Cause of eclampsia
This condition occurs against the background of preeclampsia, as a complicated course of pregnancy with dysfunction of vital organs. And it manifests itself as increased blood pressure, impaired renal function, and the occurrence of edema.
It is unknown why and how preeclampsia develops, but it is assumed that it occurs when the mother's body cannot meet the needs for the development of the fetus and protective mechanisms are impaired. As a result, there is a sharp deterioration in the blood supply to the uterus, placenta and fetus. And eclampsia is a severe form or the final stage of preeclampsia, in which internal organs are unable to perform their functions and the pregnant woman’s body completely loses the ability to support the vital functions of the fetus.
The transition to the last stage of preeclampsia can be triggered by the following conditions:
- Disease of vital organs during pregnancy. When carrying a child, the mother’s body is already under stress; the development of diseases, for example, of the kidneys, heart, liver, or the progression of diseases of these organs can provoke an attack of eclampsia.
- If infected during pregnancy against the background of weak immunity or lack of treatment, the woman’s body may not cope and this can also become a factor in the development of eclampsia.
- Stress. With chronic and negative psycho-emotional effects or physical stress (for example, during childbirth), prolonged vasoconstriction is observed, which leads to deterioration of blood circulation in organs. Preeclampsia also causes insufficient blood supply, so stress can trigger eclampsia.
- Research has found that there are women prone to this condition.
Eclampsia in pregnant women: risk factors
There are certain risk factors for the development of eclampsia in pregnant women, including:
- Early as well as late (after 40 years) first pregnancy;
- Family history of eclampsia;
- Obesity;
- Multiple pregnancy;
- Chronic diseases (diabetes, hypertension, kidney and cardiovascular diseases, antiphospholipid syndrome);
- The time interval between births is 10 years or more.
There are also a number of factors that provoke the development of eclampsia in pregnant women:
- Poor nutrition;
- Weakened uterine circulation;
- Violation of the water-salt balance in the body of a pregnant woman.
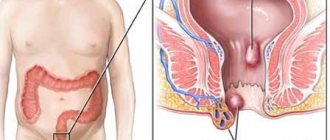
What happens during eclampsia in a woman’s body?
The development mechanism begins with preeclampsia. First, small vessels in the body narrow, causing tissues and organs to receive insufficient oxygen and nutrients. During a spasm, the load on the heart increases, since the volume of blood remains the same, and pushing blood through the vessels has become difficult. The inner lining of the arteries and veins is injured, which uses up the reserves of coagulating substances and the regulation of their tone is disrupted. Against the background of oxygen starvation of organ cells, where they also receive little blood that carries oxygen, a disorder of the liver and kidney functions occurs. This is manifested by a violation of all types of metabolism, the body’s ability to cleanse toxins, a decrease in blood filtration by the kidneys, leading to fluid retention, a decrease in the amount of urine excreted and the appearance of edema.
Further, due to insufficient blood supply in the uterus and placenta, there is a disruption in their functioning, as a result, the child suffers from oxygen starvation (hypoxia). With such a long-term condition, this can lead to damage to brain cells (the brain is most sensitive to a lack of oxygen), and in the worst case, the death of the baby. And if a woman’s protective mechanisms are not able to cope with all this or adequate medical care is not provided, then an attack of eclampsia may develop.
What does an eclampsia attack look like?
The main symptom is convulsions and loss of consciousness. But first, eclampsia is preceded by signs of circulatory problems in the brain. These are dizziness, severe headache, “floaters” or fog appear before the eyes, tinnitus, general weakness, lethargy of the woman, drowsiness or agitation, vomiting and high blood pressure (the lower level is more than 120 mm Hg, which indicates severe stress on the heart).
In clinical practice, an attack is divided into 4 periods, which occur sequentially:
- Preconvulsive. Small twitching of the eyelids is observed, which quickly spreads to the muscles of the face and arms. The gaze becomes frozen, motionless and fixed in one direction, only sometimes deviating upward or to the side. This period lasts about 20-30 seconds. The patient is breathing.
- Tonic convulsions. After twitching her hands, the woman’s head is thrown back or to the side, her body stretches, tenses, and her back begins to arch. The face becomes pale, the jaw clenches tightly, the pupils dilate, and the eyes roll under the upper eyelids, after which only white eyeballs are visible. This all also lasts about 20-30 seconds.
- Clonic seizures. Twitching is observed continuously, violently and moves from top to bottom throughout the body. Breathing is difficult or absent, the pulse is not detected, the face becomes blue, and tense veins in the neck are visible. Then the cramps gradually weaken and later disappear. The period lasts up to 1 minute, but maybe more.
- End of the attack. After this, the woman inhales loudly and deeply and breathing resumes. The patient begins to breathe slowly and deeply, foamy saliva comes out of her mouth, and if she bites her tongue, it is mixed with blood. The face gradually becomes pinkish, the pupils narrow, the pulse is rapid and weak at first, but later returns to normal.
After the attack, the woman is in a lost state, but quickly recovers from it. However, she does not remember what happened and complains of headache, lethargy and weakness. After eclampsia, the central nervous system is depressed, but then the brain becomes overly excited. Therefore, any irritants in the form of loud conversation, bright light, noise, pain can lead to a new attack.
There is a form of eclampsia in which convulsions do not occur and the woman immediately begins to faint. Characterized by high blood pressure, edema, decreased heart rate, increased body temperature, kidney damage, and impaired brain function, which develop against the background of depression of consciousness. This is the most dangerous, insidious and severe form of eclampsia, because it often ends in death.
Treatment
Eclampsia: its treatment should be carried out taking into account the severity of the clinical picture and the occurrence of consequences for the mother and fetus. There are many treatment methods that were used until recently, but due to their ineffectiveness and inexpediency, their use is excluded and has only historical significance. Until recently, eclampsia was treated using the Stroganov method, which is considered one of the leading methods. Its essence was the use of light inhalation anesthesia, the use of narcotic drugs, accelerated delivery and bloodletting. But this method is not used in our time, since narcotic drugs depress the nervous system and they have been replaced with a solution of magnesium sulfate and oxygen inhalation have replaced inhalation anesthesia.
So, treatment of eclampsia in pregnant women includes the following main points:
- compliance with a strict protective regime, while it is necessary to ensure silence, eliminate painful stimuli and remove bright light in the room.
- The woman is placed in a dark room that can be ventilated, excluding bright light and noise from the staff.
- Apply a solution of magnesium sulfate 20 milliliters every 6 hours during the day with a gradual reduction in the dose of the drug
- Sometimes aminazine is used in 1 - 2 ml of 2.5% solution with 50 ml of 40% glucose solution, which has a sedative, anticonvulsant effect and reduces blood pressure
- Neuroleptanalgesia is widely used - this is a combination of droperidol 1 - 2 ml along with diazepam 2 ml.
- To reduce blood pressure, not only magnesia and aminazine are used, but aminophylline in a dose of 5-10 ml of a 2.4% solution with 10 ml of 20% glucose has a hypotensive effect.
- In order to enhance hourly diuresis, diuretics and dehydration drugs are used to correct hypoproteinemia and hypovolemia, protein drugs are used
Treatment of eclampsia after childbirth is based on the same principles as during pregnancy, only here the threat is only for the mother, since the child has already been born. If eclampsia occurs during childbirth, we assess the readiness of the birth canal and deliver the woman by cesarean section or using obstetric forceps (extraction of the fetus during breech presentation).
Eclampsia after childbirth, its treatment begins in the first 48 hours after birth, which reduces the risk of developing recurrent seizures. Postpartum eclampsia is caused by hemodynamic disturbances, metabolic disorders and hypoxia of the body during pregnancy. The clinical manifestations of eclampsia after childbirth are identical to the clinical manifestations of eclampsia during pregnancy and childbirth. Sometimes postpartum eclampsia depends on painful shock or external irritating factors - bright light, loud sound.
Eclampsia in pregnant women. Its treatment is carried out in an intensive care ward with closed dark windows and dim lights, eliminating noise and loud sounds, which reduces the likelihood of recurrent seizures. Pregnancy with eclampsia does not last, so timely delivery and resuscitation measures can save the woman and her child. In preparation for surgical delivery, it is necessary to monitor the condition of the fetus, treat and prevent subsequent attacks of seizures, antihypertensive therapy and monitor the condition of vital organs and systems.
The diet for eclampsia is starvation, parenteral nutrition is carried out, and if the woman’s consciousness is preserved, then drinking it in the form of juice or warm tea is indicated. When expanding the regime, the amount of salt is limited to 5 g/day, the amount of liquid consumed is no more than a liter, protein foods to replenish it and fasting days are carried out 2 times a week.
Treatment of eclampsia after delivery is also carried out in the intensive care unit jointly by an obstetrician-gynecologist and an anesthesiologist. Most often, eclampsia occurs in the first 48 hours after birth, and after this time the likelihood of seizures is very low. For this purpose, maintenance therapy with magnesium sulfate solution is used. Very rarely, late postpartum eclampsia occurs - a series of seizures after 48 hours from the moment of birth and up to 28 days of the postpartum period.
Diagnosis of eclampsia
Detection of eclampsia in most cases does not cause difficulties. The clinical picture is a typical onset of an attack, before which a number of the above-mentioned symptoms are observed (vomiting, dizziness, headache, etc.). Next, convulsions develop, which begin in the face and end with continuous contraction of all muscles, and later with loss of consciousness. If eclampsia occurs in the maternity hospital, they quickly provide first aid and do a blood test, which will show signs of organ dysfunction due to deterioration in their blood supply, and a urine test, which will diagnose signs of kidney damage.
When a woman was observed in the hospital for preeclampsia or was treated for this condition previously, then if such an attack occurs during pregnancy or childbirth, doubts that it is eclampsia do not arise.
Etiology [edit | edit code ]
The etiology and pathogenesis are not fully understood. There are more than 30 theories of the occurrence of eclampsia, the most common of which include:
- Genetic factors (gene defects: 7q36, eNOS, 7q23-ACE, HLA, AT2Р1, C677T - polymorphism);
- Thrombophilia (APS);
- Extragenital pathology;
- Infection.
There is not a single test that can reliably predict eclampsia [3].
The main trigger of preeclampsia is placental insufficiency [4] in combination with other maternal risk factors [5] .
Maternal risk factors [ edit | edit code ]
- Severe preeclampsia/eclampsia during previous pregnancies (RR - 7.19);
- Family history of severe preeclampsia/eclampsia (OR: 2.90);
- Multiple pregnancy (RR - 2.93);
- Chronic somatic diseases:
- Arterial hypertension;
- Kidney diseases;
- Diseases of the cardiovascular system;
- Diabetes mellitus (RR - 3.56);
- Obesity (BMI > 35) (RR - 2.47);
- First pregnancy (RR - 2.91);
- Antiphospholipid syndrome; (RR when combined with a history of preeclampsia > 9);
- Age over 40 years (OR - 2.1);
- The interval between births is more than 10 years (OR - 1.9).
Differential diagnosis of eclampsia
Seizures in epilepsy are very similar to those in eclampsia. But with epilepsy there will never be edema and high blood pressure, and in laboratory tests there will be no signs of kidney damage. Another important condition for distinguishing it from epilepsy is that eclampsia occurs only during pregnancy, childbirth or the postpartum period.
There are also dangerous conditions that can confuse the doctor and confuse eclampsia with uremic, hepatic or diabetic coma. Here, loss of consciousness also occurs and there may be convulsions, but due to organ failure. Uremic coma occurs when the kidneys fail and can be suspected by blood and urine tests. Hepatic coma often presents with jaundice, mental agitation, and dark urine. Diabetic coma occurs when the concentration of sugar in the blood is very low and its feature will be slow development, complaints of thirst, dizziness and weakness.
- mommy!
Eclampsia and preeclampsia - causes, symptoms, consequences - in pregnant women Stars flashed before their eyes. My head ached in the temple area. Weakness appeared in the body. Somehow I felt unwell and had a strange feeling in my stomach. The baby suddenly became quiet. On the display of the device for measuring blood pressure, the numbers 160 to 100 are frozen. Lie down, lie down, maybe it will go away slowly. Under no circumstances should you waste time. Only an immediate emergency call can save the baby and the woman, because eclampsia spares no one.
Eclampsia: what is it?
Pregnancy for a woman’s body is a serious test for all organs and systems. In most cases, the body adjusts to pregnancy, and all compensatory mechanisms work normally. But in a small percentage of cases, decompensation of functions occurs and gestosis develops (or, as it was previously called, late toxicosis), the extreme manifestation of which is eclampsia. Its main manifestations are loss of consciousness and convulsions due to high blood pressure. However, before these symptoms appear, there is almost always preeclampsia, which presents with a wide variety of symptoms. You need to pay attention to them and respond immediately.
Preeclampsia and eclampsia: what are the causes?
There are no unambiguous and clear reasons leading to gestosis and eclampsia. However, there are certain factors that contribute to the development of these extremely unpleasant conditions.
1. Hereditary factors
It has been proven that if the mother had eclampsia, then the daughter’s risk is very high. Inherited defective genes determine a woman’s predisposition to pregnancy complications.
2. Immune factors
A tendency to autoimmune processes in the body can become a background for the development of gestosis with disruption of compensatory mechanisms of adaptation to pregnancy.
3. High risk factors
Diseases of internal organs existing before pregnancy, to one degree or another, provoke the development of gestosis and eclampsia. Of these, it should be noted:
- -vascular diseases, of which the most important are arterial hypertension, a tendency to thrombosis, a decrease in the number of platelets, and the presence of thrombophilia proven by laboratory methods;
- endocrine diseases, manifested in the form of diabetes, obesity and metabolic syndrome;
- kidney diseases, of which chronic pyelonephritis and glomerulonephritis should be noted.
Risk factors include complications that a woman had during previous pregnancies. In particular, if the last time there was gestosis and preeclampsia, then these complications should be expected in all subsequent pregnancies.
Preeclampsia: what are the manifestations?
1. Subjective manifestations or how a woman will feel
During pregnancy, a woman may experience a wide variety of unpleasant sensations, but she needs to respond quickly if the following complaints occur, especially if they occur after 20 weeks of pregnancy and are combined with each other:
- - flashing stars or flies before the eyes;
- severe headaches;
- nausea and vomiting;
- pain in the upper abdomen.
2. Objective manifestations or what the doctor will notice
During each standard examination at the antenatal clinic, the doctor checks weight gain, blood pressure and the presence of edema. Among the tests, a general urine test taken the day before is evaluated. Using these data, it is possible to identify manifestations of gestosis and preeclampsia:
- - increased blood pressure;
- pronounced weight gain;
- presence of tissue swelling;
- the appearance of protein in the urine.
Even if there is a woman’s subjective sensations and high blood pressure, it is necessary to call an ambulance and provide emergency assistance to the pregnant woman. If there is swelling and protein in the urine, then this further aggravates the severity of gestosis.
Eclampsia: how does it manifest?
One of the most life-threatening complications during pregnancy for the mother and fetus is manifested by all the symptoms of preeclampsia, which are accompanied by loss of consciousness and convulsive syndrome, expressed as an attack of convulsions at a period of more than 20 weeks in the absence of epilepsy in the woman before pregnancy. As a rule, this extreme version of pregnancy complications occurs in cases where a woman is not seen in the antenatal clinic and is extremely irresponsible towards herself and her baby.
Preeclampsia and eclampsia: what are the complications?
1. From the fetus
The first thing you need to understand is that the baby suffers very much in this situation. In fact, an increase in blood pressure is a spasm of all blood vessels in the body. The blood that carries oxygen to the child stops flowing to him. The baby experiences severe oxygen starvation, which can cause:
- — fetoplacental insufficiency and fetal hypoxia;
- threatening fetal asphyxia;
- intrauterine death.
Mother's side
The organs and systems of a pregnant woman during acute vascular spasm experience no less oxygen stress. Depending on where in the body blood circulation is disrupted, the following serious complications can be identified:
- — disturbance of cerebral blood flow with the development of stroke;
- visual impairment up to retinal detachment;
- changes in blood flow in the area of the heart and lungs with the development of cardiac and respiratory failure;
- impaired liver function with the occurrence of jaundice, destruction of liver cells and the development of liver failure;
- changes in kidney function, leading to renal failure and a sharp decrease in the amount of urine produced;
- disruption of blood flow in the placenta, which causes premature placental abruption and bleeding from the uterus;
- the development of total intravascular coagulation, which will cause the formation of blood clots anywhere in the body.
Any of these complications can lead to severe pathology and death of the woman, which is why it is so important to notice and respond to the minimal symptoms of preeclampsia in time.
Preeclampsia and eclampsia: what are the tactics?
1. Help before the obstetric hospital
If a pregnant woman, while at home, feels a headache or spots appear before her eyes, then her blood pressure should be measured. For any readings exceeding the norm (120 to 80), you must call an ambulance. You don't need to take a blood pressure pill. This will be lost time, which is so necessary to save health and life.
If a woman comes to an antenatal clinic with complaints, and the doctor finds high blood pressure, then the woman will not be allowed to go home. A resuscitation ambulance team will be called. Before emergency assistance arrives, a woman with preeclampsia should be provided with strict bed rest and treatment aimed at lowering blood pressure. A team of resuscitators will provide emergency care on the spot, then on a stretcher (a pregnant woman with preeclampsia must absolutely not be moved to an upright position or led to the car with her feet) taken to the intensive care unit and taken to the perinatal center.
If convulsions suddenly begin, then, regardless of who is next to the woman, the following measures must be taken:
- — immediately call emergency medical assistance;
- try to protect the woman as much as possible from injury and damage, without actively trying to restrain her;
- turn the woman on her left side to prevent the tongue from retracting with difficulty breathing and vomit from entering the throat;
- after the convulsions have ended, use a napkin or handkerchief to clear the woman’s mouth of vomit so that she can breathe normally.
2. Help in the perinatal center
When a pregnant woman with preeclampsia is admitted to a perinatal center, the first step is to ensure stable blood pressure. Some medications have already been administered by the emergency resuscitator, so treatment is prescribed taking this into account.
Next, you need to quickly assess the condition of the woman and the fetus in order to decide on the method of delivery. It is necessary to understand that the only way to save the life of a woman and baby is to quickly rid the woman’s body of pregnancy. The decision on management tactics is made jointly by the obstetrician and the anesthesiologist-resuscitator.
If a woman has a full-term pregnancy, the birth canal is ready, the fetus is in good condition and blood pressure remains stable, then a natural birth is possible. Although this favorable combination of factors is very rare.
In case of a premature pregnancy and the ability to keep blood pressure within normal limits, the medical council may decide to delay delivery in order to try to prepare the fetal lungs as much as possible with the help of special drugs that accelerate the maturation of lung tissue.
If unfavorable conditions are created, an emergency caesarean section is performed. Indications for surgical delivery include:
- - presence of at least one convulsive seizure;
— placental abruption with bleeding;
- threatening asphyxia or severe fetal suffering according to the results of ultrasound or cardiotocography;
- swelling and hemorrhages in the fundus during examination by an ophthalmologist;
- symptoms of preeclampsia that do not go away within 6-12 hours of intensive treatment;
- complications of gestosis with the development of renal and liver failure.
In addition to delivery, it is necessary to carry out the entire range of therapeutic measures aimed at preserving the health and life of the woman. This assistance is provided by an anesthesiologist-resuscitator. If a convulsive syndrome occurs with loss of consciousness, the development of severe complications from vital organs (heart, lungs, brain), the woman is transferred to artificial pulmonary ventilation (ALV) with the entire complex of resuscitation medical care.
Preeclampsia and eclampsia: what will happen in the postpartum period?
After the birth of the child, it is necessary to continue treatment, because even in the absence of pregnancy, a seizure can occur. And this risk remains in the next 2 weeks after birth. The first week of treatment is carried out in the intensive care unit or in the intensive care ward. Then transfer to the postpartum ward is possible, subject to positive dynamics.
As a rule, if there are complications from organs and systems in a woman, further treatment is necessary in a specialized hospital (in cardiology, nephrology or neurology). Subsequently, rehabilitation is carried out on an outpatient basis under the supervision of an obstetrician-gynecologist, local therapist and specialized specialist.
Preeclampsia and eclampsia: what are the outcomes and consequences?
1. For the fetus
The consequences for the child largely depend on the speed of medical care, which is why it is so important to respond promptly to the first manifestations of preeclampsia. The chances of saving the life of the fetus are very high if you immediately call an ambulance at the first symptoms and end up in an obstetric hospital. The baby has an extremely low chance of survival if the seizure occurs far from the maternity hospital, when it is impossible to perform a caesarean section in the next few minutes.
2. For the mother
The consequences for a woman can affect the rest of her life. This is especially true for the consequences of the most severe variant - eclampsia. Circulatory disorders, even short-term, will affect the functions of organs and systems, causing the following diseases:
- — hypertension with constant use of antihypertensive pills;
— kidney pathology with the presence of protein and leukocytes in urine analysis;
— pathology of the nervous system caused by cerebral hypoxia;
— pathology of the cardiovascular system with an increased risk of thrombosis in any part of the body;
- liver pathology with the development of endocrine diseases.
The difficulty is that after suffering from preeclampsia and eclampsia, some of the problems in the body cannot be detected. Latent failure in any organ may gradually manifest itself over at least the next five years. Therefore, one of the strict recommendations for a woman is mandatory contraception, so that the next desired pregnancy occurs no earlier than in five years. And all this time you should be monitored by a therapist with regular examination using laboratory and diagnostic methods for detecting pathology.
Preeclampsia, manifested by certain complaints and increased blood pressure, is a reason to call emergency help, regardless of the stage of pregnancy. The occurrence of a convulsive seizure with loss of consciousness, which are signs of eclampsia, sharply reduces the ability of doctors to save the life of the mother and fetus. Only timely medical care can guarantee a woman’s continued health and life, and will also give her baby a real chance of survival.
Emergency care during an attack of eclampsia
Treatment begins immediately at the site of eclampsia. The goal of emergency care is to stop the seizures and create conditions for free breathing.
The first thing they do is turn the woman on her side, since in case of vomiting, the vomit can enter the lungs and cause suffocation. When a woman does not breathe for a long time, they begin to pump oxygen through a special mask. At the same time, anticonvulsants, such as magnesia, are administered. To stop repeated seizures or when the patient continues to be in a coma, muscle relaxants (drugs that relax the muscles) are administered.
In the case of prolonged seizures (about 30 minutes), this condition is considered as eclamptic status, in which their elimination using general anesthesia is indicated. Next, metabolism, blood acidity, fluid replenishment and toxin removal are carried out. A pregnant woman is examined by a neurologist to detect disorders of the nervous system. Blood is donated for hemoglobin, protein, sugar, to assess coagulation, liver function, concentration of trace elements (calcium, magnesium, potassium) and urine to identify kidney damage. That is, essentially all the indicators, since this is a serious condition in which there may be damage to internal organs, which needs to be diagnosed.
Prevention
Eclampsia – its prevention in women at risk.
So, knowing the main points of the appearance of eclampsia, symptoms, diagnosis, emergency care and treatment, now you need to remember the basic measures to prevent this dangerous pregnancy complication that occurs with severe preeclampsia. Based on the pathogenesis and statistical observations, all women who are at risk for the development of this complication from the beginning of pregnancy until the 20th week are recommended to take aspirin at a dose of 75-100 mg per day, and also if there is insufficient calcium intake from food, take a calcium supplement 1 g /day throughout pregnancy.
Prevention of eclampsia is carried out for all pregnant women with severe preeclampsia in order to prevent the occurrence of seizures and for this purpose a solution of magnesium sulfate is used.
To prevent eclampsia, the ineffectiveness of following a salt-free diet with protein foods, as well as taking vitamin C, folic acid, iron and vitamin E has been proven.
But first of all, the prevention of eclampsia is aimed at preventing late gestosis, their timely diagnosis, treatment and prevention. For this purpose, it is necessary to constantly monitor body weight, monitor blood pressure levels, urine tests and regular examinations by the attending physician, especially women at risk in the third trimester.
Is it necessary to give birth after eclampsia?
After eliminating the attack, it is necessary to urgently create conditions for childbirth. If the gestational age is more than 37 weeks (the baby is considered full-term) and the reproductive tract is ready for childbirth (sufficient opening of the cervix), then childbirth is carried out physiologically. In the absence of such conditions and an attack occurs during childbirth, a caesarean section is used.
Usually, doctors do not risk giving birth through the genital tract with preeclampsia or eclampsia and are more often inclined to have a caesarean section. In this case, this is the most gentle method of delivery. During delivery, anticonvulsants and blood pressure-lowering drugs are administered in parallel.
Prognosis for eclampsia
This condition is dangerous for the life of the child and mother. During an attack, a woman’s body can cope without medical help, but this is rare and often ends in the death of the fetus. Therefore, the prognosis is determined by how timely and effectively medical care was provided. With adequate treatment, the attack can be stopped and its further occurrence can be prevented, and urgent delivery will save the child’s life.
After eclampsia, persistent high blood pressure may occur, which carries a risk of stroke and cardiovascular diseases such as coronary heart disease, heart failure and arrhythmia. Therefore, the woman needs to consult a therapist and be hospitalized in the therapeutic department. Also, after eclampsia, mental disorders may occur, which requires a visit to a psychotherapist.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: Date of publication: 04/27/2018
Gynecologists - search service and appointment with gynecologists in Moscow
What is postpartum preeclampsia?
Preeclampsia is an increase in blood pressure along with an increase in protein in the urine of women during pregnancy. Sometimes preeclampsia can develop soon after giving birth, in which case it is called postpartum preeclampsia. Postpartum preeclampsia is a rare condition that develops in women shortly after giving birth. It can occur literally a couple of days after birth, or several weeks after this event. Postpartum preeclampsia also causes increased levels of protein in the urine. As already mentioned, this disease is rare and should not be confused with common preeclampsia. Preeclampsia is an increase in blood pressure during pregnancy.