This term has other meanings, see Adrenaline (meanings).
| Adrenalin | |
| Epinephrine | |
| Chemical compound | |
| IUPAC | (R)-4-[1-hydroxy-2-(methylamino)ethyl]-benzene-1,2-diol |
| Gross formula | C9H13NO3 |
| CAS | 51-43-4 |
| PubChem | 5816 |
| DrugBank | 00668 |
| Classification | |
| Pharmacol. group | Adrenergic and sympathomimetics (alpha, beta). Hypertensive drugs[1] |
| ATX | A01AD01, B02BC09, C01CA24, R01AA14, R03AA01, S01EA01 |
| ICD-10 | 16.216.2, 40.140.1, 45., 57., 78.278.2, 79.479.4, 81.181.1[1] |
| Dosage forms | |
| solution 1 mg/ml, 1.8 mg/ml for injection; solution 0.1% for topical use; 1% solution for external use; homeopathic tincture substance; powder substance[2] | |
| Other names | |
| adrenaline, synthetic adrenaline, adrenaline hydrotartrate, adrenaline hydrochloride, "Adrenaline hydrochloride-Vial", epinephrine hydrotartrate[2] | |
| Media files on Wikimedia Commons | |
Adrenaline (epinephrine)
(L-1 (3,4-Dihydroxyphenyl)-2-methylaminoethanol) is a hormone that is synthesized by the adrenal medulla. Produced by the body from tyrosine, an amino acid supplied with food[3]. Adrenaline is also formed when the autonomic nervous system is excited (at the synapses of nerve fibers)[4].
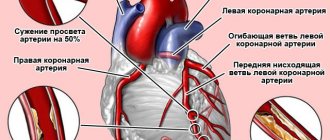
The hormone constricts blood vessels, especially in the abdominal cavity. The volume of blood in the body is redistributed, from the liver and spleen it flows into the vessels of the body, replenishing the volume of blood circulating in them, as a result of which the vessels leading to the heart and brain expand, and the blood supply to the organs improves[5].
Its chemical structure is a catecholamine. Adrenaline is found in various organs and tissues; it is produced in significant quantities in chromaffin tissue. Plays an important role in the physiological fight-or-flight response. Recent research by scientists has shown that osteocalcin plays an equally important role in triggering this reaction [6].
Synthetic adrenaline is used as a medicine under the name Epinephrine (INN).
In American literature, adrenaline is called epinephrine, both names mean the same thing, “near the kidney,” but in the first case Latin is used, and in the second Greek. The two names exist in parallel to this day and reflect more than a century of dispute between American and English universities over what the compound was that was named epinephrine more than 120 years ago.[7]
Chemical properties
Epinephrine - what is it?
One of the most important neurotransmitters , the main hormone produced by the adrenal medulla. Another name for the drug is adrenaline . Based on its entire chemical structure, the substance can be classified as a catecholamine . Epinephrine is synthetic adrenaline .
Normally, the compound is found in various tissues and organs and is produced by chromaffin tissue, especially the adrenal medulla. Epinephrine on Wikipedia is described in the article about adrenaline , it affects alpha and beta adrenergic receptors , and activates the processes of excitation of sympathetic nerve fibers.
During times of stress, with a sense of danger, fear and anxiety, burns, injuries, the concentration of adrenaline in the body increases, activating a chain of “fight or flight” reactions. Adrenaline takes part in many types of metabolism, affects tissue metabolism and glucose , enhances glycogenolysis and gluconeogenesis glycogen synthesis in liver tissue and muscles, enhances the breakdown of fats and protein catabolism.
There are various forms of release of Epinephrine. The compound is sold in the form of homeopathic granules or drops for oral administration, injection solutions of various dosages, solutions for topical use, as a powder substance or tincture substance.
Story
The physiological effect of adrenal gland extracts on the cardiovascular system was first described in articles by the Englishmen Oliver and Schaefer[8] and the Pole Napoleon Cybulski,[9] published almost simultaneously. The British published their article in English in the journal J Physiol
, and Napoleon Cybulski described his research in Polish in a preprint from the Jagiellonian University, so his work is little known. Both studies referred to “physiologically active adrenal gland extracts” and no active substance was identified.
A couple of years later, John Jacob Abel, who by the end of his life would be called the father of American pharmacology, obtained from these extracts a crystalline substance that had the property of increasing blood pressure[10]. Abel gave it the name epinephrine, which in Greek means “above the kidney.” At the same time, the German von Früth also isolated a compound from the adrenal glands, which he called suprarenin [11]. However, both of these substances had slightly different physiological effects from the extract itself.
A couple of years later, the Japanese Jokichi Takamine[en], after visiting Abel’s laboratory at Johns Hopkins University, figured out to use an additional purification stage and patented the substance he isolated,[12] and the pharmaceutical company Parke-Davis released it for sale under the trade name “Adrenaline.”
Future Nobel laureate Henry Dale worked with adrenaline for many years, trying to understand the mechanism of its action on different cells. Dale insisted that the compound obtained by Takamine could not be called epinephrine, since it differed in a number of properties from Abel's epinephrine[13]. Dale thought the name adrenaline should be used.
Currently, most researchers in the USA, Canada and Japan use the name “epinephrine”; in all other countries the name “adrenaline” is more common [7].
Although the hormone itself is called epinephrine in the United States, its receptors are called adrenoreceptors, and epinephrine-like compounds are called adrenergic agonist/antagonist.
Pharmacodynamics and pharmacokinetics
Synthetic adrenaline - Epinephrine activates the enzyme adenylate cyclase at the cellular level, increases the intracellular concentration of calcium ions and cAMP . The substance stimulates alpha-adrenergic receptors and beta-adrenergic receptors , increases blood pressure, constricts blood vessels in the abdominal organs, skin and mucous membranes, skeletal muscles, while dilating the blood vessels of the brain. The pressor effect after administration of the drug is not as pronounced as after an injection of norepinephrine .
If the rate of administration of the drug is low enough (less than 0.01 mcg per kg of patient weight per minute), then there is a possibility of a decrease in blood pressure due to dilation of the blood vessels of the skeletal muscles. At a sufficiently high rate of administration (from 0.04 to 0.1 mcg per kg per minute) and dosage, Epinephrine increases heart rate and cardiovascular system, minute volume of blood circulation and stroke volume of blood. In this case, a decrease in total peripheral vascular resistance is observed. If the infusion rate is more than 0.02 mcg per kg of body weight per minute, then systolic blood pressure and total peripheral vascular resistance increase.
By changing cardiac activity and stimulating beta-adrenergic receptors of the heart muscle, Epinephrine significantly increases and speeds up heart contractions, facilitates atrioventricular conduction, which can lead to the development of arrhythmias , transient reflex bradycardia .
The substance also has a multidirectional effect on smooth muscles. It relaxes the muscles of the bronchi and intestines, but leads to pupil dilation. Due to stimulation of the processes of removal of potassium ions from cells, the use of the substance can lead to hypokalemia .
The drug increases the oxygen demand of the heart muscle and prevents the development of bronchiole edema . The medicine also reduces the rate of absorption of local anesthetics , increases the duration of action and reduces the toxicity of local anesthetics.
Despite the fact that Epinephrine stimulates the central nervous system, it does not penetrate the BBB well. The product stimulates activity and releases mental energy, helps to mobilize the body's strength, and causes a feeling of anxiety and tension.
The product has a pronounced anti-allergic and anti-inflammatory effect , slows down the production of kinins, histamine, serotonin, leukotrienes and prostaglandins , inflammatory mediators . The substance also increases the level of leukocytes in the blood (removes them from the depot in the spleen and redistributes the formed elements of the blood). Adrenaline has the ability to reduce blood flow to the cavernous bodies and stimulate blood clotting.
When administered intravenously, the effect of the drug is observed instantly, the duration of action is up to 2 minutes. After subcutaneous administration, changes in the condition are observed after 5-10 minutes, with a peak after 20.
The substance is well absorbed after intramuscular or subcutaneous administration, but is destroyed quite quickly. The drug is quite completely absorbed into the systemic circulation after endotracheal and conjunctival use . After injection, maximum concentration is achieved within 3-10 minutes.
The compound crosses the placental barrier and is excreted in breast milk. Metabolism of the substance occurs in the liver, COMT and MAO endings of sympathetic nerves and tissues. The medicine is excreted by the kidneys in the form of vanillylmandelic acid , glucuronides , sulfates and slightly unchanged.
Areas of use and indications
Indications for the use of single drugs containing epinephrine:
- anaphylactic shock;
- bronchospasm;
- asystole;
- a sharp drop in blood pressure that is not amenable to other therapy;
- bleeding (locally);
- for pupil dilation during ophthalmological operations;
- relief of prolonged and painful erection (priapism);
- hypoglycemia due to insulin overdose (a sharp drop in blood glucose levels);
- to prolong the effect of local anesthetics.
By influencing α-adrenergic receptors of the skin and mucous membranes, epinephrine (adrenaline) reduces the rate of absorption of local anesthetics and increases the period of their action. This feature has found wide application in dentistry and maxillofacial surgery.
By combining the local anesthetic articaine with epinephrine (in various concentrations) in one preparation, it is possible to achieve a quick and powerful analgesic effect lasting from 45 to 75 minutes. The drugs are administered only into non-inflamed tissue of the oral cavity and allow, with comfort for the patient, simple dental treatment, as well as prosthetics, implantation and other dental operations on the mucous membrane and bones.
Indications for use
Epinephrine Hydrochloride is used:
- to eliminate immediate allergic reactions ( Quincke's edema, anaphylactic shock, urticaria ), which developed as a result of drug allergies , blood transfusions, consumption of food, the introduction of other allergens or insect bites;
- with asystole , including against the background 3rd degree AV block
- to relieve an attack of bronchial asthma ;
- for bronchospasm that occurs during the use of anesthesia ;
- if it is necessary to prolong the effect of local painkillers;
- with arterial hypotension , which cannot be treated with replacement fluids (after injuries, in shock, with bacteremia , open heart surgery, with renal failure, drug overdose, heart failure);
- in patients with hypoglycemia insulin overdose ;
- for open-angle glaucoma , if eye surgery is required in order to dilate the pupil and relieve intraocular pressure ;
- to stop bleeding;
- in the treatment of priapism .
Physiological role
Adrenaline is produced by neuroendocrine cells of the adrenal medulla and is involved in a state in which the body mobilizes to eliminate a threat (“fight or flight”).
Conditions for increased secretion
Its secretion increases sharply during stressful conditions, borderline situations, feelings of danger, anxiety, fear, injuries, burns and shock. The content of adrenaline in the blood increases, including with increased muscular work.
Action
The effect of adrenaline is associated with the effect on α- and β-adrenergic receptors and largely coincides with the effects of excitation of sympathetic nerve fibers.
It causes vasoconstriction of the abdominal organs, skin and mucous membranes; to a lesser extent constricts the vessels of skeletal muscles, but dilates the vessels of the brain. Blood pressure increases under the influence of adrenaline.
However, the pressor effect of adrenaline is less pronounced than that of norepinephrine due to the excitation of not only α1 and α2-adrenergic receptors, but also vascular β2-adrenergic receptors (see below).
Effect on the heart
Changes in cardiac activity are complex: by stimulating β1-adrenergic receptors of the heart, adrenaline contributes to a significant increase and acceleration of heart contractions, facilitating atrioventricular conduction, and increasing the automaticity of the heart muscle, which can lead to arrhythmias. However, due to an increase in blood pressure, the center of the vagus nerves is excited, which has an inhibitory effect on the heart, and transient reflex bradycardia may occur. Adrenaline has complex effects on blood pressure. There are 4 phases of its action (see diagram):
- Cardiac, associated with stimulation of β1-adrenergic receptors and manifested by an increase in systolic blood pressure due to an increase in cardiac output;
- Vagal, associated with stimulation of the baroreceptors of the aortic arch and carotid glomerulus by increased systolic output. This leads to activation of the dorsal nucleus of the vagus nerve and activates the baroreceptor depressor reflex. The phase is characterized by a slowing of the heart rate (reflex bradycardia) and a temporary cessation of the rise in blood pressure;
- Vascular pressor, in which the peripheral vasopressor effects of adrenaline “defeat” the vagal phase. The phase is associated with stimulation of α1- and α2-adrenergic receptors and is manifested by a further increase in blood pressure. Adrenaline, stimulating β1-adrenergic receptors of the juxtaglomerular apparatus of the nephrons of the kidneys, increases the secretion of renin, activating the renin-angiotensin-aldosterone system, which is also responsible for increasing blood pressure.
- Vascular depressor, depending on the excitation of vascular β2-adrenergic receptors and accompanied by a decrease in blood pressure. These receptors last the longest to respond to adrenaline.
Phases of action of adrenaline on blood pressure
Effect on smooth muscle
Adrenaline has a multidirectional effect on smooth muscles, depending on the presence of different types of adrenergic receptors in them. By stimulating β2-adrenergic receptors, adrenaline causes relaxation of the smooth muscles of the bronchi and intestines, and by stimulating α1-adrenergic receptors of the radial muscle of the iris, adrenaline dilates the pupil.
Long-term stimulation of β2-adrenergic receptors is accompanied by increased removal of K+ from the cell and can lead to hypokalemia.
Effect on metabolism
Adrenaline is a catabolic hormone and affects almost all types of metabolism. Under its influence, there is an increase in blood glucose and increased tissue metabolism. Being a counter-insular(?) hormone and acting on β2-adrenergic receptors of tissues and the liver, adrenaline enhances gluconeogenesis and glycogenolysis, inhibits glycogen synthesis in the liver and skeletal muscles, enhances the uptake and utilization of glucose by tissues, increasing the activity of glycolytic enzymes. Adrenaline also enhances lipolysis (fat breakdown) and inhibits fat synthesis. This is ensured by its effect on β3-adrenergic receptors in adipose tissue. At high concentrations, adrenaline enhances protein catabolism.
Effect on skeletal muscles and myocardium
By simulating the effects of stimulation of “trophic” sympathetic nerve fibers, adrenaline in moderate concentrations that do not have an excessive catabolic effect has a trophic effect on the myocardium and skeletal muscles. Adrenaline improves the functional ability of skeletal muscles (especially during fatigue).
With prolonged exposure to moderate concentrations of adrenaline, an increase in the size (functional hypertrophy) of the myocardium and skeletal muscles is noted. Presumably this effect is one of the body’s adaptation mechanisms to long-term chronic stress and increased physical activity.
However, prolonged exposure to high concentrations of adrenaline leads to increased protein catabolism, decreased muscle mass and strength, weight loss and exhaustion. This explains emaciation and exhaustion during distress (stress that exceeds the body's adaptive capabilities).
Effect on the nervous system
Adrenaline has a stimulating effect on the central nervous system, although it poorly penetrates the blood-brain barrier. It increases the level of wakefulness, mental energy and activity, causes mental mobilization, orientation reaction and feelings of anxiety, restlessness or tension.
Adrenaline excites the area of the hypothalamus responsible for the synthesis of corticotropin releasing hormone, activating the hypothalamic-pituitary-adrenal system and the synthesis of adrenocorticotropic hormone. The resulting increase in the concentration of cortisol in the blood enhances the effect of adrenaline on tissues and increases the body's resistance to stress and shock.
Anti-allergic and anti-inflammatory effect
Adrenaline has a pronounced anti-allergic and anti-inflammatory effect, inhibits the release of histamine, serotonin, kinins, prostaglandins, leukotrienes and other mediators of allergy and inflammation from mast cells (membrane stabilizing effect), stimulating the β2-adrenergic receptors located on them, and reduces the sensitivity of tissues to these substances. This, as well as stimulation of β2-adrenergic receptors of bronchioles, eliminates their spasm and prevents the development of edema of the mucous membrane.
Adrenaline causes an increase in the number of leukocytes in the blood, partly due to the release of leukocytes from the depot in the spleen, partly due to the redistribution of blood cells during vasospasm, partly due to the release of incompletely mature leukocytes from the bone marrow depot. One of the physiological mechanisms for limiting inflammatory and allergic reactions is an increase in the secretion of adrenaline by the adrenal medulla, which occurs during many acute infections, inflammatory processes, and allergic reactions. The antiallergic effect of adrenaline is also associated with its effect on the synthesis of cortisol.
Effect on erection
Sexual arousal disappears.
When administered intracavernosally, it reduces blood supply to the cavernous bodies, acting through α-adrenergic receptors.
Hemostatic effect
Adrenaline has a stimulating effect on the blood coagulation system. It increases the number and functional activity of platelets, which, along with spasm of small capillaries, determines the hemostatic (hemostatic) effect of adrenaline. One of the physiological mechanisms promoting hemostasis is an increase in the concentration of adrenaline in the blood during blood loss.
Contraindications
Epinephrine should not be used:
- if you have hypersensitivity to this substance;
- patients with high blood pressure ;
- for ischemic heart disease and tachyarrhythmia ;
- persons with ventricular fibrillation ;
- pregnant women;
- with pheochromocytoma ;
- during lactation;
- with hypertrophic cardiomyopathy .
During treatment, special care should be taken:
- patients with metabolic acidosis ;
- with hypercapnia ;
- after cold injury;
- for atrial fibrillation, ventricular arrhythmia and hypoxia ;
- patients with pulmonary hypertension ;
- after myocardial infarction ;
- with hemorrhagic, cardiogenic, traumatic or any other shock not caused by allergies;
- patients with thyrotoxicosis ;
- for occlusive vascular diseases;
- patients with atherosclerosis or Buerger's disease ;
- for diabetic endarteritis ;
- patients with Raynaud's disease ;
- for cerebral atherosclerosis ;
- patients with diabetes mellitus or closed-angle glaucoma ;
- patients with Parkinson's disease ;
- with increased convulsive activity;
- if inhalation agents for general anesthesia ( cyclopropane, Ftorotan, chloroform ) are used at the same time;
- with prostatic hypertrophy ;
- elderly patients;
- children.
Side effects
After administration of the drug, the following may develop:
- angina pectoris, tachycardia , palpitations, bradycardia , increased or decreased blood pressure ;
- ventricular arrhythmia , chest pain, cardiac arrhythmia (high dosages of the drug);
- anxiety, tremor , headaches, dizziness;
- less often than usual - feeling tired, feeling hot or cold, nervousness ;
- insomnia , spontaneous muscle contractions, nervous system excitement, memory loss, disorientation , panic and aggression, paranoia , disorders similar to schizophrenia (rare);
- vomiting, problems with urination, pain during urination, nausea;
- allergic skin rashes, bronchospasm , angioedema , erythema multiforme ;
- sweating, hypokalemia – rare;
- cramps , persistent and strong erection , muscle tightening.
During intramuscular injection, pain and burning may occur at the injection site.
Pharmacokinetics
When administered intramuscularly or subcutaneously, it is absorbed unpredictably, since it has a direct pressor effect on the capillaries at the injection site, significantly slowing down the entry into the systemic circulation and therefore, in emergency cases, when intravenous administration is not possible, it is administered intratracheally or intracorporeally. Introduction into soft tissues is used in the form of injection only to block the absorption of an allergenic substance that was introduced earlier and caused a pathological reaction, when providing assistance for anaphylactic shock, and sometimes to stop capillary or parenchymal bleeding [14] [15]. When administered intravenously, it begins to act almost instantly. It is also absorbed after endotracheal and conjunctival administration. When administered parenterally, it is quickly destroyed[16]. Penetrates through the placenta, into breast milk, does not penetrate the blood-brain barrier.
Metabolized mainly by MAO and COMT in the endings of sympathetic nerves and other tissues, as well as in the liver with the formation of inactive metabolites. The half-life for intravenous administration is 1-2 minutes.
Excreted by the kidneys mainly in the form of metabolites: vanillylmandelic acid, metanephrine, sulfates, glucuronides; and also in very small quantities - unchanged [2].
Epinephrine, instructions for use (Method and dosage)
Most often, the drug is prescribed subcutaneously or intramuscularly . Less commonly, it is administered intravenously .
Epinephrine, instructions for use
As a vasoconstrictor, the medicine is recommended to be administered intravenously , by drip . The infusion rate is 1 mcg per minute, with the possibility of further increasing to 10 mcg per minute.
For anaphylactic shock, the drug is administered slowly intravenously. sodium chloride solution . If necessary, you can continue to administer the drug at a concentration of 0.1 m per ml. If the patient's condition is more stable, then intramuscular or subcutaneous administration of 0.3-0.5 mg of the drug is recommended. If necessary, you can give a second injection after 10-20 minutes and another after the same period of time.
To relieve an attack of bronchial asthma, it is recommended to administer 0.3-0.5 mg of diluted or undiluted Epinephrine solution subcutaneously. If necessary, an additional dose can be administered after 20 minutes (up to 3 times). Also indicated are intravenous injections of the drug at 0.1-0.25 mg in solution with sodium chloride , concentration 0.1 mg per 1 ml.
To extend the duration of action of the local anesthetic, 5 mcg per ml is prescribed. 0.2-0.4 mg of the drug is used as spinal anesthesia
To stop bleeding, the substance is used topically. A tampon moistened with a solution of the drug is placed on the bleeding area.
For asystole, intracardiac injections sodium chloride solution in a ratio of 0.5 mg of substance per 10 ml of solvent, are prescribed During resuscitation, intravenous injections of diluted medication are used every 3-5 minutes. For endotracheal instillation, the optimal dosage is determined by the doctor; it should be 2-2.5 times greater than the dosage for intravenous injection.
For asystole in newborns, the medicine is administered slowly intravenously at 10-30 mcg per kg of the child’s weight. The frequency of injections is every 3-5 minutes. If the child is more than 1 month old, use higher dosages of the drug. The drug can also be administered endotracheally .
To eliminate anaphylactic shock in children, the substance is used subcutaneously or intramuscularly at 10 mg per kg of child weight. The maximum dosage is 0.3 mg. If necessary, the medicine can be administered every 15 minutes, no more than 3 times.
For bronchospasm in children, up to 0.3 mg of the drug is used subcutaneously. Injections can be repeated every 15 minutes up to 4 times.
Treatment of open-angle glaucoma is carried out by instilling one drop of 1-2% Epinephrine solution into the affected eye, 2 times a day. The duration of treatment is determined by the doctor.
Composition of the drug
Epinephrine is a foreign name, when in domestic medicine the drug is more commonly defined as Adrenaline
. It is a white or slightly pinkish crystalline powder. Subject to change under the influence of light and air. It is used medically in the form of a 0.1% solution.
The Epinephrine solution itself is prepared with the addition of 0.01 N. hydrochloric acid. The resulting substance is colorless and transparent and cannot be heated.
Overdose
In case of overdose, the following symptoms occur: a strong increase in blood pressure , bradycardia and tachycardia , ventricular or atrial , pale skin, cold sweat, headache, nausea and vomiting, metabolic acidosis . Myocardial infarction , cerebral hemorrhage (especially in old age), and pulmonary edema may develop . In extreme cases, death.
As treatment, it is indicated to stop the infusion or injection of the drug and provide symptomatic therapy aimed at maintaining the functioning of the cardiovascular system and normalizing blood pressure. Alpha-blockers (for example, phentolamine ), beta-blockers ( propranolol ) are also administered
Interaction
Alpha and beta adrenergic receptor blockers are antagonists of this substance.
When the substance is combined with ergot alkaloids, the vasoconstrictor effect of taking medications is enhanced gangrene and severe ischemia .
The pressor effect of taking the drug is potentiated by the action of non-selective beta-blockers .
When combined with drugs that prolong the QT ( cisapride, astemizolol, terfenadine ), the drug helps to further increase the duration of the QT interval.
It is highly not recommended to combine the drug with cardiac glycosides, quinidine, dopamine, chloroform, halothane, methoxyflurane, enflurane, tricyclic antidepressants, isoflurane, cocaine due to the increased risk of developing cardiac arrhythmia .
The combined use of Epinephrine with sympathomimetics increases the load on the heart and can lead to side effects from the cardiovascular system.
The medicine reduces the effectiveness of antihypertensive drugs (for example, diuretics ).
The effect of taking Epinephrine is enhanced by the action of MAO inhibitors, m-anticholinergics, thyroid hormones, reserpine, ganglion blockers, octadine .
The substance weakens the effect of insulin , hypoglycemic agents , cholinomimetics , opioid painkillers , neuroleptics, muscle relaxants, and hypnotics .
Content
- 1. History
- 2 Physiological role 2.1 Conditions for increased secretion
- 2.2 Action
- 2.3 Effect on the heart
- 2.4 Effect on smooth muscle
- 2.5 Effect on metabolism
- 2.6 Effect on skeletal muscle and myocardium
- 2.7 Effect on the nervous system
- 2.8 Antiallergic and anti-inflammatory effects
- 2.9 Effect on erection
- 2.10 Hemostatic effect
- 5.1 Indications
- 6.1 Overdose
special instructions
The substance is not recommended for use after myocardial infarction , as it can provoke ischemia .
During infusion, a measuring device must be used to regulate the rate of administration of the substance. It is best if the infusion is carried out into a large vein, preferably a central one.
Intracardiac administration of the drug is recommended only in emergency cases, if other methods of administration are not available, as the risk of pneumothorax and cardiac tamponade .
During treatment with the drug, it is recommended to periodically determine the concentration of potassium in the blood serum, measure blood pressure , diuresis , perform an ECG , and monitor central venous pressure .
When endotracheally , absorption and achievement of maximum plasma concentrations of the substance may be unpredictable.
Administration of the drug in a state of shock does not replace the lost volume of circulating blood; it is still necessary to perform a blood or plasma transfusion, to administer blood replacement fluids or saline solutions to the patient.
Long-term therapy with Epinephrine is highly discouraged, as this can lead to the development of gangrene or necrosis.
Also, the medicine cannot be used to correct blood pressure during childbirth; uterine atony and bleeding may develop, and the second stage of labor may be delayed.
With long-term use, it is necessary to reduce the dose gradually; sudden discontinuation of the drug can cause a decrease in blood pressure.
The solution is easily destroyed with an alkali or an oxidizing agent .
If the solution turns brown or turns pink, or a sediment has formed at the bottom of the ampoule, it must be discarded.
pharmachologic effect
Epinephrine ampoule, 1 mg (Suprarenin)
The pharmacological actions of adrenaline are based on its physiological properties (α, β-adrenergic agonist). In medical practice, two adrenaline salts are used: hydrochloride and hydrogen tartrate. Adrenaline is used mainly as a vasoconstrictor, hypertensive, bronchodilator, hyperglycemic and antiallergic agent. Also prescribed to improve cardiac conduction in acute conditions (myocardial infarction, myocarditis, etc.)
At an injection rate of 0.04-0.1 mcg/kg/min, adrenaline causes an increase in heart rate, increases stroke volume and minute volume of blood flow, and reduces total peripheral vascular resistance (TPVR). At a dose above 0.2 mcg/kg/min, adrenaline constricts blood vessels, increases blood pressure (mainly systolic) and peripheral vascular resistance. The pressor effect can cause short-term reflex bradycardia. Relaxes the smooth muscles of the bronchi. Doses above 0.3 mcg/kg/min reduce renal blood flow, blood supply to internal organs, tone and motility of the gastrointestinal tract.
The therapeutic effect develops almost instantly with intravenous administration (duration of action - 1-2 minutes), 5-10 minutes after subcutaneous administration (maximum effect - after 20 minutes), with intramuscular administration - the onset of the effect is variable [2].
The ability to constrict blood vessels in the mucous membranes and skin and slow blood flow is used in local anesthesia to reduce the rate of absorption of anesthetics, which increases the duration of their action and reduces systemic toxic effects.
During pregnancy and lactation
There have been no adequate, well-controlled studies on which to conclude that the drug is safe to use in pregnant women.
The use of Epinephrine in early pregnancy can lead to the development of deformities, anoxia and inguinal hernia in children. The medicine should not be administered to pregnant women if blood pressure is more than 130 to 80 mm.
As a result of experiments on animals, it was revealed that when using doses 25 times higher than those recommended for humans, the medicine has a pronounced teratogenic effect .
It is best to stop breastfeeding.
Notes
| Wiktionary has an entry for " adrenaline " |
- ↑ 1 2
Epinephrine (Russian).
ReLeS.ru
(April 12, 1998). Access date: March 29, 2008. Archived August 23, 2011. - ↑ 1 2 3 4 5 6 7 8 9
Search in the drug database, search options: INN -
Epinephrine
, flags
“Search in the register of registered drugs”
,
“Search TKFS”
,
“Show lekforms”
(Russian) (inaccessible link).
Circulation of medicines
.
Federal State Institution “Scientific Center for Expertise of Medical Products” of Roszdravnadzor of the Russian Federation (March 27, 2008). — A standard clinical and pharmacological article is a by-law and is not protected by copyright in accordance with part four of the Civil Code of the Russian Federation No. 230-FZ of December 18, 2006
. Retrieved March 29, 2008. Archived September 3, 2011. - V. Dubynin.
Norepinephrine (Russian).
"PostScience"
(August 25, 2016). Date accessed: April 6, 2021. - Postganglionic fibers of the sympathetic (Russian). chem21.info/
(1980). Date accessed: April 6, 2021. - Matyushichev V.B., Shamratova V.G.
The role of adrenaline in the regulation of the electrokinetic properties of erythrocytes (Russian) // Biological Communications: scientific journal. - SPb.: Publishing house. St. Petersburg State University, 2004. - Issue. 2. - pp. 68-73. — ISSN 2587-5779. - Natalya Panasenko.
A stress hormone has been discovered that mobilizes the body better than adrenaline (Russian).
"Rossiyskaya Gazeta"
(September 15, 2019). Date accessed: April 6, 2021. - ↑ 1 2 Jeffrey K Aronson.
“Where name and image meet”—the argument for “adrenaline” // British Medical Journal. - 2000. - Vol. 320, iss. 7233. - P. 506–509. — ISSN 0959-8138. - doi:10.1136/bmj.320.7233.506. - George Oliver, E. A. Schaefer.
The Physiological Effects of Extracts of the Suprarenal Capsules (English) // The Journal of Physiology. — 1895-07-18. - Vol. 18, iss. 3. - P. 230–276. — ISSN 0022-3751. - doi:10.1113/jphysiol.1895.sp000564. - Poznań Supercomputing and Networking Center-dL Team.
FBC (Polish). FBC. Access date: January 13, 2021. - Epinephrin from the Suprarenal Capsule: “A Classic of Science” // The Science News-Letter. — 1932-12-17. - Vol. 22, iss. 610. - P. 391. - ISSN 0096-4018. - doi:10.2307/3908203.
- Organic chemistry (English) // Journal of the Chemical Society, Abstracts. - 1900. - Vol. 78. - P. A73. — ISSN 0590-9791. - doi:10.1039/ca9007800073.
- Jōkichi Takamine.
The Blood Pressure Raising Principle Of The Suprarenal Gland (English) // JAMA: The Journal of the American Medical Association. - 1902-01-18. - Vol. XXXVIII, iss. 3. - P. 153. - ISSN 0098-7484. - doi:10.1001/jama.1902.62480030011001c. - E. M. Tansey.
What's in a name? Henry Dale and adrenaline, 1906. (English) // Medical History. — 1995-10. - Vol. 39, iss. 4. - P. 459–476. — ISSN 0025-7273. - doi:10.1017/s0025727300060373. - Ruksin, “Guide to the provision of emergency and emergency medical care”
- Struchkov, “General Surgery”
- M. D. Mashkovsky, “Medicines, vol. 1.”
Drugs containing (Epinephrine analogues)
Level 4 ATC code matches:
Norepinephrine
Mezaton
Dobutamine
Dopamine
Dopamine
Adrenalin
Analogs of Epinephrine: Adrenaline, Epinephrine hydrotartrate, Adrenaline hydrotartrate solution 0.18% for injection, Adrenaline-Hydrochloride-Vial, Adrenaline tartrate .
Articaine and Epinephrine are included in the following drugs: Alfacaine SP, Articaine INIBSA, Artifrin, Primacaine with adrenaline, Ubistezin, Ultracaine D-S, Brilocaine-adrenaline, Cytokartin, Articaine DF, Articaine Perrel with adrenaline, Septanest with adrenaline .
Similar drugs
The most common analogues of Epinephrine are Vial and Adrenaline. They contain similar active ingredients.
Thus, Epinephrine is an indispensable drug for people with diseases of the visual system, namely open-angle glaucoma. Particular attention should be paid to contraindications for use and side effects of the drug.
Before you start taking it, you should definitely consult with your doctor, who will decide whether to take the medicine and determine the required dosage.
For interesting information about modern methods of treating glaucoma, watch the video: