| Parainfluenza belongs to a group of viruses called anthroponotic acute respiratory viral infection (HPIV - the common abbreviation or AARVI). This group includes four viruses, each of which causes different symptoms and illnesses. All forms of HPIV cause infections of the upper or lower respiratory tract in humans. |
Fast passage:
- Types of parainfluenza viruses
- Pathogenesis of parainfluenza
- Routes of transmission of parainfluenza
- Symptoms of parainfluenza
- Diagnosis of parainfluenza
- Treatment of parainfluenza
- Medicines for parainfluenza
- Prevention of parainfluenza
- How dangerous is parainfluenza?
The symptoms of HPIV are very similar to those of the common cold, and when the symptoms are quite mild, the viruses are often misdiagnosed. Most healthy people infected with HPIV recover without drug treatment. On the other hand, a person with a weakened immune system is at major risk, since the virus can cause a number of serious complications.
What is parainfluenza and how does it develop?
Parainfluenza is a disease of infectious viral origin that primarily affects the upper respiratory tract, affecting the lower organs only in the presence of complications.
Parainfluenza can occur in different ways. Patients with a mild course of the disease often believe that they have a common cold, but some patients experience severe symptoms that a person far from medicine may mistake for the flu.
Attention! Influenza, parainfluenza - diseases similar in name, they belong to ARVI, but have significant differences - they are provoked by different pathogens and differ in clinical appearances.
Parainfluenza is a highly contact disease transmitted from a sick person who is considered contagious from the first days of incubation until the end of the acute period. Parainfluenza causes a high level of morbidity in kindergartens - among all acute respiratory viral infections, about 30% of children in the autumn suffer from parainfluenza.
Epidemiology of parainfluenza
Parainfluenza is widespread. The incidence rate rises in the autumn-spring period, sporadic cases are recorded throughout the year. The source of infection is a sick person in the first days of illness, when catarrhal symptoms (cough, rhinitis) are most pronounced.
The route of transmission is airborne, possibly household contact . People of all ages get sick, but children are more susceptible to infection. The parainfluenza virus-2 is isolated more often in the case of an uncomplicated course, the parainfluenza virus-3 - in the case of a complicated form (bronchitis, pneumonia).
Parainfluenza virus
The causative agent of parainfluenza is a virus containing ribonucleic acid and belonging to the Paramyxovirus family. It is distinguished by its high affinity for the mucous membrane of the upper respiratory tract. It quickly breaks down outside the human body - at temperatures above 50°C it dies within half an hour, and at 30°C it dies in 2-4 hours.
The parainfluenza virus is not able to mutate, forming new serotypes, so the disease is sporadic and does not cause large-scale epidemics. But, having a high contact rate, it quickly spreads among people in close contact.
Parainfluenza
Signs
The incubation period of the disease depends on the type of virus and lasts 2-7 days.
Then the patient complains of a mild headache, weakness, slight chills, and muscle aches. The temperature is often low-grade, but sometimes rises to significant levels. It was noticed that the temperature reaches its maximum on 2-3 days. Almost from the beginning of the disease, the sufferer’s nose is stuffy, the throat hurts, the voice is hoarse, the cough is dry, often “barking.” The patient is also worried about a severe runny nose with serous discharge.
In adults, the disease is milder than in children. Children with parainfluenza may have hallucinations and meningeal syndrome, but fortunately this is rare. The tonsils become enlarged and their throat often turns red.
Description
Parainfluenza is caused by the RNA parainfluenza virus of the Paramyxoviridae family. Experts identify 5 types of this virus, two of which are not dangerous to humans. The remaining three species are ubiquitous. All of them are unstable in the external environment; at room temperature they die within 4 hours, and when heated to 50°C - after half an hour.
The parainfluenza virus was discovered in 1952 by N. Kuroda. It happened in the Japanese city of Sendai, and the virus was originally called the Sendai influenza D virus. Later, in 1954 and 1957, other viruses were isolated that were very similar to the influenza virus. And in 1959 they were called parainfluenza.
Outbreaks of parainfluenza are usually recorded in autumn and winter, although they can cause illness in other seasons. Mostly preschoolers and primary schoolchildren suffer. Doctors often diagnose not specifically parainfluenza, but ARVI. According to statistics, approximately 20% of acute respiratory viral infections in adults and 30% of acute respiratory viral infections in children are caused by parainfluenza.
The source of infection is a person suffering from parainfluenza, and it is most dangerous on the 2-3rd day from the onset of the disease. The disease is transmitted by airborne droplets. Viruses enter the mucous membranes of the nose, throat, and larynx, invade epithelial cells and multiply in them. Because of this, the epithelium is gradually destroyed. An inflammatory reaction slowly develops, the mucous membrane swells. The virus also penetrates into the blood, but viremia (presence of the virus in the blood) usually does not last long.
In young children, parainfluenza is often complicated by false croup. This occurs due to rapidly increasing swelling of the larynx and accumulation of mucus in its lumen. False croup often develops at night. At the same time, the child becomes restless, his breathing is difficult, his voice is hoarse, and the skin of the nasolabial triangle acquires a bluish tint.
In adults, parainfluenza is often complicated by pneumonia, sore throat, otitis media or sinusitis. In addition, against the background of parainfluenza, chronic diseases can worsen.
Diagnostics
The diagnosis of “parainfluenza” is made by a local physician or infectious disease specialist. It is difficult to diagnose this disease, since it has no characteristic signs, it is similar to other ARVIs. The patient is referred for general and biochemical blood tests, and a general urinalysis. Parainfluenza virus is identified by immunofluorescence. In this case, nasal discharge is taken for analysis. It is also possible to isolate the virus from a patient's blood, but this test takes time.
The disease is differentiated from influenza and other acute respiratory viral infections.
Treatment
There is no specific treatment for parainfluenza. Patients are prescribed antiviral drugs and immunomodulators. At temperatures above 38.5°C, antipyretics are prescribed.
When coughing, expectorants and sputum thinners are prescribed.
For a runny nose, vasoconstrictors are prescribed. However, they cannot be used for longer than 5-7 days. In addition, it is useful to rinse your nose with a solution of sea salt.
Phytotherapy is widely used in the treatment of parainfluenza - diaphoretics (raspberry, linden), expectorants (licorice, coltsfoot), anti-inflammatory (chamomile, sage, eucalyptus, calendula).
The room of a person suffering from parainfluenza must be ventilated several times a day. Daily wet cleaning is also necessary.
In case of complications, antibiotics or antibacterial drugs are prescribed.
Prevention
To prevent parainfluenza, it is necessary to isolate those suffering from this disease from healthy people. During their illness, they need separate dishes and cutlery.
It is important to harden yourself, strengthen your immune system, and take vitamins if necessary. During outbreaks, it is better to avoid crowded places where you can become infected with parainfluenza and other acute respiratory viral infections.
© Dr. Peter
Etiology of the disease
Parainfluenza develops when its pathogens penetrate the respiratory system. The reason for the development of parainfluenza is direct contact with a sick person, even if he does not yet have symptoms of the disease.
Children of early preschool age and adults, due to their professional activities, are in contact with a large number of people, have the greatest predisposition to infection.
Parainfluenza is a sporadic disease that occurs more often in the autumn-winter period. In spring and summer, the incidence rate is much lower, and most patients during this period are children under 5 years of age.
Etiology and epidemiology
The causative agent of the pathology is an RNA virus from the Paramyxoviridae
(paramyxoviruses). The parainfluenza virus is tropic to the epithelium of the respiratory system and is practically unstable to external factors - when heated to 50° it is inactivated in 30 minutes, and at 30° it dies in 4 hours.
Parainfluenza is a sporadic disease that usually occurs in the autumn or winter seasons. Group outbreaks of parainfluenza infection may occur in children's groups.
The most susceptible category of people to parainfluenza are children from one to five years of age. Infants under the age of 4 months practically do not get sick, since they retain passive immunity.
The route of spread of infection is airborne droplets, the source is a sick person with catarrhal symptoms. A high risk of infection is observed in the first two days, and in the next 10 days the risk of infection gradually decreases. Virus carriers are not dangerous to others because they do not have catarrhal syndrome.
Types, forms, types and severity of parainfluenza
Parainfluenza infection can occur typically and atypically. The typical course of the disease is said to occur when the clinical manifestations have characteristic features of parainfluenza, which makes it possible to make a diagnosis without special diagnostic measures.
Types of parainfluenza:
- HPIV-1 - affects the upper respiratory tract and larynx, causes stenosis and false croup in children. Most common in autumn.
- HPIV-2 also causes damage to the upper respiratory organs and croup, but is much less common than the first type.
- HPIV-3 is most common in the spring and summer. Causes severe swelling of the airways, affecting the bronchi and lungs (bronchiolitis and pneumonia).
- HPIV-4 is almost never seen; no outbreaks of parainfluenza caused by this type have been diagnosed for a long time.
Atypical parainfluenza occurs in two forms:
- Asymptomatic - there are no symptoms of the disease, the diagnosis can be made when antibodies to the parainfluenza virus increase in the results of 4 or more tests.
- Erased - expressed by mild catarrhal manifestations, absence of temperature and symptoms of intoxication.
Attention! Atypical forms are typical for re-infection of adults and older children.
Depending on the severity of the flow, three forms are distinguished:
- Mild - mild catarrhal symptoms, slight discharge of exudate from the nose, light, dry cough, quickly wet cough.
- Moderate - moderately pronounced signs of intoxication and catarrhal manifestations. Body temperature in adults rises to 38°C, in children up to 39°C.
- Severe – high body temperature up to 39-40°C, headaches, nausea, severe weakness. Sometimes meningal or encephalitic syndrome occurs, the lower respiratory organs are affected, and respiratory toxicosis appears. Severe cases are extremely rare.
By nature, parainfluenza is divided into smooth and non-smooth. With non-smooth parainfluenza, bacterial pathogens join the viral microflora, complications develop or existing chronic diseases worsen.
The danger of parainfluenza
For most people, the symptoms of infection are mild, the disease causes only mild discomfort, but the body copes with the infection on its own. Parainfluenza is dangerous for newborns and the elderly, as there is a risk of complications.
Young children are at risk of developing croup due to swelling of the laryngeal mucosa. This complication develops suddenly, manifests itself as a coughing attack, the child behaves restlessly, he is frightened, cyanosis, tachycardia, and difficulty breathing appear.
Choosing the right treatment for people at risk guarantees a full recovery without consequences.
Pathogenesis and pathomorphology
Viral particles spread through airborne droplets. Together with the air flow, particles of saliva and dust, they penetrate the respiratory tract and settle on the mucous epithelium. Due to their large size, parainfluenza viruses are often localized in the nasopharynx, rarely penetrating down the respiratory tract.
Having established itself in the mucous epithelium, the viral microflora multiplies, causing inflammation and cell degeneration. When the affected cells are destroyed, the parainfluenza virus penetrates the bloodstream and lymphatic system, affects nerve endings and causes symptoms of intoxication.
The inflammatory process can affect the larynx, trachea and lower respiratory organs. According to pathomorphological characteristics, parainfluenza is expressed in the form of laryngitis, tracheitis, laryngotracheitis, tracheobronchitis.
When the body weakens, the body’s own pathogenic microflora is activated or a secondary infection occurs. Under the influence of bacterial pathogens, there is a significant deterioration in the patient’s condition and the development of complications.
On days 7-10 of the disease, the immune system begins to produce immune bodies that suppress the activity of pathogenic microflora. The effect of antibodies is short-lived and does not provide long-term protection against re-infection. Therefore, during one autumn-winter period, a person can get parainfluenza several times, primarily this applies to children attending preschool educational institutions.
Pathogenesis of parainfluenza
Reproduction of the parainfluenza virus occurs in the cytoplasm of columnar epithelial cells of the respiratory tract, causing their destruction. Damage to the mucous membrane of the larynx is typical - swelling and edema .
The narrowing of the lumen of the larynx is caused by swelling of the mucous membrane, inflammatory cell infiltration, hypersecretion of the mucous glands and accumulation of exudate. The nature of the inflammation can be catarrhal, catarrhal-purulent, fibrinous-purulent and ulcerative-necrotic.
The resulting obstruction results in hypoxia, hypercapnia, and in severe cases, asphyxia. Metabolic disorders and the threat of cerebral edema develop.
Incubation period
From the moment viral particles enter the body, a hidden period of their reproduction and damage to the cells of the mucous epithelium of the respiratory tract begins. Parainfluenza is characterized by slow spread and penetration into the systemic bloodstream and lymph.
From the moment of infection, the first symptoms appear after 2-7 days, depending on the state of the body’s defenses. Most often, the first signs appear on day 4, but the patient becomes infectious on the first day before clinical manifestations.
How to treat parainfluenza
Therapy for parainfluenza is usually symptomatic; there is no specific treatment. The main task of the doctor and the patient is to strengthen the body so that it can independently fight the virus.
Symptomatic treatment is carried out with medications and traditional methods of treatment. Nasal drops, antipyretics, throat pain relievers, antitussives and expectorants are prescribed.
The following drugs are prescribed for the treatment of parainfluenza:
- Arbidol - allowed for children from 2 years old to take 2 tablets before meals, from 6 years old 4 tablets are recommended, from 12 years old - 8 tablets, the course of therapy is 5 days;
- Oxolinic ointment is prescribed to lubricate the nasal mucosa; it should be applied up to 4 times a day;
- Lokferon is a rectal suppository that is indicated for children for the treatment of inflammatory diseases;
- Isoprinosine - prescribed 3 times a day, course of treatment - 10 days;
- Ribavirin – indicated from 12 years of age, the course of treatment lasts 5 days.
Immunomodulators are required to suppress the virus and stimulate the immune system. Representatives: Viferon and Interferon.
In severe cases of the disease, treatment of parainfluenza is supplemented with the following medications:
- to reduce body temperature - Nurofen, Ibuprofen;
- for severe coughs, expectorants are prescribed - Mucaltin, Lazolvan;
- for nasal congestion and runny nose, saline solutions are indicated;
- to relieve inflammation of the respiratory tract - Erespal.
If therapy is ineffective, antibacterial drugs may be prescribed.
Temperature
Parainfluenza differs from other viral infections by a rare increase in body temperature above subfebrile levels. If the patient’s immunity is strong and there are no complications, the temperature stays within 37-37.5°C.
When the body's defenses weaken, in adults the temperature rises to 38°C; in children it can rise higher, but rarely rises above 39°C. Higher rates may indicate the presence of complications or an incorrect diagnosis that requires additional diagnostics.
Classification of croup syndrome
Degree of laryngeal stenosis Diagnostic criteria I degree (compensated stage) Hoarseness of voice, dry “barking” cough. Difficulty breathing when inhaling, retraction of the jugular fossa increases with anxiety or physical exertion. There is no cyanosis. There is no hypoxemia or it is insignificant (paO2 >70 mm Hg). There is no hypercapnia. Duration of stenosis - from several hours to 1–2 days I degree (subcompensated stenosis, stage of incomplete compensation) Breathing is noisy with the participation of auxiliary muscles in the act of breathing. Anxiety. Perioral cyanosis. Hypoxemia (paO2 less than 70 mm Hg). There is no hypercapnia. The symptoms of laryngeal stenosis persist for up to 3–4 days. III degree (decompensated stage) Breathing is noisy with a sharp retraction of all compliant places of the chest, retraction of the lower end of the sternum. Reduced breathing sounds in the lungs. Paradoxical pulse. Lip cyanosis, acrocyanosis. Concern expressed. Hypoxemia (paO2 less than 60 mm Hg). Hypercapnia (paO2 >45 mm Hg). Combined or only respiratory acidosis IV degree (asphyxia, terminal stage) Severe signs of respiratory failure. Breathing is shallow with irregular rhythm. General cyanosis. Phenomena of capillary stasis. Body temperature drops to normal or subnormal values. Breathing in the lungs is barely audible. Tendency towards bradycardia. Coma. Hypoxemia (paO2 less than 50 mmHg). Hypercapnia (paO2 more than 70 mm Hg)In adults, the course of the disease is usually favorable. Protracted bronchitis, especially in the presence of mucopurulent sputum, is associated with the addition of a secondary bacterial infection.
Pneumonia is a common and serious complication. When it occurs early, it is characterized by severe toxicosis and often a severe course.
Symptoms of the disease in adults
After the end of the incubation period, the patient develops symptoms resembling a cold. A sore throat, nasal congestion, and dry cough are the first symptoms of parainfluenza in adults.
The further course of the disease depends on the functioning of the immune system. In some cases, parainfluenza occurs without intoxication or increased body temperature.
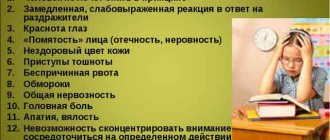
But there are symptoms of parainfluenza that are characteristic of most patients:
- temperature 37.5-38°C;
- fever and chills, when the temperature rises above 38°C;
- nasal congestion, exudative discharge;
- sore and sore throat;
- hoarse voice;
- dry, barking cough;
- weakness, malaise.
If a bacterial infection occurs, the cough becomes productive. Purulent sputum begins to come out when you cough. In patients with chronic diseases of the respiratory system, inflammation can spread to the lungs and bronchi.
Symptoms and manifestations of parainfluenza in children and adults
Diagnosis of parainfluenza
In most cases, the treating physician will not be concerned about whether the patient has HPIV. This is due to the fact that completely healthy people cope with this virus without additional treatment, so there is no need for an accurate diagnosis. However, if you have a weakened immune system, your doctor may want to check whether you have parainfluenza and what type it is to avoid serious complications such as bronchitis or pneumonia.
Most likely, your doctor can do a simple test to determine if your symptoms match those of parainfluenza. For a more accurate diagnosis, the doctor may take a swab from the throat or nose to determine the presence of the virus, particularly in the cell structure. A doctor can also determine the presence of the virus by detecting antibodies that the body produces to fight the virus.
On examination, the nasal mucosa is hyperemic and swollen. The soft palate and posterior wall of the pharynx are clearly hyperemic. Some patients experience fine granularity of the soft palate and slight swelling of the pharyngeal mucosa. There is an increase in heart rate and a corresponding increase in body temperature; in severe cases of the disease, there is a muffled heart sound.
Normocytosis or moderate leukopenia is detected in the blood. During the period of convalescence, monocytosis is possible; ESR is within normal limits.
To determine the extent of parainfluenza symptoms and determine whether complications such as pneumonia are present, your doctor may order a chest X-ray or CT scan of the chest. Both methods help doctors see exactly what is happening inside the patient's chest.
Features of the disease in children
Symptoms of parainfluenza in children can develop gradually or rapidly progress, causing acute manifestations. If the child’s immunity is strong enough, then the disease proceeds like a regular respiratory infection, lasting no more than a week.
But most children experience acute symptoms:
- low-grade or febrile temperature;
- nasal congestion;
- mucous or purulent mucous discharge from the nose;
- severe swelling and redness of the larynx;
- hoarseness of voice;
- dry, hacking cough;
- tonsil hypertrophy;
- weakness, loss of appetite.
Parainfluenza in children is often accompanied by laryngitis or tracheitis. The development of complications in the form of false croup is typical. Due to the narrowing of the larynx and severe swelling, attacks of suffocation may occur, requiring urgent medical attention.
When a bacterial infection occurs, the child’s body temperature rapidly rises, fever develops, and pronounced signs of toxic poisoning appear. Particular attention should be paid if a severe cough appears, accompanied by purulent sputum and chest pain - these signs indicate the development of pneumonia.
In infants, parainfluenza develops rapidly - from the first signs to recovery it takes about a week. Already on the first day of illness, all the symptoms of the disease may appear - profuse nasal discharge, cough, hoarseness.
Against the background of parainfluenza, infants become capricious, weak, and refuse to breastfeed. High body temperature and intoxication are not typical for children in the first year of life, as are complications in the form of false croup or damage to the respiratory tract.
Acute laryngotracheitis
A complication of parainfluenza in children is laryngeal stenosis in acute laryngotracheitis, also called “false croup”. Predisposing factors of development are anatomical and physiological features, among which are:
- narrowness of the lumen of the larynx, pliability of cartilage;
- an abundance of vessels in the mucous membrane of the larynx;
- narrowness and curvature of the epiglottis, short vocal cords;
- tendency to increased neuro-reflex excitability.
In the pathogenesis of acute laryngotracheitis, several factors are important: swelling of the laryngeal mucosa, muscle spasm and accumulation of inflammatory exudate - this leads to cough, aggravating spasm and stenosis.
To compensate for the lack of oxygen, breathing becomes more frequent, including through the mouth - the incoming air is heated and not sufficiently humidified. The viscosity of the accumulated mucus increases and it is difficult to separate. Loss of voice (aphonia). The patient's condition worsens - at first pale skin, sweating and anxiety appear; in the absence of help, the skin becomes cyanotic and later gray, excitement gives way to apathy, loss of consciousness, and areflexia.
The initial manifestations of laryngeal stenosis in the compensation stage are characterized by the absence of pronounced disturbances in the general condition, preservation of the pale pink color of the skin, slowing and deepening of breathing, shortness of breath during physical exertion, and fear. Symptoms usually appear at night. The main signs are a rough cough, hoarseness and difficulty breathing.
At the stage of partial compensation, tachypnea (rapid breathing) appears. The intercostal spaces and the fossa above and below the collarbone are retracted. The skin turns pale, the child is excited. Shortness of breath is noticeable even in a calm state and is manifested by noisy breathing that can be heard from a distance.
Breathing in the stage of decompensation slows down and becomes less noisy than before - this is an unfavorable prognostic sign. The skin acquires a bluish tint, sweating, and a forced position in bed with the head thrown back are also characteristic.
The terminal stage, or the stage of asphyxia, is characterized by the presence of single, superficial and intermittent respiratory movements. Noisy breathing completely disappears. Involuntary urination and defecation may occur. The color of the skin is pale gray, the pulse is barely palpable. Blood pressure decreases, cardiac arrest occurs.
Diagnostics
Diagnosis of parainfluenza is based on the results of a visual examination and patient complaints. The doctor pays attention to the condition of the larynx, the nature of catarrhal manifestations and the severity of intoxication. The presence of croup syndrome in children almost always indicates damage to the larynx by parainfluenza viruses.
Diagnosis may be based on laboratory blood tests. The most sensitive enzyme immunoassay is considered to be able to determine the levels of immunoglobulins and the stage of the disease. Enzyme immunoassay diagnostics are express methods and allow you to get results in a few minutes.
It is very important to promptly differentiate the appearance of influenza, parainfluenza and adenovirus infection. While patients with parainfluenza and adenovirus infection do not always require special treatment, influenza requires careful therapy aimed at suppressing viruses and preventing complications. Therefore, a smear is taken from the larynx to identify the causative agent of the disease.
How dangerous is parainfluenza?
For most people, HPIV goes away relatively smoothly. The symptoms may cause serious discomfort for a few days, however, you can only cope with the infection on your own if your immune system is functioning correctly.
Newborns, young children and the elderly, whose immune systems are weakened, are most at risk of parainfluenza infection and complications, so these categories of the population should definitely be examined by a doctor and receive clear instructions for effective treatment of the disease. However, with proper treatment, even such people recover quickly and completely.
Treatment of parainfluenza in children and adults
Treatment of parainfluenza in adults and children is carried out at home and requires hospitalization only in the presence of severe complications. For treatment to be effective, you need to adhere to certain rules of therapy.
Even with a mild course of the disease, bed rest is required to reduce the risk of complications. All patients, regardless of age and clinical manifestations, need plenty of fluids, regular ventilation and a nutritious diet rich in vitamins and proteins.
To ease general well-being and restore breathing, rinsing the nose with salt water and instilling vasoconstrictor drops - Vibrocil, Tizin, Nazivin, Xymelin - are prescribed. Gargling is prescribed to all patients from 4-5 years of age.
The most effective are:
- Saline solutions.
- Tinctures of eucalyptus, propolis, calendula.
- Miramistin.
- Rotokan.
There are no special drugs for parainfluenza, therefore both adults and children are prescribed drugs related to broad-spectrum antiviral drugs with immunostimulating properties:
- Viferon.
- Amiksin.
- Cytovir-3.
- Interferon.
- Kagocel.
- Anaferon.
Medicines such as ACC, Mucaltin, Codelac, Broncholitin will help you cope with cough. Prevents spasms of the bronchi and larynx, has an antispasmodic effect and a powerful anti-inflammatory effect Erespal.
For high fever the following is prescribed:
- Paracetamol (Panadol).
- Ibuprofen (Nurofen, Ibuklin).
Treatment of parainfluenza in children is often carried out using inhalations with mucolytic and antiseptic solutions. Ambrobene, Lazolvan, Fluimucil are prescribed for cough, alkaline mineral water and saline solution to soften the mucous membrane, and Miramistin, calendula tincture, Rotokan to relieve inflammation.
If a bacterial infection is associated with parainfluenza, broad-spectrum antibiotics are prescribed: Amoxicillin, Sumamed, Amoxiclav, Suprax, Augmentin. For inhalation, use Fluimucil AT, Gentamicin or Dioxidin to reduce the negative impact of drugs on the gastrointestinal tract. For severe swelling and laryngospasms, glucocorticosteroids are prescribed in injections or tablets: Prednisolone, Dexamethasone. Children often use inhalations with Dexamethosone or nasal sprays Nasonex, Momat Rino.
Treatment
Etiotropic treatment - antiviral:
- “Kagocel” is an antiviral agent whose action is aimed at stimulating the body’s production of the interferon protein and destroying viruses. This is a safe drug approved for children over 3 years of age.
- "Remantadine" - destroys viruses, stimulates the immune system, reduces symptoms of intoxication. The disadvantages of the drug are its selective action and the possibility of developing side effects.
- "Amiksin" is the basis for the treatment and prevention of viral infections.
Immunomodulators and immunostimulants:
- Suppositories “Viferon”, “Kipferon”.
- Nasal drops “Grippferon”, “Interferon”.
- Syrup for children “Tsitovir”, “Orvirem”.
- Tablets "Cycloferon", "Anaferon", "Ergoferon".
Symptomatic treatment of parainfluenza:
- Antipyretics based on paracetamol or ibuprofen,
- For dry cough, “Sinekod”, “Stoptusin”, “Gidelix” are prescribed.
- If the cough has become wet, expectorants and mucolytics “Lazolvan”, “ACC”,
- "Erespal" is an anti-inflammatory drug widely used to treat the respiratory system,
- Rinsing the nose with saline or AquaMaris, removing swelling with Xilen or Tizin
If complications occur, patients are prescribed:
- Antibacterial drugs,
- Sulfonamides,
- Hot foot baths,
- Steam inhalations,
- Corticosteroids.
ethnoscience
Antiviral herbal remedies include: chamomile, St. John's wort, calendula, sage, eucalyptus, onion and garlic, raspberries, pomegranate. Raspberry, linden, coltsfoot have a diaphoretic effect; expectorant - licorice, marshmallow.
Patients with parainfluenza are recommended to drink tea with raspberries, thyme, a decoction of blackberry leaves, rose hips, chamomile, linden tea, carrot juice, cranberry juice, sea buckthorn juice, and an aloe decoction with honey.
Complications of parainfluenza, what are they?
Parainfluenza in adults rarely causes complications, since the immune system of adults is able to suppress the reproduction of viruses. The child’s body is most predisposed to the spread of inflammation to the lower respiratory organs and the addition of a bacterial infection.
Complications of parainfluenza:
- Sinusitis.
- Adenoiditis.
- Bronchiolitis.
- Pneumonia.
- Otitis.
- Meningitis.
The most severe consequence of parainfluenza in children is false croup, which is expressed by attacks of suffocation. Depending on the degree of stenosis, various symptoms appear and the most severe are characteristic of the last stage - convulsions, confusion, heart failure, decreased blood pressure. Children with croup may develop severe asphyxia, which can be fatal.
Pathogenesis
After adsorption on epithelial cells, the virus enters the cells and multiplies, leading to their death. Intoxication is caused by the penetration of reproduced viruses and decay products of epithelial cells into the blood. The key points of pathogenesis are:
- dystrophic changes and necrosis of ciliated epithelial cells;
- loss of the mucous membrane's protective barrier;
- viremia and intoxication.
Primary viral pneumonia is caused directly by the causative agent of parainfluenza. It is called secondary when a microbial infection is attached. The settling of immune complexes in the capillaries provokes immunopathological reactions, and inflammation and swelling of the laryngeal mucosa cause symptoms of stenosis in parainfluenza in children.
Prevention of parainfluenza, what is it?
Parainfluenza, the symptoms and treatment of which depend on the patient’s age and the characteristics of his immune system, requires compliance with the rules of prevention to protect against infection. First of all, this is the absence of contact with sick people and wearing a mask during epidemics of respiratory infections. It is imperative to observe general rules of hygiene and carry out hardening procedures that strengthen the body's defenses.
There is no vaccine against parainfluenza for humans. Antibodies produced upon contact with viral particles disappear very quickly, and lasting immunity is not formed. Therefore, if there were vaccines against parainfluenza, they would have short-term effectiveness.
Clinic
The incubation period of the disease lasts from 2 to 7 days.
Unlike influenza, parainfluenza begins gradually. The patient complains of malaise, headache (usually in the forehead or temporal areas), and sometimes pain in the eyes. Then chilling and moderate myalgia appear.
The temperature rarely exceeds 38 °C. A rough “barking” cough is characteristic, which appears from the 1st day of illness. Nasal breathing may be impaired, swelling of the nasal mucosa and runny nose may appear.
Objectively : the pharynx is hyperemic and swollen. Fine granularity of the soft palate may be noted.
Treatment of ARVI during the COVID-19 epidemic
Intoxication is mild, changes in internal organs are practically absent. Sometimes you can listen to muffled heart sounds, moderate tachycardia, corresponding to the temperature level.
In young children, the process quickly progresses to the bronchi and alveoli, leading to bronchitis and bronchiolitis.
Diagnosis is based on clinical examination data.
For rapid diagnosis, the immunofluorescence method is used.
Serodiagnosis includes RSC and RTGA.
Diagnosis of a viral disease
To diagnose a patient, the doctor will need to carefully study the characteristics of the disease. The main signs confirming the presence of the virus will be a sharp deterioration in the patient’s well-being, inflammatory processes in the area of the vocal cords, leading to the development of a hacking cough, and swelling in the upper respiratory tract. At the age of less than 3 years, parainfluenza is indicated by symptoms of croup.
To finally confirm the diagnosis, a laboratory study of the patient’s biomaterial is performed.
If parainfluenza causes complications, the basic diagnosis is supplemented by serological and enzyme-linked immunosorbent blood tests, immunofluorescence, and radiography of the sternum. A detailed examination helps differentiate the disease from similar pathologies (adenovirus). Characteristic features of the latter virus are the development of severe intoxication, conjunctivitis, swelling of the lymph nodes, digestive disorders, and puffiness of the face.
Parainfluenza can also be distinguished from similar diseases by the presence of moderate intoxication and a dry, rough cough. The disease is characterized by the absence of myalgia (muscle pain), atralgia (joint pain), enlargement of the liver or spleen. The appearance of the patient often does not differ from that in a healthy state.
Forecast and preventive measures
Parainfluenza is not one of the diseases with a negative prognosis. If therapy is started in a timely manner and all doctor’s recommendations are followed, recovery occurs quickly and there are no complications.
Prevention of parainfluenza in the form of vaccination is not provided. To prevent infection with the virus and the subsequent development of the disease, it is recommended:
- Avoid any contact with a person who has been confirmed to have the infection.
- Ventilate the room frequently.
- Wash your hands regularly with soap (preferably laundry soap).
- Every day at least 20-30 minutes. be in the fresh air.
- Monitor your diet and include a sufficient amount of fortified foods (the most important thing is the presence of vitamin C in food).
- Practice proper hardening and moderate exercise.
- Get enough sleep and rest after intense work.
During seasonal activation of viruses, it is recommended to use medical masks and take immunostimulants (to choose the right drug, you should consult an immunologist or therapist). It is important to avoid long stays in crowded places. After returning from the street, it is recommended to wash with warm water and soap (this helps remove pathogens from the skin and mucous membranes).
From 2 years of age, Oxolinic ointment can be used - an antiviral agent intended for treating the nasal passages. To destroy the viruses that cause parainfluenza, it is recommended to use portable quartz lamps. Home air humidifiers are also useful, helping to avoid drying out of the mucous membranes and exposure to infectious agents.
Video on the topic:
Consultation with a doctor about parainfluenza
Question: Why is there no vaccine against parainfluenza infection? Answer: there is, but it is not advisable, because it causes an increase in specific antibodies in the blood, and the site of entry of the pathogen remains untouched (i.e., into the nasal mucosa) and the virus easily penetrates further throughout the body, causing moderate intoxication. In case of prevention, it is more advisable to use local antiviral ointments (Oxolinic) before visiting public places.
General practitioner Shabanova I.E.
Parainfluenza is an acute pathology of viral etiology that affects the respiratory organs - the nose and larynx, manifested by catarrhal and intoxication symptoms.
In 1952, Japanese scientists discovered a virus that was similar in morphological and physiological properties to the influenza virus and was called parainfluenza.
Traditional medicine against parainfluenza viruses
Folk remedies for parainfluenza will help support the body while fighting the virus and speed up recovery. The use of alternative medicine recipes should be considered as a supplement to the main course of medication.
Parainfluenza therapy is carried out using:
- raspberries;
- aloe with honey;
- sea buckthorn;
- clover tinctures;
- linden color.
Recipe with raspberries
Dried berries are poured with boiling water and left for 15 minutes. The finished drink is taken before bed (adults - 1 glass, children - half as much).
Aloe+honey
You need to combine crushed aloe leaf, ½ cup of liquid honey, 200 ml of non-hot boiled water. The finished mixture must be simmered over low heat for half an hour, and taken strained, 1 tbsp. l. three times a day.
Sea buckthorn drink for parainfluenza
Fresh sea buckthorn berries (1 kg) are crushed using a meat grinder or blender, and the juice is squeezed out. The product is drunk daily, in small portions. The course of therapy is until the condition improves.
Clover tincture against viruses
To prepare such a “medicine”, several flowers of the plant (at least 7 pieces) are poured with a glass of just boiled water and left for half an hour. After straining, a small amount of honey is added to the composition. The finished product is drunk twice within 24 hours, in the amount of 1 glass.
Lime blossom product
3 tbsp. l. vegetable raw materials are poured with boiled water and placed in a water bath for 15 minutes. Next, the composition is kept for 1 hour, filtered, diluted with boiled water to obtain a volume of 250 ml. When affected by the parainfluenza virus, the decoction is consumed in the morning and evening, 1 glass each.
As an additional remedy for parainfluenza, it is also recommended to take tea from thyme, chamomile, St. John's wort, coltsfoot, blackberry, and calendula.
Routes of infection by paramyxoviruses
Parainfluenza tends to become active twice a year. The greatest outbreaks of morbidity are observed in autumn and spring. The main route of transmission of infection is airborne droplets.
The virus is transmitted from sick people to healthy people:
- During the process of coughing and sneezing.
- When kissing.
- During close proximity, conversation.
Infection can occur if you touch objects that contain nasopharyngeal mucus from a sick person. The virus easily enters the body of patients who do not care enough about hand hygiene, or who completely neglect it.
Despite the milder course of parainfluenza compared to influenza viruses, it should not be carried on your feet. If this rule is violated, the disease can affect the lower respiratory tract, causing bronchitis or pneumonia.