Overdose
An overdose of Butorphanol occurs when a large dose of the drug is administered or it is used simultaneously with alcohol, benzodiazepines, barbiturates, and other opioids. The key symptom is respiratory depression (hypoventilation). Dizziness, confusion, drowsiness, fatigue and weakness develop. Sticky sweat appears on the skin, breathing becomes difficult, and the heartbeat becomes uneven. Blood pressure decreases, pupils narrow, and convulsions occur. The patient experiences anxiety and restlessness. In severe cases, he loses consciousness and falls into a coma. In the absence of emergency medical assistance, breathing slows down and death occurs.
Release form and composition
Colorless, transparent or slightly opalescent solution 2 mg/ml for intramuscular or intravenous administration. Available in:
- Ampoules, volume 1 ml, transparent or dark glass (in blister packs of 5 pieces, in a cardboard pack 1, 2, 4, 10 or 20 packs, packs are equipped with an ampoule knife);
- Syringe tubes, volume 1 ml (1, 2 or 5 syringe tubes in a cardboard pack).
The active ingredient is butorphanol tartrate.
Auxiliary components: Trilon B, sodium citrate, citric acid, sodium chloride, water for injection.
Indications
The use of Butorphanol is indicated for the following diseases and conditions:
- To relieve pain caused by cancer
- For severe pain syndromes of various origins
- For pain relief during surgical interventions
- For premedication and postoperative period
- During childbirth, if the fetus shows no signs of intrauterine pathology
Contraindications
Contraindications to the use of Butorphanol are:
- Increased intracranial pressure;
- Respiratory depression;
- Traumatic brain injuries;
- CNS depression;
- Alcoholic psychosis and acute alcoholic states;
- Convulsions;
- Kidney and liver failure;
- Bronchial asthma;
- Arterial hypertension;
- Heart failure;
- Heart rhythm disturbances;
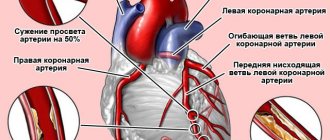
- Acute myocardial infarction;
- Acute surgical diseases of the abdominal organs (before diagnosis);
- Drug dependence on morphine-like drugs (Promedol, Morphine, Fentanyl).
- Hypersensitivity to the components of the drug;
- Pregnancy and lactation (except for pain relief during childbirth and preparation for it);
- Age up to 18 years.
The drug is not prescribed during treatment with MAO inhibitors, or within 2 weeks after their discontinuation.
Use with caution in old age (after 65 years).
Addiction treatment
The fight against addiction begins with stopping the administration of Butorphanol. To alleviate withdrawal symptoms and speed up the detoxification process, the patient is prescribed opioid receptor antagonists (Naloxone, Naltrexone), as well as painkillers, vitamins, saline drips, and sedatives. After the withdrawal syndrome ends, a course of psychotherapy begins, which helps the patient cope with psychological dependence. Attendance at support groups, occupational therapy, rehabilitation at home, and return to professional activity may be recommended.
Directions for use and dosage
The drug is administered intravenously or intramuscularly. The dose of the drug is determined individually by the attending physician.
Depending on the age and condition of the patient, the drug is administered in the following dosages:
- To relieve pain – 1 mg intravenously or 2 mg intramuscularly, every 3-4 hours as needed;
- For premedication - 2 mg intramuscularly 1-1.5 hours before surgery or the same dose intravenously immediately before surgery;
- When performing general anesthesia - 2 mg intravenously, before the introduction of sodium thiopental, then add 0.5-1 mg to maintain the required depth of anesthesia. The full dose of Butorphanol required for general anesthesia can vary from 4 to 12.5 mg;
- During childbirth - 1-2 mg of the drug intramuscularly or intravenously, for women in labor at least 37 weeks of pregnancy, only if the fetus has no signs of intrauterine pathology. The drug should not be administered more than once every 4 hours; the last injection should be given at least 4 hours before delivery.
For elderly people (over 65 years old), it is recommended to reduce the dose by 2 times, and increase the interval between doses to 6 hours.
Pharmacological properties of the drug Butorphanol
Synthetic opioid analgesic of the phenanthrene series. Butorphanol and its main metabolites are κ-class opiate receptor agonists and μ-opiate receptor antagonists. The interaction of butorphanol with these receptors in the central nervous system provides most of its pharmacological effects. In addition to the central analgesic, it has a sedative effect, reduces the excitability of the cough center, stimulates the gag reflex, and also causes miosis. Effects that may not be related to the central nervous system include changes in hemodynamics, bronchial tone, secretory and motor activity of the digestive tract, and bladder sphincter tone. Like other high-affinity κ-receptor opiate agonist-antagonists, butorphanol may cause unwanted psychotomimetic effects. At a dose of 1-2 mg or higher, by any route of administration, may cause nausea and/or vomiting and respiratory depression. Butorphanol exhibits an antitussive effect, increases pulmonary artery pressure, vascular resistance, increases end-diastolic pressure in the left ventricle and systemic blood pressure. The analgesic effect depends on the route of administration and appears a few minutes after intravenous administration and within 10–15 minutes after intramuscular administration. The maximum analgesic effect is observed 30–60 minutes after IV or IM administration. The average duration of the analgesic effect after IM and IV administration is 3–4 hours, after which repeated administration is required in 50% of cases.
Side effects
The most common use of Butorphanol can cause dizziness, drowsiness, nausea and vomiting. Other side effects from organs and systems are rarely possible:
- Organs of the gastrointestinal tract: rarely - constipation, anorexia, dryness of the oral mucosa, epigastric pain;
- Cardiovascular system and blood (hemostasis, hematopoiesis): rarely - palpitations, vasodilation; extremely rarely - fainting, decreased or increased blood pressure, chest pain, tachycardia;
- Nervous system and sensory organs: rarely - euphoria, confusion, anxiety, nervousness, insomnia, drowsiness, paresthesia, headache, asthenia, tremor, tinnitus, eye pain, blurred vision, lethargy; extremely rarely - agitation, hostility, unusual dreams, dysphoria, hallucinations, vertigo, depression, withdrawal syndrome;
- Allergic reactions: extremely rarely - urticaria, rash;
- Other: rarely - itching, increased sweating, feeling of heat; extremely rarely – shallow breathing, decreased urination.
Also during post-marketing observations, the following were noted: convulsions, apnea, delirium, transient difficulty in movement and speech (associated with excessive influence of the drug), drug dependence.
Side effects that can cause an overdose of Butorphanol: hypothermia, arterial hypotension, cardiovascular failure, hypoventilation, stuporous or comatose state. In case of overdose, it is necessary to maintain adequate pulmonary ventilation, systemic hemodynamics and body temperature. In case of respiratory depression, it is possible to administer the specific opioid antagonist Naloxone - 0.4-2 mg intravenously. The patient should be provided with continuous monitoring and, if necessary, perform artificial ventilation.
Analogs
Among other opiates, it is worth highlighting Nalbuk, which is a direct analogue of Butorphanol. Nalbuphine, which is part of it, has the same therapeutic effects as Butorphanol, but with a lesser degree of influence on the respiratory center.
Also, Nalbuk is not characterized by the development of side effects from the cardiovascular system. It is distinguished by an almost complete absence of predisposition to the development of addiction. It is important to note that Nalbuk is a potent substance, therefore it is subject to quantitative accounting within a medical institution and is not sold in retail pharmacies.
It is not always possible to use a powerful opioid analgesic, especially when it comes to chronic pain. In this case, it will be effective to prescribe similar drugs that will be safer and will not cause addiction:
- One of the most effective drugs from the NSAID group is Diclofenac sodium. It realizes its analgesic effect by inhibiting cyclooxygenase-2, thereby reducing the production of prostaglandins of the E2 and E2-alpha classes. Diclofenac effectively copes with moderate pain syndrome and is also recommended in case of a migraine attack.
The drug is freely available and has a fairly low cost and wide distribution. Of the side effects, the most common may be disorders of the blood coagulation system, so taking the drug and adjusting doses should only be carried out under the supervision of the attending physician.
Features of the drug - Paracetamol stands apart in the group of analgesics, despite the fact that the principle of action is based on reducing the level of prostaglandins by inhibiting COX. However, this happens not only within the local focus of inflammation, but also in the central nervous system. The excitability of the thermoregulation center is also reduced, which makes it possible to obtain a pyrolytic effect.
The drug helps fight headaches and toothaches of varying intensity, as well as neuralgia and sciatica. The main side effect that must be taken into account when prescribing the drug is its hepatotoxicity. Therefore, for people with liver failure, use should be carried out taking into account risk and benefit indicators.
special instructions
Before starting therapy with Butorphanol, it is necessary to carry out a set of measures aimed at the complete elimination of narcotic substances from the body in patients with a history of drug addiction.
In preparation for childbirth, the drug can be prescribed only under close medical supervision.
During the treatment period, you should not engage in potentially hazardous types of work that require increased attention and high speed of psychomotor reactions.
You should not consume ethanol throughout the course of treatment.
It is not recommended to use the drug as an anesthetic for short-term surgical interventions, as long-term post-anesthesia respiratory depression is possible.
The drug should not be combined with other opioid analgesics, since there is a high probability of weakening analgesia and provoking withdrawal symptoms in patients with opioid dependence.
When using sleeping pills and general anesthesia, in order to avoid excessive suppression of the activity of the respiratory center and increased depression of the central nervous system, the drug is taken in reduced doses and under close medical supervision.
Please note that Butorphanol:
- Pharmaceutically incompatible with barbiturates, diazepam;
- Loses effectiveness when used simultaneously with local vasoconstrictors administered intranasally;
- Enhances the effect of drugs that depress the central nervous system (anxiolytics, barbiturates, antipsychotics, ethanol, histamine H1 receptor blockers).
Consequences of dependence on Butorphanol
Since Butorphanol is administered intravenously, among drug addicts there is a high risk of contracting infectious diseases - hepatitis, syphilis, HIV infection. The drug inhibits the cough reflex and at the same time reduces the activity of the immune system, which leads to the development of bronchitis and pneumonia. Often these diseases remain undiagnosed and lead to death in those who regularly took Butorphanol. The drug also leads to the following complications:
- toxic liver damage
- phlebitis, scars on veins, suppuration in the area of drug administration
- tooth decay
- impotence
- decreased intelligence
- personality degradation
Overdose
Symptoms:
- Decreased body temperature
- Drop in blood pressure
- Stupor or coma
- Cardiovascular failure
- Shallow breathing (hypoventilation)
Treatment:
- Artificial ventilation
- Maintaining systemic hemodynamics and adequate body temperature
- When the respiratory center is depressed, the opioid antagonist Nolaxon is used at a dosage of 0.4-2 mg intravenously