The drug Glibenclamide is a drug belonging to the group of glycemic agents that have a stimulating effect on the pancreas. The product activates the process of insulin production. The drug is indicated for patients suffering from type 2 diabetes mellitus in cases where diet therapy and physical activity do not stabilize the condition.
Pharmacological group
The drug belongs to the group of oral hypoglycemic compounds, sulfonylurea derivatives of the 2nd generation. The drug activates the secretion of insulin by pancreatic cells and increases the intensity of insulin release. The drug acts primarily during the second stage of the insulin production process. The drug increases the sensitivity of peripheral tissues to insulin and the degree of its binding to target cells.
The drug has a hypolipidemic effect and reduces the properties of the blood. After oral administration, the active substance is quickly and completely absorbed from the gastrointestinal tract. Binding to blood proteins is more than 95%. The substance is metabolized in the liver with the formation of inactive metabolites. The drug is excreted from the body in the form of metabolites in urine and bile. The half-life is approximately 10 hours.
Side effect
From the metabolic side there may be:
hypoglycemia, often nocturnal, accompanied by:
- headache,
- hunger
- nausea,
- sleep disturbance,
- nightmares,
- anxiety,
- trembling,
- secretion of cold sticky sweat,
- tachycardia,
- confused consciousness
- feeling tired
- speech and vision disorders,
Sometimes there may be seizures and coma, as well as:
- increased sensitivity to alcohol;
- increased body weight;
- dyslipidemia, accumulation of adipose tissue;
- with long-term use, it is possible to develop hypofunction of the thyroid gland.
From the digestive system:
- nausea, vomiting;
- heaviness, discomfort and feeling of pain in the abdomen;
- flatulence, heartburn, diarrhea;
- increased or decreased appetite;
- in rare cases, liver function may be disrupted, hepatitis, cholestatic jaundice, and porphyria may develop.
From the hematopoietic system:
- very rarely there may be aplastic or hemolytic anemia;
- lecopenia;
- agranulocytosis;
- pancytopenia;
- eosinophilia;
- thrombocytopenia.
Allergic reactions:
- rarely develop erythema multiforme, photosensitivity or exfoliative dermatitis;
- cross-allergy to thiazide-like drugs, sulfonamides or sulfonylurea derivatives may occur.
Other side effects:
- hypoosmolarity;
- hyponatremia;
Inadequate release of antidiuretic hormone, accompanied by:
- dizziness,
- swelling of the face,
- hands and ankles,
- depression,
- lethargy,
- convulsions,
- stupor,
- whom,
- accommodation disorder (transient).
If any undesirable reactions or unusual phenomena appear, you should definitely consult with your doctor regarding further treatment with this drug; in the meantime, Glibenclamide will have to be postponed.
Indications for use
The list of indications for use of the composition includes type 2 diabetes mellitus when high compensation is not achieved in the process of diet therapy and physical activity.
for adults
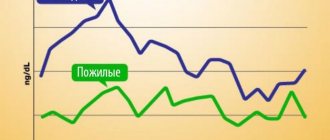
The drug is indicated for patients of this age category. The product can be used by elderly people who have no contraindications for use. It should be remembered that patients with impaired liver and kidney function, as well as elderly people, require adjustment of sane doses.
for children
The drug is not used in pediatric practice. Children under 18 years of age are a contraindication to the use of the medicinal composition.
for pregnant women and during lactation
The drug is not recommended for use during pregnancy and lactation due to the lack of reliable data on the effect of the drug on the body of a pregnant woman and the process of fetal development. If it is necessary to use the composition during breastfeeding, natural feeding should be stopped and the child subsequently transferred to artificial nutrition.
special instructions
It is necessary to regularly monitor the blood glucose level on an empty stomach and after meals, the daily curve of glucose levels in the blood and urine.
In case of surgical interventions or in case of decompensation of diabetes, the possibility of using insulin preparations must be considered.
Patients should be warned about the increased risk of hypoglycemia when taking ethanol (including the possible development of disulfiram-like reactions: abdominal pain, nausea, vomiting, headache), NSAIDs, and during fasting.
During treatment, it is not recommended to stay in the sun for a long time.
Dose adjustment is necessary in case of physical and emotional stress, or changes in diet.
Clinical manifestations of hypoglycemia can be masked when taking beta-blockers, clonidine, reserpine, guanethidine.
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Applications and dosages
It is recommended to determine the dose of the drug on an individual basis. When determining the maximum effective dose, it is recommended to take into account the severity of diabetes, the level of glycemia on an empty stomach and 2 hours after eating.
for adults
The average dose is 2.5-15 mg per day. The frequency of administration varies from 1 to 3 times. The drug is taken some time before meals. A dose of more than 15 mg is used in rare cases, because it can provoke an increase in the pronounced hypoglycemic effect. For elderly patients, the initial dose is 1 milligram per day. When transitioning, the initial dose is 2.5 milligrams. If there is no compensation within 4-6 weeks, combination therapy should be planned.
for children
The drug is not used in pediatric practice due to the lack of accurate information about the effect of the drug on the child’s body.
for pregnant women and during lactation
Taking the drug is contraindicated during pregnancy and breastfeeding due to the lack of accurate data on the effect of the composition on the course of pregnancy and the process of fetal development.
Overdose
A single overdose or the use of slightly increased doses for a long time can lead to severe prolonged hypoglycemia, which is life-threatening.
Symptoms of overdose (hypoglycemia): sudden sweating, increased heart rate, trembling, feeling of hunger, anxiety, paresthesia in the mouth, pale skin, headache, drowsiness, sleep disorders, fearfulness, uncertainty in movements, temporary neurological disorders (speech and vision disorders , the appearance of paralysis or sensory impairment). With progressive hypoglycemia, the patient may lose control over his condition and lose consciousness (hypoglycemic shock). In such cases, the skin feels moist and cold to the touch, tachycardia, hyperthermia, motor agitation, hyperreflexia, paresis and a positive Babinski reflex occur, and convulsions may occur.
Treatment. The patient can eliminate mild or moderate hypoglycemia on his own by consuming sugar, food or drinks with a high sugar content. If hypoglycemia is severe, you should immediately seek help from a doctor. In case of accidental poisoning and provided that contact can be established with the patient, vomiting should be induced and (in the absence of a tendency to convulsions) intravenous administration of glucose should be administered. If the patient loses consciousness, intravenous glucose should be immediately started (40-80 ml of a 40% solution in the form of an injection, followed by an infusion of 5-10% glucose solution). If necessary, you can additionally administer 1 mg of glucagon intravenously or intramuscularly. If the patient does not regain consciousness, these measures are repeated, and in the future intensive therapy may be necessary. In case of prolonged hypoglycemia, the patient must be monitored for several days with regular monitoring of blood sugar levels and, if necessary, infusion therapy.
Analogs
The drug has a sufficient number of analogues for use, but you can change the medicinal composition prescribed by your doctor after a preliminary consultation.
Formetin
The drug Formetin belongs to the group of hypoglycemic agents. The composition is used for the treatment of insulin-dependent diabetes mellitus. Formetine should not be used by children or pregnant women. During treatment, you should stop breastfeeding.
Maninil
The drug Maninil belongs to the group of hypoglycemic drugs that are sulfonylurea derivatives. The drug is used to treat type 2 diabetes mellitus in adult patients. The drug is prohibited for use by children, pregnant women and nursing mothers.
Siofor
Siofor is a popular medicine used for diabetes. The drug is used as a means to combat excess body weight. Patients should be aware that using the drug for purposes other than treating diabetes can cause significant harm to health.
Side effects
When assessing adverse reactions, the following frequencies of occurrence were taken as a basis: very often (≥ 10%), often (< 10%, ≥ 1%), sometimes (< 1%, ≥0.1%), rarely (< 0.1 %, ≥ 0.01%), very rare (< 0.01% or cases unknown).
Metabolic and nutritional disorders: often – hypoglycemia, weight gain.
Visual disturbances: very rarely - visual and accommodation disturbances, especially at the beginning of treatment.
Disorders of the digestive tract: sometimes - nausea, feeling of fullness in the stomach, vomiting, abdominal pain, diarrhea, belching, metallic taste in the mouth. These complaints are reversible and do not require discontinuation of the drug.
Liver and gallbladder dysfunction: very rarely - transient increase in AST and ALT, alkaline phosphatase, drug-induced hepatitis, intrahepatic cholestasis, which may be caused by an allergic reaction of a hyperergic type of liver cells. These disorders are reversible after discontinuation of the drug, but can lead to liver failure, which is life-threatening.
Skin and subcutaneous tissue disorders: sometimes – itching, urticarial rash, erythema nodosum, morbilliform or maculopapular exanthema, purpura, photosensitivity. These phenomena of hypersensitivity reactions are reversible, but very rarely can develop into a life-threatening condition, which is accompanied by suffocation and a decrease in blood pressure, up to the development of shock. Very rarely - generalized hypersensitivity reactions, which are accompanied by skin rash, arthralgia, fever, proteinuria and jaundice; allergic vasculitis, which is life-threatening. If skin reactions occur, consult a doctor.
Disorders of the blood and lymphatic system: rarely - thrombocytopenia. Very rarely - leukopenia, erythropenia, granulocytopenia up to the development of agranulocytosis. In some cases - pancytopenia, hemolytic anemia, aplastic anemia, eosinophilia. The above changes in the blood picture are reversible after discontinuation of the drug, but very rarely can be life-threatening.
Other side effects: very rarely - weak diuretic effect, syndrome of inappropriate secretion of antidiuretic hormone, reversible proteinuria, disulfiram-like reaction, cross-allergy with sulfonamides, sulfonamide derivatives and probenecid. Ponceau 4R may cause allergic reactions.
Price in pharmacies
Maninil, containing micronized glibenclamide, costs 130-160 rubles. per package of 120 tablets. Maninil 5 mg will be cheaper, the price of a pack is about 120 rubles. The cost of domestic analogues is even lower: from 26 rubles. for 50 tablets or 92 rubles. for 120 tablets. Thus, even with the maximum dosage, the price of treatment does not exceed 100 rubles. per month.
The drug Glibenclamide can be obtained free of charge in any region of Russia if the patient has confirmed diabetes mellitus and is registered with an endocrinologist.
Glibenclamide - reviews
On thematic forums, diabetics and doctors most often discuss the effectiveness of various drug treatment regimens. Those who are prescribed the drug as monotherapy complain of incomplete compensation of sugars. With complex treatment, some note excessive activity of Glibenclamide.
Doctors emphasize that choosing the optimal dosage for Glibenclamide, which will allow you to maintain normal well-being for a long time, requires an individual approach, requires time and constant monitoring of glucometer readings for different conditions of the patient. In such cases, correspondence counseling can be not only ineffective, but also dangerous.
The information about the medication on the site is for reference and generalization purposes, collected from available sources and is not a basis for diagnosis or self-medication. It will not replace consultation with an endocrinologist.
general characteristics
The name of the drug Glibenclamide in international format in Latin is Glibenclamide.
Externally, the medication is a light pink disk-shaped tablet with a dividing line. The coating may have a marble structure with minor inclusions. The tablets are packaged in blisters of 10 pieces. One box can contain up to 12 such plates.
Glibenclamide is dispensed with a prescription and stored under normal conditions, out of reach of children. The instructions state the shelf life of the drug is 5 years. Expired medicine should not be taken.
Each tablet contains 5 mg of glibenclamide and fillers in the form of lactose monohydrate, potato starch, magnesium stearate, polyvinylpyrrolidone, E 124.
Domestic pharmaceutical companies produce sugar-lowering agents:
- Antiviral;
- Akrikhin KhFK;
- Bivitekh;
- ALSI Pharma;
- Biosynthesis.
It is also produced by the Ukrainian company Health. The price for Glibenclamide in the Russian pharmacy chain is 270-350 rubles.
Interaction
ACE inhibitors (captopril, enalapril), H2-histamine receptor blockers (cimetidine), antifungal drugs (miconazole, fluconazole), NSAIDs (phenylbutazone, azapropazone, oxyphenbutazone), fibrates (clofibrate, bezafibrate), antituberculosis (ethionamide), salicylates, coumarin anticoagulants series, anabolic steroids, beta-blockers, MAO inhibitors, long-acting sulfonamides, cyclophosphamides, biguanides, chloramphenicol, fenfluramine, acarbose, fluoxetine, guanethidine, pentoxifylline, tetracycline, theophylline, tubular secretion blockers, reserpine, bromocriptine, disopyramide, pyridoxine, insulin, allopurinol enhances the effect.
The effect is weakened by barbiturates, corticosteroids, adrenostimulants (epinephrine, clonidine), antiepileptic drugs (phenytoin), BMCC, carbonic anhydrase inhibitors (acetazolamide), thiazide diuretics, chlorthalidone, furosemide, triamterene, asparaginase, baclofen, danazol, diazoxide, isoniazid, morphine, ritodrine, salbutamol, terbutaline, glucagon, rifampicin, thyroid hormones, Li+ salts, in high doses - nicotinic acid, chlorpromazine, oral contraceptives and estrogens.
Drugs that acidify urine (ammonium chloride, CaCl2, ascorbic acid in large doses) enhance the effect by reducing the degree of dissociation and increasing the reabsorption of glibenclamide.
Drugs that inhibit bone marrow hematopoiesis increase the risk of myelosuppression.
Contraindications
Glibenclamide is not recommended for use if:
- Hypersensitivity to the main component or additional substances
- Excessive sensitivity to sulfonamides, probenecid, sulfinamide diuretics, as well as sulfonylureas
- Diabetes mellitus, when treatment with insulin is required (insulin-dependent diabetes mellitus, metabolism with a tendency toward acidosis, postoperative condition after previous pancreatectomy, precoma or diabetic coma, secondary failure of treatment with glibenclamide in type 2 diabetes)
- Serious disorders of the liver and renal system
- Pregnancy, GW.