Raynaud's syndrome is a pathological condition characterized by a sharp spasm of peripheral vessels, trophic disorder and the appearance of pain. Vasospasm leads to paroxysmal disruption of blood flow in the capillaries and arterioles of the hands and feet. The etiology of the syndrome is not fully understood. It is believed that reversible narrowing of blood vessels occurs due to psycho-emotional stress, stress or cold exposure.
The syndrome was first described in 1863 by a neurologist from France, Maurice Raynaud. The doctor studied in detail and systematized the signs of this pathology, but initially classified it as a group of neuroses. He called the cause of the disease excessive excitability. Modern scientists have refuted this assumption. They observed young washerwomen who regularly came into contact with cold water, one of the main triggers of the syndrome. The skin of their hands first turned pale and then turned blue. These phenomena were accompanied by sensory disturbances, tingling, and pain in the hands. The conclusion suggested itself: long-term hypothermia is the cause of vasospasm and discirculatory disorders.
Raynaud's syndrome in most cases is a manifestation of systemic diseases - collagenosis, scleroderma, rheumatism, vasculitis, as well as endocrinopathies, psychopathy, hematological and neurological diseases. In extremely rare cases, the syndrome acts as an independent nosology, the causes of which have not been established.
Patients experience paroxysmal vascular spasm. Acute circulatory disturbance in a limited area of the body is the pathomorphological basis of the syndrome. This phenomenon is caused by a disorder in the functioning of the autonomic nervous system, namely an increase in the tone of its sympathetic department. The syndrome most often occurs in residents of countries with cold climates. It affects mainly young and mature women. Symmetry and bilaterality are a mandatory sign of angiotrophoneurosis. Therapeutic measures involve the use of drugs that dilate blood vessels. In severe cases, surgery is indicated. In the absence of timely and correct treatment, trophic changes in soft tissues occur.
Causes of Raynaud's disease
It is believed that the cause of excessively pronounced vasospasm in response to provoking stimuli is a defect in the central and local mechanisms of regulation of vascular tone. Among these factors, vascular endothelial, intravascular and neurovegetative disorders are important. In secondary SR, structural changes in blood vessels are also a significant factor.
Factors that provoke vasospastic reactions are low ambient temperature and/or emotional stress.
Physiotherapy
Treatment methods are aimed at relieving symptoms, and during remission, at stopping attacks. The methods are quite effective, especially in the initial stages of the disease, and are very diverse.
Lymph drainage:
- massage of the collar zone - this activates the regional blood supply and reflex zones. Massage increases microcirculation and improves lymphatic drainage, preventing swelling. The course includes at least 15 procedures;
- magnetic therapy – a traveling magnetic field reduces the tone of the venules, which improves the outflow of blood and lymph. The procedure is carried out at different magnetic frequencies, at least 10 times;
- segmental vacuum therapy - the cervicothoracic region or collar area is affected using a vacuum applicator. At the same time, the hydrostatic pressure gradient increases, which leads to a decrease in arteriolar tone and active lymph outflow.
Vasodilator methods:
- electrophoresis of vasodilators - for example, with nicotinic acid, which quickly relieves swelling and reduces painful symptoms;
- ultratonotherapy is a combination of high voltage currents and supersonic frequencies. Strengthens the outflow of blood and lymph;
- barotherapy - exposure to high and low pressure, especially indicated for obliterating endarteritis;
- IR irradiation stimulates capillary blood circulation and improves oxygen supply to soft tissues.
Hypocoagulating methods:
- low-frequency magnetic therapy - exposure to a low-frequency field. Improves blood supply to tissues and trophism;
- laser irradiation of blood - the effectiveness of the procedures is based on the absorption of a laser beam of a certain length by the molecular structures of the blood. This improves the rheological composition of the blood, which leads to a reduction in spasmodic phenomena.
They also resort to stimulating procedures: pearl showers, thalassotherapy, aerotherapy, contrast baths.
Symptoms
Clinical features of Raynaud's syndrome:
- most often, color changes are observed on the fingers;
- changes begin on one finger, then spread to other fingers and become symmetrical on both hands;
- the II-IV fingers of the hands are most often involved, the thumb usually remains unchanged;
- changes in skin color may also be observed in other areas: ears, tip of the nose, face, above the knees;
- during Raynaud's attacks, livedo reticularis may appear on the extremities, which disappears after the completion of vasospasm;
- in rare cases, damage to the tongue is observed, which is manifested by numbness and transient speech impediments.
Clinically, an attack of Raynaud's disease consists of three phases:
- The first phase is expressed in spasm of the arteries, pallor of the skin, a decrease in its temperature, numbness, and pain.
- The second phase is characterized by the development of cyanosis of the skin and increased pain.
- The third phase is swelling and redness of the skin, decreased pain.
However, classic three-phase Raynaud's attacks are observed only in 15% of patients; in most cases, two-phase color changes are observed Source: Alekperov R.T. Raynaud's syndrome in the practice of a rheumatologist / R.T. Alekperov // Modern rheumatology. - 2014. - No. 2. - P. 37-46. .
The duration of the attack is usually 15-20 minutes, but sometimes it can last even several hours.
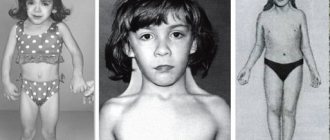
At the last stage of the disease, persistent skin lesions develop, and deformation of the fingers is possible.
In most cases, Raynaud's disease is symmetrical in nature: if the pathology affects one hand, then after some time the pathology develops on the second.
Pathogenesis
Autoimmune processes are characterized by the formation in the body of autoantibodies to its own cells and tissues, which are perceived by it as foreign. Genetic predisposition plays an important role in the development of such changes. The onset of inflammation is most often provoked by an infection. It is viruses and bacteria that are the antigens against which antibodies are produced, which also attack their own structures.
- With collagenosis, the vascular wall of arterioles and capillaries becomes inflamed, their structure changes, and the functioning of the endothelium is disrupted. Blood vessels narrow, which leads to dyscirculatory disorders. In parts of the body far from the heart, blood circulates somewhat worse. This is associated with vascular spasm in the distal extremities, nose and tongue. The spasmodic area turns pale due to the complete emptying of the capillaries. Prolonged hypoxia leads to impaired trophism and pain. This is how the ischemic stage of the syndrome develops.
- Since blood circulation is temporarily stopped, it accumulates in the venules. They become filled with blood and the affected area turns blue. Blood retention in venules and arteriovenular anastomoses leads to local cyanosis. This is the second cyanotic stage of the disease. A sharp spasm of blood vessels is always accompanied by numbness and pain. It is caused by the formation of lactic acid in tissues subject to oxygen starvation. Lactic acid is a pain provocateur.
- The third stage is manifested by hyperemia caused by vasodilation, restoration of local blood flow and a sharp rush of blood. As the pathology progresses, a mesh vascular pattern, blisters with hemorrhagic or serous contents, and areas of necrosis appear on the skin.
Blood rheology also influences systemic blood flow. Increased blood viscosity and coagulability are the cause of thrombosis. Blood clots obstruct blood flow. Blood circulation first slows down and then stops completely, which is also manifested by pallor, cyanosis and hyperemia. When there is a lack of mediators and hormones in the blood that are responsible for the normal reaction to stress, a spasm of blood vessels occurs. A pathological reaction to negative endogenous and exogenous factors also manifests itself as vasospasm.
The risk group for this pathology includes typists, computer users, pianists, as well as people suffering from migraines.
Diagnosis of Raynaud's phenomenon
The diagnosis of Raynaud's disease is established primarily on the basis of complaints and clinical symptoms and is considered reliable if the answer to the following questions is positive:
- Is there any unusual sensitivity to cold?
- Does the color of fingers change when exposed to cold?
- do they turn white and/or bluish?
Along with the diagnosis of SR, its clinical variant is specified - primary or secondary. For this purpose, such instrumental and laboratory methods as laser Doppler flowmetry, thermography, the QNL method, plethysmography, and color Doppler ultrasound scanning are used.
Diagnostic measures
Diagnosis of the pathology does not cause any particular difficulties for specialists, since the symptoms of the syndrome are very specific. To find out its cause, it is necessary to refer the patient for a comprehensive comprehensive examination. Doctors talk with the patient, examine him, find out complaints, collect anamnesis of life and illness. The results of additional methods - laboratory and instrumental - are important in making a diagnosis and prescribing treatment.
A cold test allows you to assess the state of blood flow. The patient's skin is exposed to cold temperatures, causing vasospasm, and then the hands are warmed. In healthy people, the spasm quickly passes - the skin becomes pink without signs of cyanosis. In people with Raynaud's syndrome, this process takes longer. There may be areas of blue discoloration.
Laboratory diagnostics:
- Hemogram - increased ESR, erythrocytopenia, leukopenia, thrombocytopenia.
- Blood test for biochemical markers - dysproteinemia, increase in certain enzymes: creatine phosphokinase, LDH, ALT, AST, aldolase.
- Coagulogram - increased blood viscosity and platelet clotting ability, decreased clotting time.
- General urine analysis - proteinuria, hematuria, cylindruria, myoglobinuria.
- Immunogram - increased Ig M, G, E, many immune complexes, the presence of rheumatoid factor and specific antibodies to various diseases.
Angiography, capillaroscopy, radiography with contrast of blood vessels, ultrasound and tomographic examinations of the spine and internal organs, as well as Dopplerography of blood vessels are additional methods that allow us to identify the cause of the syndrome and differentiate it from other diseases with similar symptoms.
After receiving all the results of the study, the doctor prescribes the correct treatment aimed at eliminating Raynaud's phenomenon itself or the underlying disease manifested by this syndrome.
Treatment of Raynaud's syndrome
Effective treatment for Raynaud's disease must be comprehensive. First of all, it is necessary to eliminate the factors that provoke attacks.
The treatment program for the disease includes medication and physical therapy. In some cases, surgical treatment methods are indicated.
Drug therapy consists of:
- painkillers;
- vasodilators;
- anti-inflammatory drugs;
- antibacterial drugs;
- vitamin complexes.
Physiotherapeutic procedures for the treatment of Raynaud's disease include ultraviolet irradiation, galvanic baths, electrophoresis, etc.
Forecasting and preventive measures
Raynaud's syndrome is a pathology with a relatively favorable prognosis. If the underlying disease does not progress and there are no provoking factors, the syndrome responds well to therapy. In some cases, it is enough to change your place of residence, climate conditions, profession, and ischemic attacks will cease to occur.
Preventive measures to avoid Raynaud's syndrome:
- Constant protection of hands and feet from the cold with the help of mittens, gloves, warm socks,
- Fighting bad habits, especially smoking,
- Treatment of concomitant diseases,
- Protecting the body from hypothermia, exposure to harmful physical and chemical factors,
- Stress prevention, positive mood,
- Hardening your hands with contrast baths,
- Proper nutrition,
- Maintaining a healthy lifestyle,
- Wearing clothes that suit the season and shoes that fit,
- Lubricating your hands and feet with a nourishing cream before going to bed,
- Using mild soap
- Protect your hands with household gloves when using aggressive cleaning agents and disinfectants.
It happens that a banal narrowing of blood vessels becomes a cause of disability. This seemingly not the most dangerous disease often leads to serious consequences. Gangrene and limb amputation are the outcome of the syndrome, which can occur in patients who do not seek medical help in time.
Prevention
To prevent Raynaud's disease, medical experts recommend using contrast baths to train blood vessels. It is also necessary to eat properly and nutritiously, and not to overuse coffee, as it constricts blood vessels.
Avoid overheating; in cold weather, always wear gloves and dress appropriately for the weather.
Raynaud's disease should only be treated under the supervision of a qualified physician. You can get quality medical care in.
Treatment process
Emergency measures will help alleviate the condition during an attack before the start of treatment procedures. The affected limb must be warmed by holding it in warm water or massaging it with a woolen cloth. It is useful to drink a cup of hot tea. Vigorous swings of the arms raised above the head promote a rush of blood to the hands.
Patients with Raynaud's syndrome must receive medications for life. They are prescribed the following medications:
- Vasodilators - Nifedipine, Diltiazem, Verapamil, Capoten, Lisinopril;
- Antiplatelet agents – “Pentoxifylline”, “Trental”, “Vazonit”;
- Antispasmodics – “Drotaverine”, “Platifillin”;
- NSAIDs – “Indomethacin”, “Diclofenac”, “Butadione”;
- Glucocorticosteroids – “Prednisolone”, “Dexamethasone”;
- Cytostatics – “Methotrexate”.
Surgical treatment is performed if there is no effect from conservative therapy. Sympathectomy or ganglectomy are operations that are indicated for all patients with a progressive form of the disease. In order to prevent a new spasm of blood vessels, during the surgical intervention the nerve fibers along which pathological impulses travel are “switched off”. Currently, sympathectomy is performed endoscopically. The syndrome may recur 2-3 weeks after surgery.
Non-drug techniques used to treat Raynaud's syndrome:
- psychotherapy,
- acupuncture,
- electrophoresis,
- magnetotherapy,
- oxygen therapy,
- massage,
- hydrotherapy,
- exercise therapy,
- paraffin applications,
- ozokerite,
- mud treatment,
- UHF,
- extracorporeal hemocorrection.
The disease can be treated using traditional medicine. For this use:
- contrasting pine and turpentine baths,
- heat compresses from pumpkin or aloe juice,
- adaptogens,
- decoction with wild strawberries, celery and parsley juice, rosehip infusion, remedy with lemon and garlic, onion mixture, pine decoction, knotweed tincture.
Diet is of great importance in the treatment of patients. It consists of excluding fatty foods, smoked meats, sauces, and sausages from the diet. You should eat foods high in ascorbic acid, rutin, and fiber.
The treatment process is labor-intensive and long. It requires a lot of patience and discipline from the patient and the doctor. To stop the steady progression of the pathology, it is necessary to eliminate all existing etiopathogenetic factors.
General information
Raynaud's syndrome is a disorder that causes severe constriction of the blood vessels of the skin, which occurs in humans as a result of severe stress or exposure to cold.
This disease was named after Maurice Raynaud, who described this disease in 1862. This disorder is paroxysmal, vasospastic in nature. It is classified as a systemic connective tissue disease. According to various sources, this disease affects 3 to 5% of the population. At the same time, women are more often susceptible to attacks of this syndrome. As a rule, Raynaud's syndrome manifests itself in a person at a later age, after 35 years. At the same time, Raynaud's disease can occur in people as early as fifteen years of age.
Raynaud's syndrome is a manifestation of the so-called Raynaud's phenomenon . In medicine, this phenomenon is usually divided into two types. Raynaud's disease is defined as primary Raynaud's phenomenon. Its peculiarity is its course regardless of other diseases. Among the total number of cases of this condition, Raynaud's disease accounts for approximately 90% of cases.
Raynaud's syndrome is defined as a secondary Raynaud's phenomenon, since this pathology mainly manifests itself as part of another illness.
Etiology
The etiology of Raynaud's disease is not specified, as with other angiotrophoneuroses. Hereditary predisposition, constitutional defects of vasomotor innervation and its functional disorders of an unexplored nature are important; Psychogenic factors and trauma appear to play a certain role. n. pp., chronic intoxication with nicotine, alcohol. Raynaud's disease is more often observed in young women, sometimes developing after infectious diseases, in some cases after exposure to provoking factors (hypothermia, excessive insolation, fatigue). Pay attention to the relatively high incidence among typists and pianists, as well as the combination of R. b. with migraine (see).
The cause of the development of Raynaud's syndrome may be systemic connective tissue diseases and related processes (scleroderma, dermatomyositis, Hamman-Rich disease); ovarian dysfunction, diseases of the thyroid gland and adrenal glands; diseases of the nervous system (for example, inflammation of the anterior roots of the spinal nerves; diseases leading to cervicobrachial syndrome (accessory ribs, muscle hypertrophy); obliterating lesions of the vessels of the extremities (see), cryoglobulinemia, etc. Thermal lesions can lead to the development of Raynaud's syndrome with chronic exposure to cold such as trench foot (see) or the consequences of sharp temperature fluctuations; mechanical damage to the hands, especially vibration disease (see), intoxication with certain poisons - ergot, heavy metals (lead, mercury), vinyl chloride. These same exogenous effects in R. b. can act as factors contributing to its progression.
Recommendations
A consultation with a neurologist and Doppler flowmetry using functional tests are recommended.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Head of the Department of Russian State Medical University, Professor, Academician of the Russian Academy of Medical Sciences Gusev E.I. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| G. AVANZINI, Italy. |
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0 | 1 | 1 | 5 | 10 | 0 | 0 | 0 | 40 | 40 | 30 | 10 |
Unconventional approach to treatment
First of all, patients diagnosed with Raynaud's syndrome are recommended to massage the affected areas - fingers, arms, lower limbs. Massaging movements should begin from the fingertips, gradually moving to the shoulder. The movements should be smooth - you can stroke the skin, rub, pinch, pat. This massage should be carried out for at least 2 weeks for 10 minutes. After this, you need to take a break for 1 week and then repeat the course again. If the clinical symptoms of the disease extend to the earlobes, then they also need to be massaged, stroked and rubbed.
To make the treatment even more effective, massage can be carried out by first moistening your hands with massage oil and adding a few drops of essential oil of mint, anise, motherwort or yarrow. These oils have an antispasmodic and analgesic effect.
Hot baths with the addition of a decoction of herbs - motherwort, valerian root, dill inflorescences, yarrow - have proven themselves well. You can also add a few drops of the essential oils listed above to the water. The duration of the therapeutic bath is 15 minutes, and the water temperature should not exceed 39-40 degrees. During this time, the patient warms up properly, the blood supply to small blood vessels increases, and the heartbeat quickens.
Instead of a bath, you can try soaks. They are prepared in the same way as a medicinal bath, only they dip their hands or feet in water. It is important to monitor the temperature of the water - you should not keep your limbs in the bath after the water has cooled. Not only will this not be beneficial, but it may also worsen Raynaud's attacks.
Pathological anatomy
In pathomorphological. Raynaud's disease is characterized by hypertrophy of the smooth muscles of the digital arteries. Subsequently, dystrophic type bone changes occur in the phalanges of the fingers, interphalangeal joints, and osteolysis of the nail tuberosities (tubercles of the distal phalanges). The most severe local changes are observed with the development of necrosis (see) and gangrene of soft tissues (see Gangrene), sometimes involving bones (see Osteonecrosis). However, these changes do not differ from those observed in burns, frostbite, leprosy, scleroderma, tabes dorsalis and neurological diseases. With various variants of Raynaud's syndrome, morphological signs of the underlying disease that led to its development are identified.