Pharmacological action of Erythromycin
Erythromycin and Erythromycin analogues disrupt the process of formation of bonds between amino acid molecules, blocking the synthesis of bacterial proteins (do not affect the process of formation of nucleic acids). The use of Erythromycin in high doses promotes the manifestation of its bactericidal effect.
According to the instructions, treatment with Erythromycin or Erythromycin analogs is prescribed for diseases caused by gram-negative (Haemophilus influenzae, Neisseria gonorrhoeae, Brucella spp., Bordetella pertussis, Legionella spp.) or gram-positive bacteria (Streptococcus spp., Staphylococcus spp., synthesizing and not synthesizing penicillinase, alpha- hemolytic streptococcus from the Viridans group, Corynebacterium minutissimum, Corynebacterium diphtheriae, Bacillus anthracis), as well as Listeria monocytogenes, Treponema spp., Chlamydia spp., Entamoeba histolytica, Rickettsia spp.
Gram-negative bacilli Pseudomonas aeruginosa, Escherichia coli, as well as Salmonella spp., Shigella spp. are resistant to Erythromycin.
Microorganisms whose growth slows down at a drug concentration of less than 0.005 g/l are considered sensitive to Erythromycin, moderately sensitive - from 0.001 to 0.006 g/l, moderately resistant and resistant - from 0.006 to 0.008 g/l.
Erythromycin is distributed unevenly in the body. Most of it accumulates in the kidneys, spleen, and liver. The drug penetrates well into synovial and ascitic fluids, the pleural cavity, lung tissue, and sperm. The concentration in the cerebrospinal fluid is 10% of the antibiotic content in plasma.
The main part of Erythromycin is metabolized in the liver (about 90%). 20-30% of the antibiotic is excreted with bile, 2-5% of Erythromycin is excreted unchanged by the kidneys (half-life - 1.5-2 hours).
Chemical properties[edit | edit code]
Macrolides get their name from the macrocyclic lactone ring (14-membered in erythromycin and clarithromycin and 15-membered in azithromycin), to which at least one deoxysugar residue is connected. Clarithromycin differs from erythromycin in the methyl group that replaces the hydrogen of the hydroxyl group at position 6, and azithromycin has an additional nitrogen atom with a methyl group attached to its lactone ring. Due to these structural differences, azithromycin and clarithromycin are more stable in an acidic environment, penetrate tissue better and have a wider spectrum of action. The chemical formulas of macrolides are as follows:
Structural formula of erythromycin Structural formulas of clarithromycin and azithromycin
Indications for use of Erythromycin
According to the instructions, treatment with Erythromycin is indicated for various infectious and inflammatory processes, including respiratory tract infections, diphtheria, prostatitis, scarlet fever, amoebic dysentery, listeriosis, syphilis, cholecystitis, gonorrhea. Erythromycin is used in the treatment of infections of soft tissues and skin - trophic ulcers, second and third degree burns, furunculosis, infected wounds, pustular skin diseases. In addition, the antibiotic is used for various infections of the mucous membrane of the eyes (including conjunctivitis in newborns), and for genitourinary infections in pregnant women caused by Chlamydia trachomatis.
Reviews of Erythromycin indicate that this antibiotic is often used to prevent infectious complications during various diagnostic and therapeutic procedures.
Side effects[edit | edit code]
Erythromycin rarely causes severe side effects. Allergic reactions include fever, eosinophilia, and rash, which may occur alone or in combination. After discontinuation of the drug, the symptoms quickly disappear. The most severe side effect is cholestatic hepatitis. It is mainly caused by erythromycin estolate, very rarely by erythromycin ethylsuccinate or erythromycin stearate (Ginsburg and Eichenwald, 1976). The disease begins approximately 10-20 days after the start of treatment with nausea, vomiting and cramping abdominal pain. The pain is often the same as with | acute cholecystitis, which may lead to unnecessary surgery. Jaundice soon appears, sometimes accompanied by fever, leukocytosis, eosinophilia and increased aminotransferase activity. Liver biopsy reveals cholestasis, periportal infiltration of neutrophils, lymphocytes and eosinophils, and sometimes necrosis of hepatocytes. Manifestations of hepatitis rarely persist for more than a few days after discontinuation of the drug. It is possible that cholestatic hepatitis results from an allergic reaction to erythromycin estolate (Tolman et al., 1974). There may be a slight increase in serum liver enzyme activity (McCormack et al., 1977).
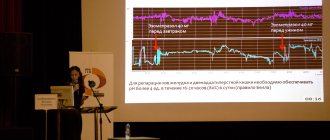
When taken orally, especially in large doses, erythromycin often causes epigastric pain, sometimes quite severe. With intravenous administration, gastrointestinal disorders are also possible - cramping abdominal pain, nausea, vomiting, diarrhea. Erythromycin has been shown to enhance gastrointestinal motility by binding to motilin receptors (Smith et al., 2000). Gastrointestinal disturbances are dose-dependent and are more common in children and young adults (Seifert et al., 1989). Longer infusion (over 1 hour) and pre-administration of glycopyrronium bromide alleviate these symptoms (Bowler et al., 1992). IV administration of the drug at a dose of 1 g, even when diluted in a large volume of liquid, is often accompanied by thrombophlebitis. Slow administration reduces the risk of this complication.
There are reports that erythromycin causes cardiac arrhythmias, including prolongation of the QT interval and, against its background, ventricular tachycardia. In most cases, these disorders occurred in patients with heart disease or were observed when erythromycin was prescribed concomitantly with drugs such as cisapride and terfenadine (Brandriss et al., 1994).
The use of erythromycin in large doses (erythromycin glucoheptonate or erythromycin lactobionate, 4 g/day IV, or large doses of erythromycin estolate orally) may be accompanied by transient hearing loss (Karmody and Weinstein, 1977).
Instructions for use
According to the instructions, Erythromycin tablets should be taken orally (do not chew). The daily dose of the drug for adults and adolescents (over 14 years old) is 1-2 g, a single dose is 0.25-0.50 g. If necessary, the daily dose is increased to 4 g. The interval between doses is six hours.
Children from four months to 18 years, depending on body weight, age and severity of the disease, are prescribed 0.03-0.05 g/kg per day in two to four doses, children in the first three months of life - 0.2-0. 4 g/kg Erythromycin per day. If necessary, the daily dose is doubled.
When treating diphtheria with Erythromycin, take 0.25 g of the drug twice a day.
The therapeutic dose for primary syphilis is 30-40 g of antibiotic for the entire course of treatment. The course of treatment is one to two weeks.
For amoebic dysentery, adults are prescribed 0.25 g of the drug four times a day, children - 0.03-0.05 g/kg of Erythromycin per day. Course duration is 10-15 days.
For legionellosis, take 0.5-1 medication four times a day for two weeks.
For gonorrhea - 0.5 g of the drug every six hours for three days, then 0.25 g every six hours for a week.
To prevent infectious complications, 1 g of antibiotic is prescribed 19 hours, 18 hours and 9 hours before the start of surgery.
For whooping cough, take 0.04-0.05 g/kg of antibiotic per day for one to two weeks. For pneumonia in children - 0.05 g/kg of antibiotic per day (in four doses). The duration of the course is at least three weeks.
For genitourinary infections during pregnancy - 0.5 g of medication four times a day for a week.
Erythromycin in the form of an ointment is applied to the affected area, and for eye diseases it is placed behind the lower eyelid. The frequency, dose and duration of use of Erythromycin in the form of ointment are determined individually.
Antimicrobial activity[edit | edit code]
Erythromycin usually has a bacteriostatic effect, but in high concentrations it can act bactericidal on highly sensitive microorganisms. In vitro, erythromycin is most active against aerobic gram-positive cocci and rods (Steigbiegel, 2000). The MIC for sensitive strains of Streptococcus pyogenes and Streptococcus pneumoniae ranges from 0.015 to 1 μg/ml. However, the number of erythromycin-resistant streptococcal strains is increasing. The mechanism of resistance is the same for all macrolides, therefore such strains are cross-resistant to other drugs in this group. Due to the widespread use of macrolides, the proportion of Streptococcus pyogenes strains resistant to them can reach 40% (Seppala et al., 1997; Esposito et al., 1998). In Streptococcus pneumoniae, the prevalence of macrolide resistance is particularly high among penicillin-resistant strains, being 60% compared with 5% among penicillin-susceptible strains (Thomsberry et al., 1997; Thomsberry et al., 1999). The MIC of erythromycin for viridans streptococci is 0.06–3.1 μg/ml.
Some staphylococci are sensitive to erythromycin, but the MIC for them varies widely (for Staphylococcus epidermidis - from 8 to more than 32 μg/ml, for Staphylococcus aureus - from 0.12 to more than 128 μg/ml). Hospital strains of Staphylococcus aureus are often resistant to macrolides; in addition, Staphylococcus aureus may become resistant during treatment. Macrolide-resistant strains of Staphylococcus aureus exhibit cross-resistance to clindamycin (Fass, 1993). Many gram-positive bacilli are sensitive to erythromycin: the MIC for Clostridium perfringens is 1 μg/ml, for Corynebacterium diphtheriae - 0.2-3 μg/ml, for Listeria monocytogenes - 0.25-4 μg/ml.
Erythromycin has no effect on most enterobacteria, but is active against other gram-negative microorganisms. In vitro, it is moderately active against Haemophilus influenzae (MIC 1-32 μg/ml) and Neisseria meningitidis (MIC 0.4-1.6 μg/ml), highly active against most strains of Neisseria gonorrhoeae (MIC 0.12-2 μg/ml). ml; Steigbigel, 2000). In addition, it acts on Pasteurella mul-tocida, Borrelia spp. and Bordetella pertussis. Strains of Bacteroides fragilis are often resistant to erythromycin (MIC 2–32 μg/ml), and Campylobacter jejuni are sensitive (MIC 0.5–4 μg/ml). Erythromycin is effective against infections caused by Mycoplasma pneumoniae (MIC 0.004–0.02 μg/ml) and Legionella pneumophila (MIC 0.01–2 μg/ml). For most strains of Chlamydia trachomatis, the MIC is 0.06–2 μg/ml. In vitro, some atypical mycobacteria, including Mycobacterium scrofulaceum, are also sensitive to erythromycin. The susceptibility of Mycobacterium kansasii and Mycobacterium avium-intracellulare varies (Molavi and Weinstein, 1971). Mycobacterium fortuitum is resistant to erythromycin.
Clarithromycin is slightly more active than erythromycin against strains of streptococci and staphylococci that are sensitive to the latter, and is moderately active against Haemophilus influenzae and Neisseria gonorrhoeae. In addition, clarithromycin has a good effect on Moraxella catarrhalis, Chlamydia spp., Legionella pneumophila, Borrelia burgdorferi, Mycoplasma pneumoniae, Mycobacterium leprae (Chan et al., 1994).
Azithromycin is generally less active than erythromycin against gram-positive bacteria (streptococci, enterococci), but slightly stronger than erythromycin and clarithromycin against Haemophilus influenzae and Campylobacter spp. (Peters et al., 1992). Azithromycin is highly active against Moraxella catarrhalis, Pasteurella multocida. Chlamydia spp., Mycoplasma pneumoniae. Legionella pneumophila, Borrelia burgdorferi, Fusobacterium spp. and Neisseria gonorrhoeae.
A microorganism is considered sensitive to new macrolides (clarithromycin and azithromycin) if its MIC does not exceed 2 μg/ml. An exception is Haemophilus influenzae: the MIC for strains sensitive to clarithromycin does not exceed 8 μg/ml, and the MIC for strains sensitive to azithromycin is 4 μg/ml.
Azithromycin and clarithromycin are more active than erythromycin against Mycobacterium avium-intracellulare. New macrolides also act on some protozoa (Toxoplasma gondii, Cryptosporidium spp., Plasmodium spp.).
Drug interactions of Erythromycin
The antibiotic reduces the bactericidal effect of beta-lactam antimicrobial drugs - cephalosporins, penicillins, carbopenems.
Erythromycin enhances the nephrotoxicity of cyclosporine and the pharmacological effect of benzodiazepines.
The simultaneous use of Erythromycin and terfenadine or astemizole contributes to the possible development of arrhythmia.
Simultaneous administration of the drug and dihydroergotamine or non-hydrogenated ergot alkaloids leads to spasmodic vasoconstriction.
Mechanism of action[edit | edit code]
Macrolides are bacteriostatic antibiotics that inhibit protein synthesis by reversibly binding to the 505 ribosomal subunit (Fig. 47.3; Brisson-Noel et al., 1988). Macrolides act on the same target as chloramphenicol, competitively inhibiting its binding to ribosomes (Fig. 47.2). A change in the 50S ribosomal subunit due to mutation, which disrupts the binding of macrolides to the target, leads to the development of drug resistance. Unlike chloramphenicol, which prevents the formation of a peptide bond, macrolides act at the stage of translocation - the transfer of a newly synthesized peptidyl-tRNA molecule from the aminoacyl site of the ribosome to the peptidyl site.
Gram-positive bacteria accumulate almost 100 times more erythromycin than gram-negative bacteria.
In an alkaline environment, the antimicrobial activity of the drug is much higher, probably because in its non-ionized form, which predominates at high pH, it penetrates bacterial cells much better (Sabath et al., 1968; Vogel et al., 1971).
Acquired resistance to macrolides is due to three main mechanisms:
- active removal of the drug from the cell (in staphylococci the transporter is encoded by the mrsA gene, in Streptococcus pyogenes - by the mefA gene, in Streptococcus pneumoniae - by the mefE gene),
- a decrease in the affinity of ribosomes for the drug, due to their methylation under the influence of the inducible or constitutive enzyme methyltransferase (this enzyme is encoded by the egtA, egtB and egtC genes)
- hydrolysis of macrolides by enterobacterial esterases (Barth61dmy et al., 1984).
The second mechanism, mediated by the egt genes, determines resistance not only to macrolides, but also to lincosamides and streptogramins (MLSB phenotype). All of these drugs act on the same target, the methylation of which leads to the formation of resistance. There is another mechanism of macrolide resistance found in Bacillus subtilis, Campylobacter spp. and gram-positive cocci. It is caused by chromosomal mutations that change the structure of the protein 508-ribosomal subunit.
Read also[edit | edit code]
- Antibiotics (antimicrobial agents) Choice of antibiotic
- Combination antibiotic therapy
- Prophylactic antibiotic therapy
- Mechanisms of action of antibiotics
- Sulfonamides, trimethoprim/sulfamethoxazole
- Quinolones and urinary antiseptics
- Beta-lactam antibiotics Penicillins
- Cephalosporins
- Carbapenems
- Beta-lactamase inhibitors
- Tetracyclines
- Antituberculosis drugs (antimycobacterial) Isoniazid
- Rifampicin
- Ethambutol
- Streptomycin
- Pyrazinamide
- Other anti-tuberculosis drugs
Drug interactions[edit | edit code]
Erythromycin and clarithromycin interact with other drugs (Periti et al., 1992). Erythromycin enhances the effects of astemizole, carbamazepine, glucocorticoids, cyclosporine, digoxin, ergot alkaloids, terfenadine, theophylline, triazolam, valproic acid and warfarin, probably by inhibiting liver microsomal enzymes involved in the metabolism of these drugs (Ludden, 1985; Martell et al. , 1986; Honig et al., 1992). Clarithromycin, which is similar in structure to erythromycin, interacts with the same drugs. Azithromycin, apparently, does not enter into drug interactions, since, unlike erythromycin and clarithromycin, it contains a 15-membered lactone ring. However, azithromycin should be prescribed concomitantly with the drugs listed above with caution.