absence of a pacemaker;
- Interstitial pulmonary pathologies;
- The period of breastfeeding or pregnancy;
- Taking drugs from the category of MAO inhibitors;
- Childhood;
- Hypersensitivity to iodine or individual components of the drug.
Description of the medication
Amiodarone is an antiarrhythmic drug that facilitates cardiac activity, but does not affect the release of blood flow and contractile functions of the myocardium. Both solution and tablets of Amiodarone are available for sale. The solution is placed in ampoules, tablets are sold in blisters.
- The mechanism of action of Amiodarone is reduced to antiarrhythmic effects. The medication facilitates cardiac activity.
- By relaxing the heart arteries, blood circulation increases and the heart rate decreases, while blood pressure levels normalize.
- Amiodarone has antianginal, coronary vasodilating and antiarrhythmic effects.
- When taking the medication, the oxygen needs of the myocardium are significantly reduced, its energy reserves increase, and the heart begins to function better.
The therapeutic effect begins to be felt within half an hour after taking the drug, and the active ingredient reaches its maximum concentration after about 5-7 hours.
From practice
The instructions for use indicate that amiodarone, except in the most emergency cases, should be administered through a central vein (catheter in the subclavian vein), but this is usually neglected. When administered through peripheral veins (veins in the arm), we get local inflammation; it is extremely difficult to get into this vein again. As patients put it, the veins are “burned” by the drug. More precisely, the veins narrow at the puncture site due to the alcohols in which amiodarone is diluted. In reality, the subclavian catheter is placed by resuscitators, firstly, they are physically unable to install it for everyone, secondly, in inexperienced hands, the subclavian catheter poses a greater danger than a damaged peripheral vein, thirdly, the medical staff of the departments is too overloaded to care for such a catheter, and it requires constant processing and monitoring.
Central and peripheral venous access
After the first administration of the drug, especially relatively young patients in cardiac departments (up to 55 years old), the following picture was noticed more than once: in the afternoon, a patient admitted with a newly diagnosed arrhythmia was administered the medicine. At night, the patient’s blood pressure drops sharply, sweat flows like a hail, he is pale, and breathing heavily. We connect an ECG, the rhythm is rare, but correct. While we are administering drugs that raise blood pressure and starting to drip saline, we call resuscitators. But by the time they arrive, suddenly everything is restored, and now the patient is pink and happy, and most importantly, without arrhythmia. Therefore, you need to know that sometimes amiodarone “reboots” the heart so that it can continue to work correctly. The most dangerous thing is if the patient at this moment is far from the hospital and qualified medical care, because sometimes everything did not end so beautifully.
Interaction with other drugs
Use together with most other antiarrhythmics and/or rhythm-shortening drugs, with drugs that cause a decrease in potassium in the blood, including some diuretics, is contraindicated. It affects the metabolism of methadone and may compete with some drugs for the treatment of HIV infection. Be sure to tell your doctor all the medications you are taking and do not stop or continue taking any medications along with amiodarone. While in the hospital, do not take “your” pills without consulting your doctor. This can be deadly.
Overdose
If toxicity occurs in the form of a proarrhythmogenic effect, the drug is discontinued.
Symptoms:
decreased blood pressure, sinus bradycardia, arrhythmias, atrioventricular block, cardiac arrest, attacks of ventricular tachycardia, paroxysmal tachycardia of the “feast” type, liver dysfunction.
Treatment:
gastric lavage and taking activated charcoal, if the drug has been taken recently. In other cases, symptomatic therapy is carried out. There is no specific antidote, hemodialysis is not effective, amiodarone and its metabolites are not removed by dialysis. With the development of bradycardia, it is possible to prescribe atropine, beta1-adrenergic stimulants, and in severe cases, cardiac stimulation. For tachycardia of the “pirouette” type - intravenous administration of Mg2+ salts, cardiac stimulation.
Indications and contraindications
Indications for taking Amiodarone are limited to treatment and prophylactic use for heart pathologies that occur with characteristic heart rhythm disturbances. Amiodarone tablets help with:
- ventricular arrhythmia, which is life-threatening;
- tachycardia, in which rapid heart rate is observed;
- ventricular or atrial asystole, when, under the influence of atrial impulses, premature excitation of the heart muscle occurs;
- angina pectoris, manifested by periodic acute chest pain;
- arrhythmia caused by chronic coronary or heart failure;
- atrial fibrillation associated with heart rhythm disturbances.
Amiodarone helps ease cardiac activity, and is even recommended to be taken prophylactically to prevent sudden death from arrhythmia in patients at risk.
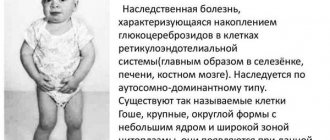
The medication is structurally similar to thyroid hormones.
After administration, the medicine is slowly absorbed, gradually leaking into the systemic circulation. It reaches its highest concentration in the bloodstream after 2-10 hours.
The drug is characterized by increased fat solubility; it accumulates in large quantities in fatty structures and intraorganic structures that have a rich blood supply, for example, in fatty structures, renal and hepatic structures, myocardium, etc.