Facial neuritis is an inflammatory disease. A very common form of facial nerve damage. A separate variant of this pathology is called Bell's palsy.
The term “neuritis” itself refers to damage to the peripheral nerve. In this case, both the myelin sheath (an electrically insulating sheath to exclude external influences from other nerve signals) and the axial cylinder (folds containing the processes of nerve cells) are damaged.
Damage leads to paralysis of all facial muscles. Typically, the nerves on one side of the face are damaged (unilateral neuritis). But this is enough for a person to be unable to close his eye (this is lagophthalmos, or otherwise hare’s eye), wrinkle his forehead, or bare his teeth.
But not only external inconvenience arises - food begins to get stuck between the cheek and gum, troubles arise with the eye of the damaged side of the face (they are called Bell's symptom).
But that's not all. Sensory (gustatory) and parasympathetic (secretory) fibers pass through the trunk of the facial nerve. Inflammation will affect them too. As a result, taste sensitivity on the affected side may be severely affected.
What is facial neuritis
Facial neuritis is an inflammatory disease that affects the 7th pair of cranial nerves (cranial nerves).
For reference. The facial nerve is responsible for the innervation of the facial muscles, therefore, when it is inflamed, facial expressions are disrupted (the patient cannot smile or frown), facial asymmetry develops, and the process of chewing food becomes significantly more difficult or impossible.
Damage to the facial nerve is most often unilateral, but two percent of patients may have a bilateral form of the disease.
Facial neuritis is characterized by a long course. Treatment in a hospital takes on average 20 to 30 days. However, complete recovery may take from 3 to 6 months.
In approximately five percent of patients, the work of the facial muscles is not fully restored (as a rule, the risk group includes patients with head injuries and tumors affecting the brain).
In 10% of patients who have suffered facial neuritis, relapses of the disease are observed.
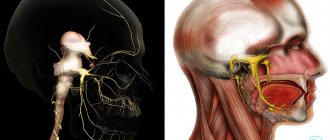
What is the facial nerve
The facial nerve is the 7th nerve of 12 pairs of the cranial nerve. The facial nerve (FN) exits the brain in the area between the pons and the medulla oblongata. This is a motor nerve, its main function is to innervate the facial muscles.
However, due to the fact that it includes PN fibers (the intermediate nerve responsible for the innervation of the lacrimal gland and providing taste sensitivity to the anterior 2/3 of the tongue), the facial nerve acquires a mixed (motor-sensitive) character.
For reference. Quite frequent neuritis of the facial nerve is facilitated by the fact that along its length the facial nerve passes through many narrow bone canals.
Therefore, even with slight inflammation or poor circulation in the surrounding tissues, when the nerve fibers swell, they are compressed and pinched in narrow bone canals.
In the absence of timely medical care, irreversible damage to the cells and fibers of the FN occurs.
Functions
The nervus facialis innervates the muscles that are responsible for facial expression. It is also responsible for transmitting a signal to the brain when the tongue comes into contact with salty, sour, sweet, etc. The facial nerve ending performs a parasympathetic function, i.e. provides connection between parts of the head and neck with the CNS (central nervous system). Provide a response to external factors of the following glands:
- salivary;
- lacrimal;
- responsible for the production of mucus in the pharynx, palate, and nose.
Causes of inflammation of the facial nerve
Neuritis of the facial nerve is a fairly common pathology.
For reference. The disease occurs with equal frequency in both men and women. More often, FN lesions are recorded in the cold season. The maximum number of patients occurs in regions with a cool and damp climate.
The main causes of the disease include:
- hypothermia (exposure to a draft or air conditioner on the neck and ear area leads to spasm of muscles and blood vessels, blood supply is disrupted, nerve inflammation occurs, and general hypothermia is observed, which contributes to a decrease in immunity);
- alcohol abuse (alcohol intoxication can cause damage to nerve fibers and lead to the development of neuritis);
- uncontrolled forms of arterial hypertension (against the background of increased intracranial pressure, damage to the nucleus of the facial nerve is possible);
- herpes viruses (especially with herpes zoster, which affects the trigeminal nerve, in which case inflammation may spread to the fibers of the facial nerve);
- mumps viruses, enteroviral and adenoviral infections, polio pathogens, past sinusitis, otitis, odontogenic infections;
- poor quality dental treatment;
- pregnancy (against the background of changes in hormonal levels, when combined with other risk factors in the first trimester, inflammation of the FN fibers may develop);
- diabetes mellitus, accompanied by damage to blood vessels and nerve fibers;
- pronounced forms of atherosclerosis of cerebral vessels and neck vessels, as well as multiple sclerosis , which is accompanied by autoimmune damage to the myelin sheaths in nerve fibers.
Pathogenesis
The triggering factor for FLN is irritation of the vessels of the craniocervical region, which contributes to the development of vasospasm of the vertebral and branches of the external carotid artery, which leads to primary ischemia of the FLN root. Increasing disturbances of microcirculation in the structures of the FN lead to anoxic swelling of the nerve . This, in turn, leads to compression (squeezing) of the nervous tissue in the facial (fallopian) canal of the temporal bone, disruption of neuromuscular conduction caused by blockade of the process of release of acetylcholine and a disorder in the interaction of acetylcholine with receptors located on the postsynaptic membrane. As disorders increase in the nervous tissue, secondary ischemia of the FN develops.
Classification
All forms of neuritis of the facial nerve are divided into:
- primary - cold inflammation of the facial nerve (develops against the background of hypothermia);
- secondary - occur against the background of concomitant pathologies (herpes infections, mumps, otitis, odontogenic infections, traumatic brain injuries accompanied by damage to the facial nerve).
For reference. There is also a separate variant of facial neuritis - Bell's palsy. The exact causes of the disease are unknown. Paralysis is seasonal and develops mainly against the background of hypothermia.
Symptoms of the disease
The disease usually develops gradually. The first symptom is a dull, aching pain behind the ear. Less commonly, the pain can be acute.
After a few days, visible facial asymmetry appears. Sometimes symptoms develop faster (a person goes to bed healthy and wakes up with visible facial asymmetry).
On the affected side of the FN it is noted:
- smoothing the nasolabial fold;
- drooping of half the face (eyebrow, corner of the eye and mouth drooping);
- “distortion” of the face.
The patient cannot smile normally (the smile appears asymmetrical), frown his eyebrows, stretch out his lips or show his teeth.
Often, a patient with neuritis of the facial nerve cannot completely close the eye (due to this, drying of the conjunctiva and cornea is noted). When you try to close the eyelids, the eye turns upward (the so-called Bell sign).
Against the background of a slightly open eyelid, the development of lagophthalmos (“hare’s eye”) is observed - a white strip of sclera is constantly visible between the iris and the lower eyelid. Due to the inability to close the eye, constant lacrimation is noted (the patient cries “crocodile tears”). Lacrimation increases sharply during meals.
Also, many patients are concerned about a sharp decrease in the taste sensitivity of the tongue, pain in the jaw and behind the ear.
Increased salivation may occur. Due to the inability to close the mouth normally, there is a constant flow of saliva from the mouth.
Less common is a decrease in the secretion of tears and saliva. Also, some patients have difficulty chewing.
For reference. A common manifestation of the disease is hyperacusis on the side of the nerve inflammation (excessively increased sensitivity to sounds).
Symptoms of secondary neuritis of the facial nerve
With poliomyelitis damage to the nucleus of the FN, severe weakness of the facial muscles is noted.
For reference. Against the background of strokes accompanied by damage to the roots of the FN, as well as the nuclei of the FN and the abducens nerve, the development of convergent strabismus, paresis of the facial muscles and visible asymmetry of the face is noted.
With neuromas, the auditory nerve is also affected, so facial asymmetry is combined with hearing loss and tinnitus .
Against the background of herpetic nerve lesions, severe cutting or burning pain in the ear is noted. Pain may radiate to the face, upper neck and occipital region.
It is also typical for a specific herpes rash to appear on the skin of the auricle, external auditory canal, eyelid skin, lips, as well as mucous membranes lining the pharynx, larynx and tongue.
For reference. Some patients may experience complaints of tinnitus, hearing loss, and constant dizziness . Sometimes there is horizontal nystagmus (fast rhythmic movements of the eyeballs from side to side).
Against the background of mumps (mumps), neuritis develops against the background of general intoxication symptoms and fever. The patient is worried about muscle and joint pain, nausea, weakness, headaches . The appearance of unilateral mumps-specific swelling is also characteristic.
With the development of inflammation of the FN against the background of complicated otitis, facial asymmetry is combined with elevated body temperature and shooting pain in the ear. Trismus (spasm) of the masticatory muscles may also develop.
Why is facial neuritis dangerous?
In any case, inflammation of the nerve leads to the death of some nerve fibers. But the innervation does not completely disappear. The need to control more muscles with less nerve fiber leads to an unpleasant situation called synkinesis.
In fact, synkinesis leads to reflexive conjugal muscle movement. For example, when you blink, the corner of your mouth will rise. Not a very pleasant impression from the outside.
Disruption of the innervation of some small facial muscles can lead to their atrophy. Part of the face will be motionless, which is completely unnecessary.
Due to impaired drooping of the eyelid and constant dryness of the conjunctiva, the development of conjunctivitis, keratitis, and corneal ulcers is possible.
Also, in the absence of timely treatment, inflammation of the FN can be complicated by unilateral contracture of the facial muscles.
For reference. In the vast majority of cases, the mobility of facial muscles is completely restored within 3-6 months with proper treatment and care.
Course and prognosis
The prognosis of this disease in most patients is favorable - complete recovery is observed in 75% of patients. If facial muscle paralysis persists for more than 3 months, the patient's chances of a full recovery rapidly decrease.
If neuritis is caused by injury or disease of the hearing organ, restoration of normal muscle function may not occur at all. As for recurrent neuritis, each subsequent episode of the disease is somewhat more severe than the previous one, and the recovery period lengthens.
Optic neuritis Trigeminal neuralgia Optic nerve atrophy Glaucoma Conjunctivitis Eye keratitis: photos, symptoms and treatment
Diagnosis of the disease
If you suspect neuritis of the facial nerve, an examination by a neurologist is required. Moreover, if the disease began with the appearance of sharp facial asymmetry, then first of all it is necessary to exclude stroke and transient cerebrovascular accident.
In particular, if the patient has symptoms uncharacteristic for neuritis of the facial nerve (loss of consciousness, speech impairment, lethargy).
In the classic course of the disease, making a diagnosis is usually not difficult.
For reference. To clarify the cause of the development of the disease, MRI or CT of the brain, electroneurography, electromyography, and examination for viral infections can be performed.
Treatment of neuritis of the facial nerve
All drugs for the treatment of facial neuritis should be prescribed exclusively by a neurologist. Self-treatment is unacceptable and can lead to the development of severe complications.
At the initial stage of the disease, it is recommended to use:
- glucocorticosteroids (prednisolone drugs relieve swelling and reduce the severity of the inflammatory reaction);
- decongestants (diuretics: furosemide, spirolactone);
- vasodilating drugs (nicotinic acid, nicotinate, scopolamine, xanthinol);
- B vitamins.
In the case of the development of secondary neuritis, treatment of the underlying disease that caused inflammation of the facial nerve is also carried out.
To speed up the recovery of facial muscles, complete rest is indicated for the first 7-10 days of illness. From the first days of illness it is allowed to use non-contact heat (sollux).
To prevent the development of conjunctivitis, keratitis and corneal ulcers, artificial tear preparations, as well as moisturizing eye ointments, are used. At night, the eye must be covered with a bandage.
The use of UHF, as well as contact heat (paraffin therapy) is allowed only from 5-6 days.
All physiotherapy procedures are prescribed in courses.
From the second week of illness, massage and exercise therapy can be used carefully. In this case, the load on the muscles should be increased gradually.
For reference. In order to accelerate the restoration of full muscle innervation, from the 14th-15th day of illness, anticholinesterase drugs (neostigmine, galantamine), as well as bendazole, can be used.
According to indications, ultrasound and hydrocortisone administration using phonophoresis are used. Methandienone preparations can also be used to accelerate metabolic processes in nerve tissues.
In rare cases, the use of electrical neurostimulation is indicated.
If there are no signs of FN recovery within 2-3 months, hyaluronidase drugs are prescribed.
Is it possible to use surgery?
Previously, surgery aimed at decompressing the nerve by widening the bone canal was widely used.
Attention. However, this technique can cause nerve damage and hearing loss. In this regard, this technique is not recommended.
Surgery is indicated only if:
- nerve rupture due to trauma (nerve suturing);
- lack of effect from conservative treatment methods for 8-10 months (nerve plastic surgery using autotransplantation is indicated).
Traditional methods
At home, you can try folk remedies as auxiliaries if you are treating with medication a nerve that has caught a cold:
- Warm the sore spots with 200 g of hot salt or sand. To do this, heat the substance in a frying pan without oil, place it in a fabric bag and keep it on the affected areas for at least half an hour;
- Drink chamomile tea and make compresses from the remaining tea bags;
- Drink rose petal tea. 3 tbsp. dry matter, pour a glass of boiling water, let the tea brew and take a glass three times a day for a month;
- Prepare a healing ointment from black poplar buds. You will need 2 tbsp. dry or fresh substance and the same amount of butter. Mix the ingredients and apply the resulting ointment to sore areas after warming with salt once a day. The duration of therapy is a month.