Release form and composition
The drug is available in the form of a solution for subcutaneous (s/c) administration: a clear, colorless or almost colorless liquid (3 ml in colorless glass cartridges (type I), which are mounted in SoloStar disposable syringe pens with a gray body and a purple button for administration of the drug, in a cardboard box with a cardboard retainer, 5 syringe pens and instructions for use of Lantus SoloStar).
1 ml of solution contains:
- active ingredient: insulin glargine – 100 units (unit of action) or 3.637 8 mg;
- auxiliary components: metacresol (m-cresol), glycerol 85%, zinc (in the form of zinc chloride), hydrochloric acid, sodium hydroxide, water for injection.
Terms and conditions of storage
Store at a temperature of 2-8 ° C (without freezing) out of the reach of children, dry and protected from light. Cartridges, pre-filled OptiSet syringe pens, OptiClick cartridge systems should be stored in their own cardboard packaging at temperatures up to 25 ° C, protected from light and out of the reach of children. Pre-filled OptiSet syringe pens cannot be refrigerated.
Best before date:
- Solution – 3 years;
- Cartridges, pre-filled OptiSet pens and OptiClick cartridge systems after first use – 28 days.
Pharmacological properties
Pharmacodynamics
Lantus SoloStar is a hypoglycemic agent. The active ingredient of the drug, insulin glargine, is an analogue of human insulin. It is obtained by the method of DNA recombination (deoxyribonucleic acid) of bacteria of the species Escherichia coli (strains K12); it is characterized by low solubility in a neutral environment.
The complete solubility of insulin glargine in Lantus SoloStar is due to the acidic reaction of the injection solution, which is neutralized after injection into the subcutaneous fat. This promotes the formation of microprecipitates, which ensure a prolonged effect of the drug as a result of the constant smooth release of small portions of insulin glargine and the preservation of the concentration-time curve profile.
As a result of biotransformation, two active metabolites are formed - M1 and M2. Insulin glargine and its active metabolites have a mechanism of binding to specific insulin receptors that is very similar to human insulin, so insulin glargine may have biological effects similar to those of endogenous insulin.
In the body, the main role of insulin and its analogues, including insulin glargine, is to regulate glucose metabolism. It reduces blood glucose concentrations by stimulating peripheral tissues (especially skeletal muscle and adipose tissue) to absorb glucose and inhibiting the production of glucose in the liver. Insulin suppresses lipolysis in fat cells (adipocytes), inhibits proteolysis and increases protein synthesis.
The reduced absorption rate of insulin glargine creates conditions for the prolonged action of Lantus SoloStar and allows it to be used once a day. After administration, the effect begins to appear, on average, after 1 hour and lasts for 24 hours, the maximum duration is 29 hours. The period of action of insulin glargine can vary significantly.
The use of Lantus SoloStar insulin in syringe pens is indicated for the treatment of type 1 diabetes mellitus in children over 2 years of age. Its effectiveness in the age group of 2–6 years is confirmed by a significant reduction in the incidence of hypoglycemia with clinical manifestations both during the day and at night.
A five-year observation of patients with type 2 diabetes mellitus taking Lantus SoloStar did not reveal significant differences in the progression of diabetic retinopathy compared with insulin isophane.
The affinity of insulin glargine for the insulin-like growth factor 1 (IGF-1) receptor is approximately 8 times higher than that of human insulin, but slightly less for the metabolites M1 and M2.
In type 1 diabetes mellitus, the level of total therapeutic concentration of insulin glargine and its metabolites is noticeably lower than the level required for half-maximal binding to IGF-1 receptors and triggering subsequent activation of the mitogenic-proliferative pathway through them. Physiological concentrations of endogenous IGF-1 can activate the mitogenic-proliferative pathway. However, the therapeutic concentrations of insulin achieved during treatment with Lantus SoloStar are significantly lower than the pharmacological concentrations necessary to activate the mitogenic-proliferative pathway.
The international, multicenter, randomized trial included 12,537 patients with impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or early stage type 2 diabetes mellitus and a high risk of cardiovascular disease. Study participants were divided into two equal groups, one of which took insulin glargine, its dose was titrated to achieve a fasting blood glucose (FBG) concentration of 5.3 mmol or less. The second group of patients received standard therapy.
The primary endpoint of the study was the time to cardiovascular death, first nonfatal stroke, or nonfatal myocardial infarction. It was found that the use of insulin glargine does not change the risk of cardiovascular events or cardiovascular mortality compared with standard hypoglycemic therapy.
The secondary endpoint was the time to the first occurrence of any complication of nonfatal myocardial infarction or nonfatal stroke, the time to coronary, peripheral, or carotid revascularization procedures, or to hospitalization for heart failure. There were no differences in any of the endpoints, the composite microvascular outcome measure, or all-cause mortality.
The median values of glycated hemoglobin (HbA1c), which was 6.4% at the beginning of treatment, ranged from 5.9% to 6.4% throughout the observation period in the insulin glargine group, and from 6.2% in the standard treatment group. up to 6.6%.
The study results showed that with the use of insulin glargine, the development of severe hypoglycemia per 100 patient-years of treatment was 1.05 episodes, and with standard hypoglycemic therapy - 0.3 episodes. Observation of patients receiving insulin glargine for 6 years did not reveal any cases of hypoglycemia in 42% of patients.
The median change in body weight at the last treatment visit was 2.2 kg higher compared to outcome in the insulin glargine group than in the standard therapy group.
Pharmacokinetics
After subcutaneous administration, the absorption of insulin glargine compared to insulin isophane occurs more slowly and over a longer period of time, and also does not reach peak concentrations. The equilibrium concentration of Lantus SoloStar in blood plasma after a single daily administration is achieved after 2–4 days. Serum insulin concentrations are comparable when injected into the abdomen, upper arm, or thigh.
Insulin glargine is characterized by less variability in its pharmacokinetic profile both within the same and between patients.
In the subcutaneous fat, partial cleavage of insulin glargine occurs from the carboxyl end of the beta chain with the formation of two active metabolites: M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin). The M1 metabolite predominantly circulates in the blood plasma; with increasing doses of the drug, its systemic exposure increases. The effect of the drug is mainly due to systemic exposure to the M1 metabolite. In the systemic circulation, insulin glargine and the M2 metabolite are practically not detected, or their concentrations do not depend on the administered dose of Lantus SoloStar.
The T½ (half-life) of insulin glargine is comparable to the T½ of human insulin.
Patient age, gender, or smoking do not differ in the safety and effectiveness of Lantus SoloStar.
Obesity of patients does not affect the safety and effectiveness of insulin glargine.
It has been established that the use of Lantus SoloStar in children aged 2–6 years with type 1 diabetes mellitus does not cause the accumulation of insulin glargine and its metabolites in the blood plasma.
Reviews
Lantus is probably the most popular long-acting insulin among diabetics and has been for many years. Its main competitor Levemir has fewer fans. The new advanced insulin Tresiba has only recently become available. It is sold at a high price and therefore fails to capture a large market share despite its improved properties. Over many years of use, many reviews have accumulated about the drug Lantus. They are written mainly by patients, and sometimes by doctors.
Negative reviews of Lantus insulin are left by patients who do not follow a low-carbohydrate diet and/or take the drug once a day. Simplified insulin therapy regimens inevitably cause spikes in blood sugar, as well as attacks of hypoglycemia.
Lantus injections once a day are a dead end. It guarantees the diabetic poor health, poor test results for glycated hemoglobin, and the gradual development of chronic complications. The worst results are for those who try to replace the administration of rapid insulin before meals with injections of large doses of a long-acting drug.
Insulin Lantus: review from a patient with type 2 diabetes
Switching to a low-carbohydrate diet allows you to reduce insulin dosages by 2-8 times. Doses of both long-acting and fast-acting drugs are reduced. The lower the insulin dose, the more stable its effect and the lower the risk of allergic reactions. You can control type 2 or type 1 diabetes well with Lantus insulin while following a low-carbohydrate diet. For more information, read the article “Control of type 1 diabetes” or “Step-by-step treatment regimen for type 2 diabetes.” However, diabetics who are aware of and treated with Dr. Bernstein's methods have traditionally used Levemir rather than Lantus. Therefore, it is difficult to find reviews about this drug from people who limit carbohydrates in their diet and inject low doses of the hormone.
If you haven't started using long-acting insulin yet, try Levemir or Tresiba first. But if you are already convinced that Lantus suits you well, continue to inject it. Each patient has their own diabetes. Someone else's experience usually cannot be applied 100% to your situation. Don't limit yourself to one injection per day. Accurately calculate the dosage using the method described here. Make sure that switching to a low-carb diet significantly reduces them. Write your review about using Lantus in the comments to this article.
Lantus SoloStar, instructions for use: method and dosage
The solution is intended only for subcutaneous administration by injection into the subcutaneous fat in the abdomen, thighs or shoulders. The procedure is performed daily, once a day at a convenient (but always the same) time of day for the patient. Injection sites must be alternated regularly.
Lantus SoloStar should not be administered intravenously!
To correctly perform the procedure safely on your own, you must carefully study the sequence of actions and strictly follow it.
First of all, when using a syringe pen for the first time, you must first remove it from the refrigerator and keep it at room temperature for 1–2 hours. During this time, the solution will warm up to room temperature, which will avoid the painful administration of cooled insulin.
Before the procedure, you need to make sure that your insulin is appropriate by reading the label on the syringe pen. After removing the cap, you should conduct a thorough visual assessment of the quality of the contents of the pen cartridge. The drug can be used if the solution has a transparent, colorless structure without visible solid particles.
If damage to the body is discovered or doubts arise about the quality of the syringe pen, it is strictly forbidden to use it. In this case, it is recommended to remove the solution from the cartridge into a new syringe that is suitable for 100 IU/ml insulin and inject it.
It is necessary to use needles compatible with SoloStar.
Each injection is made with a new sterile needle, which is installed before the direct administration of Lantus SoloStar.
To ensure that there are no air bubbles and that the syringe pen and needle are working properly, a preliminary safety test must be carried out. To do this, remove the outer and inner caps of the needle and measure out a dose corresponding to 2 units, position the syringe pen with the needle facing up. By gently tapping the insulin cartridge with your finger, all air bubbles are directed towards the needle and the injection button is fully pressed. The appearance of insulin at the tip of the needle indicates proper operation of the syringe pen and needle. If insulin is not released, the attempt should be repeated until the desired result is achieved.
The pen contains 80 units of insulin and accurately doses it. To establish the required dose, use a scale that allows for accuracy of up to 1 unit. Upon completion of the safety test, the dosage window should display the number 0, after which the required dose can be set. In cases where the amount of the drug in the syringe pen is less than the dose required for administration, two injections are performed using the remainder in the started syringe pen, and the missing amount from a new syringe pen.
The healthcare professional should inform the patient about the injection technique and ensure that it is performed correctly.
To inject, insert the needle under the skin and press the injection button all the way, holding it in this position for 10 seconds. This is necessary for complete administration of the selected dose, then the corner is removed.
After the injection, the needle is removed from the syringe pen and thrown away, and the cartridge is capped. Failure to follow these recommendations increases the risk of air and/or infection entering the cartridge, contamination, and insulin leakage.
The syringe pen is intended for use by only one patient! It must be stored under sterile conditions, away from dust and dirt. You can use a damp cloth to clean the outside of the pen. Do not immerse it in liquids, wash it or lubricate it!
The patient should always have a spare syringe pen available in case the used one is damaged or lost.
An empty syringe pen or one containing an expired drug should be discarded.
The syringe pen prepared for injection should not be cooled.
After opening, the contents of the syringe pen can be used for 4 weeks; it is recommended to indicate on the label the date of the first administration of Lantus SoloStar.
The dose is prescribed individually, taking into account clinical indications and concomitant therapy.
During the period of use of the drug, the patient should take into account that the onset and duration of action of insulin may change under the influence of physical activity and other changes in the condition of his body.
For type 2 diabetes mellitus, the use of Lantus SoloStar is indicated as monotherapy and in combination with other hypoglycemic agents.
Doses, timing of insulin administration and administration of hypoglycemic agents should be determined and adjusted individually, taking into account target blood glucose concentrations.
Dose adjustments should be made to prevent the development of hypo- or hyperglycemia, for example, when changing the timing of insulin dosing, body weight and/or lifestyle of the patient. Any changes in insulin dosage should only be made under medical supervision and with caution.
Lantus SoloStar is not the insulin of choice for the treatment of diabetic ketoacidosis; in this case, preference should be given to intravenous administration of short-acting insulin. If the treatment regimen includes injections of basal and prandial insulin, then insulin glargine is indicated as basal insulin in a dose that corresponds to 40–60% of the daily insulin dose.
The initial daily dose of insulin glargine for patients with type 2 diabetes mellitus during combination therapy with oral hypoglycemic agents should be 10 units. Further dose adjustment is made individually.
In all patients, treatment with the drug should be accompanied by monitoring of blood glucose concentrations.
When a patient switches to a treatment regimen using Lantus SoloStar after a treatment regimen using intermediate-acting or long-acting insulin, it may be necessary to adjust the daily dose and time of administration of short-acting insulin or its analogue and change the doses of hypoglycemic agents for oral administration.
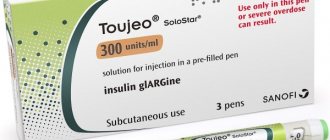
If the patient was on previous therapy with Toujeo (300 units of insulin glargine per 1 ml), then to reduce the risk of hypoglycemia when switching to Lantus SoloStar, the initial dose of the drug should not exceed 80% of the Toujeo dose.
When switching from a single daily dose of insulin isophane, the initial dose of insulin glargine is usually used in the amount of units of the drug being discontinued.
If the previous treatment regimen included two doses of isophane insulin per day, then when transferring the patient to a single dose of Lantus SoloStar before bedtime, to reduce the likelihood of hypoglycemia at night and early in the morning, its initial dose is prescribed at 80% of the daily dose of isophane insulin. During therapy, the dose is adjusted depending on the patient's response.
Switching from human insulin should be done under medical supervision. During the first weeks of using insulin glargine, careful metabolic monitoring of blood glucose concentrations and adjustment of the insulin dosage regimen as necessary is recommended. Particular attention should be paid to patients with antibodies to human insulin who require high doses of human insulin. In this category of patients, with the use of insulin glargine, a significant improvement in the response to insulin administration is possible.
As metabolic control improves and tissue sensitivity to insulin increases, the dosage regimen is adjusted.
Mixing and diluting insulin glargine with other insulins is contraindicated.
When prescribing Lantus SoloStar to elderly patients, it is recommended to use lower initial doses, their increase to the maintenance dose should be slow. It should be taken into account that in old age, recognition of developing hypoglycemia is complicated.
Classification of insulin
The origin of insulin is:
- Pork. It is obtained from the pancreas of these animals, very similar to humans.
- From cattle. There are often allergic reactions to this insulin, since it has significant differences from the human hormone.
- Human. Synthesized using bacteria.
- Genetically engineered. It is obtained from pork using new technologies, thanks to which insulin becomes identical to human insulin.
By duration of action:
- ultra-short-acting (Humalog, Novorapid, etc.);
- short-acting (Actrapid, Humulin Regular, Insuman Rapid and others);
- medium duration of action (Protafan, Insuman Bazal, etc.);
- long-acting (Lantus, Levemir, Tresiba and others).
Human insulin
Short- and ultra-short-acting insulins are used before each meal to avoid a jump in glucose and normalize its levels. Medium- and long-acting insulins are used as so-called basic therapy, they are prescribed 1-2 times a day and maintain sugar within normal limits throughout for a long time.
Side effects
- on the metabolic side: very often – hypoglycemia;
- from the immune system: rarely - allergic reactions, including low blood pressure (BP), bronchospasm, generalized skin reactions, angioedema, shock (including fatal cases);
- from the nervous system: very rarely - dysgeusia;
- from the organ of vision: rarely - transient visual impairment, retinopathy;
- dermatological reactions: often – lipodystrophy; uncommon – lipoatrophy;
- from the musculoskeletal system: very rarely – myalgia;
- disorders at the injection site: often – pain, redness, itching, swelling, inflammation, urticaria;
- general disorders: rarely - sodium retention, edema.
Overdose
Symptoms: hypoglycemia, including severe, prolonged and life-threatening episodes.
Treatment: Immediate ingestion of rapidly digestible carbohydrates often helps relieve symptoms of mild hypoglycemia. If necessary, changes should be made to the insulin dosage regimen, diet or physical activity. Episodes of severe hypoglycemia accompanied by neurological disorders, seizures or coma require the administration of glucagon (intramuscular or subcutaneous), concentrated dextrose solution (iv), and administration of carbohydrates. The patient needs careful observation by a specialist, since after visible clinical improvement, relapse of hypoglycemia is possible.
special instructions
Limited experience with the use of Lantus SoloStar does not allow us to provide a reliable assessment of its effectiveness and safety in the treatment of patients with diabetes mellitus with impaired liver function or moderate/severe renal failure.
The development of hypoglycemia may be indicated by symptoms of adrenergic counterregulation such as hunger, nervous agitation, tremor, irritability, anxiety, cold sweat, pale skin, severe palpitations, and tachycardia. Symptoms of hypoglycemia usually occur suddenly. Their severity depends on the rate of development and severity of hypoglycemia.
Further, the condition may be aggravated by the following neuropsychiatric disorders: weakness, headache, feeling of fatigue, drowsiness, nausea, unusual fatigue, decreased ability to concentrate, visual disturbances, confusion or loss of consciousness, convulsions.
Attacks of severe hypoglycemia, especially repeated ones, can cause damage to the nervous system. With prolonged and severe episodes of hypoglycemia, the threat to the lives of patients increases; with increasing hypoglycemia, death is possible.
Episodes of severe hypoglycemia in proliferative retinopathy, especially in patients not receiving photocoagulation treatment, may cause transient vision loss.
It should be taken into account that the use of Lantus SoloStar may cause the formation of antibodies that cross-react with human insulin and insulin glargine. Their presence may necessitate a revision of the dosage regimen in order to prevent the tendency to develop hypo- or hyperglycemia.
Correction of the dosage regimen if control of blood glucose levels is ineffective should be started after checking the patient’s accuracy of compliance with the treatment regimen prescribed by the doctor and a thorough analysis of all factors that may affect the concentration of glucose in the blood. It is necessary to ensure that instructions regarding injection sites and correct technique for performing subcutaneous injections are followed.
With the use of Lantus SoloStar, the time for long-acting insulin to enter the body increases, so the likelihood of developing nocturnal hypoglycemia is lower than in the early morning hours.
It should be taken into account that if hypoglycemia occurs while taking Lantus SoloStar, the patient’s recovery from the hypoglycemia state may be delayed due to the prolonged action of insulin glargine.
Patients should be informed about the following conditions and situations, against the background of which the severity of symptoms that are precursors of hypoglycemia may decrease, or they may be completely absent:
- switching to human insulin from animal insulin;
- noticeable improvement in the regulation of blood glucose concentrations;
- gradual development of hypoglycemia;
- autonomic neuropathy;
- long-term diabetes mellitus;
- presence of mental disorders;
- concomitant therapy with other drugs;
- elderly age.
The presence of normal or reduced levels of glycated hemoglobin indicates an increased risk of developing unrecognized repeated attacks of hypoglycemia, especially at night.
The tendency to hypoglycemia increases in the presence of the following factors:
- changing the area of insulin administration;
- hypersensitivity to insulin (including when eliminating stress factors);
- physical activity (increased, unusual or prolonged);
- intercurrent diseases that are accompanied by vomiting and/or diarrhea;
- violation of diet and nutrition;
- skipping meals;
- alcohol consumption;
- hypothyroidism, insufficiency of the adenohypophysis or adrenal cortex and other uncompensated disorders of the endocrine system;
- simultaneous use of other drugs.
In patients with these risk factors, insulin dosage adjustment may be required. With strict adherence to the diet, dosage regimen and correct administration of insulin and timely identification of symptoms and warning signs of hypoglycemia, patients are significantly less at risk of developing this disease.
Patients with intercurrent illnesses should not completely stop taking insulin. This category requires more intensive monitoring of blood glucose; in many cases, adjustment of the insulin dosage regimen and urine testing for the presence of ketone bodies are indicated.
The diet of patients with type 1 diabetes should regularly contain at least a small amount of carbohydrates, including in the absence of food intake or in small amounts, as well as in the case of vomiting.
Insulin injection technique
Insulin injections are carried out using an insulin syringe or pen. The latter are more convenient to use and dose the drug more accurately, so they are preferred. You can give an injection using a syringe pen without even taking off your clothes, which is convenient, especially if a person is at work or in an educational institution.
Insulin pen
Insulin is injected into the subcutaneous fatty tissue of different areas, most often the front of the thigh, abdomen and shoulder. It is preferable to inject long-acting drugs into the thigh or outer gluteal fold, short-acting drugs into the stomach or shoulder.
A prerequisite is to comply with the rules of asepsis, you must wash your hands before the injection and use only disposable syringes. It must be remembered that alcohol destroys insulin, so after treating the injection site with an antiseptic, you must wait until it dries completely and then begin administering the drug. It is also important to retreat at least 2 centimeters from the previous injection site.
Use during pregnancy and lactation
The use of Lantus SoloStar is allowed during pregnancy according to clinical indications.
The results of the studies indicate the absence of any undesirable specific effects on the course of pregnancy, as well as on the condition of the fetus or the health of newborns.
A woman should inform her doctor about the presence or planning of pregnancy.
It should be taken into account that in the first trimester of pregnancy the need for insulin may decrease, and in the second and third trimesters it may increase.
Careful monitoring of blood glucose concentrations is required immediately after delivery due to the rapid decrease in insulin requirements.
During lactation, adjustments to the insulin dosage regimen and diet should be considered.
In case of pre-existing or gestational diabetes mellitus during pregnancy, it is necessary to maintain adequate regulation of metabolic processes throughout the entire period of gestation in order to prevent the occurrence of undesirable outcomes caused by hyperglycemia.
Lantus
Active substance:
Insulin glargine*
Pharmgroup:
Insulins
Analogs for the active substance:Lantus SoloStar | Application area:Decompensation of carbohydrate metabolism Diabetes is labile Diabetes mellitus insulin dependent Diabetes type 1 Diabetic ketoacidosis Insulin dependent diabetes Insulin-dependent diabetes mellitus Coma hyperosmolar non-ketoacidotic Labile form of diabetes mellitus Disorders of carbohydrate metabolism Diabetes mellitus type 1 Diabetes mellitus type I Diabetes mellitus insulin dependent Diabetes mellitus type 1 |
Drug interactions
- oral hypoglycemic agents, angiotensin-converting enzyme inhibitors, fluoxetine, disopyramide, fibrates, pentoxifylline, propoxyphene, monoamine oxidase inhibitors, sulfonamide antimicrobial agents, salicylates: may increase the hypoglycemic effect of insulin and increase the susceptibility to the development of hypoglycemia. Use caution and adjust insulin glargine doses as needed;
- danazol, diazoxide, glucocorticosteroids, diuretics, isoniazid, estrogens, glucagon, gestagens (including hormonal contraceptives), phenothiazine derivatives, somatotropin, sympathomimetics (including epinephrine or adrenaline, terbutaline, salbutamol), protease inhibitors, thyroid hormones, some antipsychotics (including olanzapine, clozapine): may reduce the hypoglycemic effect of insulin;
- lithium salts, beta-blockers, clonidine, ethanol: can affect the hypoglycemic effect of insulin, weakening or enhancing it;
- pentamidine: increases the risk of hypoglycemia, which may be followed by hyperglycemia.
Concomitant therapy with drugs with a sympatholytic effect (including clonidine, beta-blockers, guanfacine, reserpine) in the development of hypoglycemia may partially or completely hide the signs of adrenergic counterregulation.