What role does cortisol play in the body?
When secreted normally, cortisol helps control vital processes in the body. Its tasks include controlling blood pressure, which makes it possible to maintain a normal state of the cardiovascular system; it also increases the level of glucose in the blood, thus balancing the effect of insulin, reduces the inflammatory response of the immune system, and regulates protein, carbohydrate and fat metabolism. One of cortisol's primary jobs is to help the body respond to stress. Because of this, pregnant women in their last trimester and professional athletes typically have elevated cortisol levels. People suffering from alcoholism, depression, panic disorders and malnutrition also have high levels of cortisol in the blood.
Hypersecretion of cortisol, which reaches the borders of hypercorticism and ends in the development of Itsenko-Cushing syndrome, is, as a rule, iatrogenic in nature. This syndrome is named after the authors who first understood and described the reason for the development of this complex of symptoms.
Forecast
Cushing's syndrome is a serious illness that does not go away within a week. Doctors give their patients special recommendations for organizing home therapy:
- Gradually increase physical activity and return to the usual rhythm of life with the help of minor training without overwork.
- Proper, rational, balanced nutrition.
- Performing mental gymnastics - crosswords, puzzles, problems, logical exercises.
- Normalization of psycho-emotional state, treatment of depression, prevention of stress.
- Optimal work and rest regime.
- Home methods for treating pathology are light physical exercises, water gymnastics, warm showers, massage.
If the cause of the pathology is a benign neoplasm, the prognosis is considered favorable. In such patients, the adrenal gland begins to function fully after treatment. Their chances of recovery from illness increase significantly. With adrenal cancer, death usually occurs within a year. In rare cases, doctors can extend the life of patients by a maximum of 5 years. When irreversible phenomena occur in the body and there is no competent treatment, the prognosis of the pathology becomes unfavorable.
Causes and mechanism of development of Itsenko-Cushing syndrome
There are many etiological factors that provoke the development of this syndrome. Based on the mechanism of development of hypercorticism, three types are distinguished: endogenous, exogenous and pseudo-Cushing's syndrome.
As already stated, the basis of pathological changes in the development of Itsenko-Cushing syndrome is the hyperproduction of cortisol. An increased amount of cortisol has a destructive effect on most tissues and structural units of the body (internal organs, skin, muscles, including the myocardium), in which pronounced atrophic and dystrophic changes occur over time. Hypercortisolism counteracts insulin, increasing blood glucose levels, which triggers the development of steroid-induced diabetes. Regarding fatty tissue, hypercortisolism carries out a complex tactics of damage, which is expressed in excessive obesity of some areas and atrophy of others, this is due to the different tolerance of individual fatty areas to glucocorticoids. Cushing's symptom causes electrolyte disturbances (hypernatremia, hypokalemia), which are caused by the effect of excess cortisol on the kidneys. The consequence of these electrolyte changes is the development of arterial hypertension, as well as aggravation of myocardial changes, which leads to arrhythmia and the development of heart failure. An increase in cortisol levels has a detrimental effect on the body's immune system, suppressing its functions and causing a tendency to infections.
Etiology
Etiopathogenetic factors of Cushing's syndrome are divided into two groups - endogenous and exogenous.
- The first group includes hyperplastic processes and neoplasms of the adrenal cortex. A hormone-producing tumor of the cortex is called corticosteroma. By origin, it can be an adenoma or adenocarcinoma.
- The exogenous cause of hypercortisolism is intensive and long-term therapy of various diseases with corticosteroid and corticotropic hormones. Drug syndrome develops with improper treatment with Prednisolone, Dexamethasone, Hydrocortisone, Diprospan. This is the so-called iatrogenic type of pathology.
- Pseudo-Cushing's syndrome has a similar clinical picture, but is caused by other causes not related to damage to the adrenal glands. These include nutritional obesity, alcohol addiction, pregnancy, and neuropsychiatric diseases.
- Cushing's disease is caused by increased production of ACTH. The cause of this condition is a pituitary microadenoma or corticotropinoma located in the bronchi, testicles or ovaries. The development of this benign glandular tumor is facilitated by head trauma, previous neuroinfections, and childbirth.
Types of hypercortisolism:
- Total hypercortisolism develops when all layers of the adrenal cortex are affected.
- Partial is accompanied by isolated damage to individual cortical zones.
Pathogenetic links of Cushing's syndrome:
- hypersecretion of cortisol,
- acceleration of catabolic processes,
- breakdown of proteins and amino acids,
- structural changes in organs and tissues,
- disturbance of carbohydrate metabolism leading to hyperglycemia,
- pathological fat deposits on the back, neck, face, chest,
- acid-base imbalance,
- decreased potassium in the blood and increased sodium,
- rise in blood pressure,
- suppression of immune defense,
- cardiomyopathy, heart failure, arrhythmia.
Persons at risk for developing hypercortisolism:
- athletes,
- pregnant women,
- drug addicts, smokers, alcoholics,
- mentally ill.
Symptoms of Itsenko-Cushing syndrome
Symptoms of Itsenko-Cushing syndrome are represented by characteristic changes in the appearance of patients; patients with this pathology have a so-called Cushingoid appearance. The patient's face becomes moon-shaped, 90% of patients are obese. Fat deposits are uneven and localized on the face, neck, chest, abdomen and back. The face acquires a purplish-red color, in some cases with a cyanotic tint; this phenomenon is called “matronism.” Even in the absence of obesity in severely ill patients, a characteristic redistribution of subcutaneous fat occurs.
List of sources
- Belchenko L.V. Clinical, biochemical and computed tomographic criteria for the diagnosis and treatment of Itsenko-Cushing’s disease. Author's abstract. dis. Ph.D. honey. Sci. Moscow 1991, 25 p.
- Clinical endocrinology. Guide / Ed. N. T. Starkova. — 3rd ed., revised. and additional - St. Petersburg: Peter, 2002. - pp. 62-81. — 576 p.
- Komissarenko I.V., Efimov A.S. Treatment of Itsenko-Cushing's disease. //Problem Endocrinology.// 1973, T.19, No. 1, P108-112
- Marova E.I. Algorithm for diagnosis and treatment of Itsenko-Cushing's disease // Probl. endocrinol. -1992. No. 1. - P. 39
- Tishenina R.S. Hormonal and metabolic aspects of Itsenko-Cushing's disease and various forms of obesity. Author's abstract. diss doc med. Sci. Moscow 1990, 49 p.
Skin changes
Changes in the skin are expressed in marbling of the skin, emphasized vascular pattern, thinning, dryness, peeling, and areas of regional sweating. The combination of skin collagen breakdown and obesity provokes the appearance of stretch marks (striae). Striae are localized on the skin of the abdomen, shoulders, mammary glands, inner thighs, have a purple or purplish-red color and can be several centimeters in size. Often there is an acne-type skin rash and numerous small petechiae. In some cases, hyperpigmentation is observed in areas of friction.
Other characteristic symptoms
Itsenko-Cushing syndrome in 10-20% of cases is accompanied by steroid diabetes mellitus, which has no connection with pancreatic diseases. This type of diabetes has a fairly mild course and can be eliminated with the help of a special diet and glucose-lowering medications.
In some cases, peripheral edema develops, as well as poly- and nocturia.
With prolonged hypercortisolism, men may develop:
- signs of feminization;
- decreased libido and potency;
- testicular atrophy;
- gynecomastia.
In women, hyperandrogenism can provoke:
- virilization;
- hypertrichosis;
- hirsutism;
- amenorrhea;
- menstrual irregularities;
- infertility.
Diagnosis of Itsenko-Cushing syndrome
If there is a suspicion of Itsenko-Cushing syndrome, and such suspicions arise after examining the patient and determining typical changes in appearance, a series of clinical and biochemical analyzes of blood and urine samples is indicated. In order to find the root cause of this pathology, the patient is advised to conduct topographic studies, as well as CT and MRI of certain areas.
An important point in diagnosing the Itsenko-Cushing symptom complex is the exclusion of exogenous intake of glucocorticoids (including intra-articular and inhaled).
To confirm this disease, the following tests must be performed:
- determination of the level of cortisol excretion in daily urine: the presence of an increase in excreted cortisol by 3-4 times compared to the norm confirms the reliability of the diagnosis of Itsenko-Cushing syndrome;
- conducting a small dexamethasone test, the essence of which is to determine the level of cortisol after taking dexamethasone. To carry out this test, the patient first needs to determine the cortisol level on the first day at 8-9 am, then at 24 o'clock on the same day take a dose of dexamethasone, and the next day at 8-9 am the cortisol level is determined again. Normally, taking dexamethasone helps reduce cortisol levels by more than half; in patients with Cushing's syndrome, this reaction does not occur.
Studies of biochemical parameters of urine in the Itsenko-Cushing symptom complex determine an increased level of 11-hydroxyketosteroids (11-OX) and a decrease in the level of 17-hydroxyketosteroids (17-OX). There is hypokalemia in the blood, an increase in the level of red blood cells, cholesterol and hemoglobin. Also, laboratory tests can show the presence of complications (steroid-induced diabetes mellitus, electrolyte shifts).
To determine the location of the root cause, the patient is advised to undergo CT, MRI of the pituitary gland, adrenal glands and adrenal scintiography.
In order to identify complications of hypercorticism (rib fractures, vertebrae due to osteoporosis), an X-ray examination or CT scan of the vertebrae and chest is performed.
Complications of Itsenko-Cushing syndrome
Long-term lack of therapy for the chronic course of Itsenko-Cushing syndrome can provoke the death of the patient due to complications such as stroke, cardiac decompensation, sepsis, chronic renal failure, severe pyelonephritis, osteoporosis with the presence of multiple fractures of the spine and ribs.
Reduced resistance to infections with hypercortisolism often becomes a predisposing factor to the development of phlegmon, furunculosis, fungal and suppurative skin lesions.
With Itsenko-Cushing syndrome, an emergency state of adrenal (adrenal) crisis may develop, which manifests itself in the form of arterial hypotension, nausea, vomiting, impaired consciousness, abdominal pain, hypercalcemia, hypoglycemia and metabolic acidosis.
As a rule, urolithiasis in hypercortisolism is associated with osteoporosis and hypersecretion of phosphate and calcium in the urine, which contribute to the formation of phosphate and oxalate kidney stones.
Itsenko-Cushing syndrome during pregnancy can cause miscarriage or complicated childbirth.
Pathological anatomy
In the adenohypophysis of most patients, hyperplasia of basophilic adenocytes or basophilic adenomas is found, less often adenomas arising from other types of adenocytes. Damage to the nuclei of the diencephalon has been described. In the adrenal glands, diffuse nodular hyperplasia of the zona fasciculata and zona reticularis is detected. In the heart there is myocardial hypertrophy and signs of the development of steroid cardiopathy, manifested by metabolic disorders. Fatty infiltration of the liver, hypoplasia of the gonads, and a primary wrinkled kidney are also detected. Atherosclerosis is mild, myocardial infarction rarely develops. As a result of decalcification of bones and the release of large amounts of calcium, nephrocalcinosis (see) develops and kidney stones are formed, osteoporosis of varying degrees.
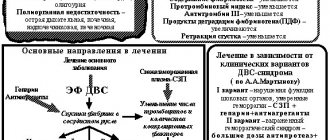
Treatment of Itsenko-Cushing syndrome
The treatment strategy for the iatrogenic (drug) form of Itsenko-Cushing syndrome consists of gradually withdrawing glucocorticoids and prescribing other immunosuppressants instead.
The presence of the endogenous nature of hypercortisolism syndrome implies treatment with drugs that suppress steroidogenesis (chloditan, mitotane, ketoconazole, aminoglutethimide).
If a tumor of the pituitary adrenal gland is diagnosed, surgical treatment is advisable; if it is impossible to remove the tumor, unilateral or bilateral adrenalectomy (removal of the adrenal glands) is performed or a course of radiation therapy of the hypothalamic-pituitary region is performed. To enhance the effect and minimize relapses, radiation therapy is often carried out in combination with drug and surgical treatment. If a pituitary adenoma is not visualized in patients with Cushing's syndrome, the use of proton therapy in the pituitary region is indicated.
In addition to basic therapeutic measures, patients with Itsenko-Cushing syndrome are prescribed symptomatic treatment. Symptomatic therapy consists of prescribing diuretics, antihypertensives, hypoglycemic drugs, bistimulants, immunomodulators, cardiac glycosides, sedatives or antidepressants, drug therapy for osteoporosis, and vitamin therapy.
The principle of postoperative treatment of patients with chronic adrenal insufficiency who have undergone surgery to remove the adrenal glands is lifelong hormone replacement therapy.