Agalates is a dopaminomimetic - a drug that excites dopamine receptors or promotes the accumulation of dopamine in synapses (increasing synthesis or preventing its destruction).
Description and application:
- Tradename
- International nonproprietary name
- Dosage form and description
- Composition and release form
- Pharmacological group
- Pharmacological properties
- Pharmacodynamics
- Pharmacokinetics
- Indications for use
- Contraindications
- Directions for use and doses
- Adults
- To suppress lactation
- Use in patients with impaired liver or kidney function
- Use in the elderly
- Side effect
- Overdose
- Interaction with other drugs
- special instructions
- Carefully
- Use during pregnancy and lactation
- Impact on the ability to drive vehicles and other mechanical means
- Storage conditions and shelf life
- Conditions for dispensing from pharmacies
- Analogs
- Opinion survey results
If you have already taken this medicine, do not forget to share your opinion about it.
Release form, composition and packaging
The tablets are white, flat, oval, with a bevel and a score on one side, engraved “0.5” on one side of the score and “CBG” on the other.
| 1 tab. | |
| cabergoline | 500 mcg |
Excipients: lactose, L-leucine, magnesium stearate (E572).
2 pcs. — dark glass bottles (1) — cardboard packs. 8 pcs. - dark glass bottles (1) - cardboard packs.
pharmachologic effect
Dopamine receptor agonist. Cabergoline is a synthetic ergot alkaloid, an ergoline derivative, a long-acting dopamine agonist that inhibits prolactin secretion. The mechanism of action of cabergoline involves stimulation of central dopamine receptors in the hypothalamus. At doses higher than those required to suppress prolactin secretion, the drug causes a central dopaminergic effect due to stimulation of dopamine D2 receptors. The effect of the drug is dose-dependent. A decrease in prolactin levels in the blood is usually observed after 3 hours and persists for 2-3 weeks, and therefore one dose of the drug is usually sufficient to suppress milk secretion. When treating hyperprolactinemia, the content of prolactin in the blood is normalized after 2-4 weeks of using the drug in an effective dose. Normal prolactin levels may persist for several months after discontinuation of the drug.
Cabergoline has a highly selective effect and does not affect the basal secretion of other pituitary hormones and cortisol. The only pharmacodynamic effect not related to the therapeutic effect is a decrease in blood pressure. The maximum hypotensive effect usually develops 6 hours after a single dose of the drug; the degree of blood pressure reduction and the frequency of development of the hypotensive effect are dose-dependent.
Are there cheaper candidates: comparison of analogues
Dostinex is a relatively expensive medicine. Therefore, when it is necessary to quickly finish breastfeeding, not everyone will have the money to purchase this particular drug. Therefore, in addition to pills, you can also consider traditional methods of reducing lactation. For details please refer to this article. If you just need to stop the production of breast milk and do it correctly, then these options are most suitable.
Let's try to figure out how to do this without harm to health and with the help of cheap analogues of Dostinex. Analogues in Russia are presented in the following versions:
- tablets to stop lactation with a similar active ingredient (Cabergoline, Bergolak, Agalates);
- drugs with similar effects, but different in composition (in particular, Bromocriptine).
| A drug | Active substance | A course of treatment | Average price, rub. |
| BROMOCRYPTINE | bromocriptine | 2 times 0.125 mg (1/2 tablet) on the 1st day + 2 weeks 0.25 mg (1 tablet) 2 times a day | From 220 |
| BERGOLAK | cabergoline | 2 days 1 tablet 0.25 mg 2 times a day | From 270 |
| CABERGOLINE | cabergoline | 2 days 1 tablet 0.25 mg 2 times a day | From 700 |
| AGALATES | cabergoline | 2 days 1 tablet 0.25 mg 2 times a day | From 430 |
The main contraindications of Dostinex analogues:
| Contraindications | BROMOCRYPTINE | BERGOLAK | CABERGOLINE | AGALATES |
| Lactation | + | + | + | |
| Children under 16 years old | + | + | + | |
| Intolerance to the main substance of the drug | + | + | + | + |
| Unstable blood pressure | + | + | + | + |
| Liver failure | + | + | ||
| Cardiovascular diseases | + | + | + | |
| Respiratory diseases | + | + | + |
The main side effects of substitutes:
| Side effects | BROMOCRYPTINE | BERGOLAK | CABERGOLINE | AGALATES |
| Headache | + | + | + | |
| Nausea and vomiting | + | + | + | |
| Dizziness | + | + | + | |
| drowsiness | + | + | + | |
| Itching, allergic rashes | + | |||
| Constipation or diarrhea | + | + | + | |
| Arterial hypotension | + | + | ||
| Muscle cramps of the limbs | + | + | ||
| Depression or unreasonable aggression | + | |||
| Hallucinations, psychoses | + |
1 According to the instructions for use of Cabergoline, the product contains the same active ingredient as Dostinex - the main difference is only in the manufacturer and price. To prevent lactation after an abortion or unsuccessful birth, take 1 tablet 3-4 hours after surgery, and to stop it - 1 tablet 2 times a day for 2 days.
2 The instructions for use of Bergolak are similar to Dostinex and Cabergoline, since the product contains the same active ingredient. A single dose will be required to prevent lactation and a 2-day period to stop milk production.
3 According to the instructions for use, the drug Agalates has contraindications, adverse reactions and the method of use with dosages will be identical to the drugs discussed above.
Cabergoline, Bergolak and Agalates are cheaper analogues of the “original”, differing mainly only in the manufacturer.
Therefore, it is difficult to unequivocally answer the question of which is better: Dostinex or Bergolak, because the drugs contain one active ingredient. Differences can only be found in price, contraindications and individual intolerance to the additional components of these medications.
4 And now about a medication to stop lactation, which differs from Dostinex in the active substance - bromocriptine (quinagolide). Bromocriptine is produced in Russia. It has a similar effect on dopamine receptors. The drug reduces the production of prolactin and suppresses the physiological process of lactation. It has a low price - from 220 rubles. per package.
Drugs to stop lactation should be used with extreme caution. This threatens, among other things,
inflammation of the mammary glands
Bromocriptine preparations are the cheapest medications for cessation of lactation - one package is enough for a course of treatment. But many are frightened by the duration of treatment (2 weeks) and the impressive list of side effects.
You need to be careful when choosing and using birth control pills when breastfeeding. Which is better to use, Charozetta or Lactinet, is explained in a separate publication
Bromocriptine to stop lactation will require longer use: the tablets should be taken in half on the first day, and then 1 tablet at a time. 2 times a day for 2 weeks. It is recommended to take Bromocriptine with food.
If the task is to restore lactation, then how to do it correctly is described here.
Pharmacokinetics
Suction
After oral administration, cabergoline is rapidly absorbed from the gastrointestinal tract. Cmax in blood plasma is reached after 0.5-4 hours. Food does not affect the absorption or distribution of cabergoline.
Pharmacokinetics is linear up to a dose of 7 mg/day.
Distribution
The binding of cabergoline (at a concentration of 0.1-10 ng/ml) to plasma proteins is 41-42%.
Metabolism
Metabolites of cabergoline were found in the urine: 6-allyl-8β-carboxy-ergoline in an amount of 4-6% of the dose taken, as well as three other metabolites with a total content of less than 3%.
All metabolites inhibit prolactin secretion to a significantly lesser extent (compared to cabergoline).
Removal
Cabergoline has a long T1/2. T1/2 in healthy volunteers is 63-68 hours, T1/2 in patients with hyperprolactinemia is 79-115 hours. With this T1/2, the equilibrium state is achieved after 4 weeks.
In urine and feces, 18% and 72% of the dose taken were found, respectively. The content of unchanged cabergoline in urine is 2-3%.
Instructions:
Clinical and pharmacological group
15.040 (Prolactin secretion inhibitor)
Release form, composition and packaging
The tablets are white, flat, oval, with a bevel and a score on one side, engraved “0.5” on one side of the score and “CBG” on the other.
| 1 tab. | |
| cabergoline | 500 mcg |
Excipients: lactose, L-leucine, magnesium stearate (E572).
2 pcs. — dark glass bottles (1) — cardboard packs. 8 pcs. - dark glass bottles (1) - cardboard packs.
pharmachologic effect
Dopamine receptor agonist. Cabergoline is a synthetic ergot alkaloid, an ergoline derivative, a long-acting dopamine agonist that inhibits prolactin secretion. The mechanism of action of cabergoline involves stimulation of central dopamine receptors in the hypothalamus. At doses higher than those required to suppress prolactin secretion, the drug causes a central dopaminergic effect due to stimulation of dopamine D2 receptors. The effect of the drug is dose-dependent. A decrease in prolactin levels in the blood is usually observed after 3 hours and persists for 2-3 weeks, and therefore one dose of the drug is usually sufficient to suppress milk secretion. When treating hyperprolactinemia, the content of prolactin in the blood is normalized after 2-4 weeks of using the drug in an effective dose. Normal prolactin levels may persist for several months after discontinuation of the drug.
Cabergoline has a highly selective effect and does not affect the basal secretion of other pituitary hormones and cortisol. The only pharmacodynamic effect not related to the therapeutic effect is a decrease in blood pressure. The maximum hypotensive effect usually develops 6 hours after a single dose of the drug; the degree of blood pressure reduction and the frequency of development of the hypotensive effect are dose-dependent.
Pharmacokinetics
Suction
After oral administration, cabergoline is rapidly absorbed from the gastrointestinal tract. Cmax in blood plasma is reached after 0.5-4 hours. Food does not affect the absorption or distribution of cabergoline.
Pharmacokinetics is linear up to a dose of 7 mg/day.
Distribution
The binding of cabergoline (at a concentration of 0.1-10 ng/ml) to plasma proteins is 41-42%.
Metabolism
Metabolites of cabergoline were found in the urine: 6-allyl-8β-carboxy-ergoline in an amount of 4-6% of the dose taken, as well as three other metabolites with a total content of less than 3%.
All metabolites inhibit prolactin secretion to a significantly lesser extent (compared to cabergoline).
Removal
Cabergoline has a long T1/2. T1/2 in healthy volunteers is 63-68 hours, T1/2 in patients with hyperprolactinemia is 79-115 hours. With this T1/2, the equilibrium state is achieved after 4 weeks.
In urine and feces, 18% and 72% of the dose taken were found, respectively. The content of unchanged cabergoline in urine is 2-3%.
Dosage
Cabergoline is taken orally, preferably with meals.
For the treatment of disorders associated with hyperprolactinemia, the recommended starting dose is 500 mcg per week in 1 or 2 divided doses (eg, Monday and Thursday). The dose is increased gradually, usually by 500 mcg per week at intervals of 1 month until the optimal therapeutic effect is achieved. Maintenance dose - 1 mg/week (0.25-2 mg/week); in some cases in patients with hyperprolactinemia - up to 4.5 mg/week.
When using the drug in doses above 1 mg/week, it is recommended to divide the weekly dose into 2 or more doses depending on tolerability.
To suppress lactation, the recommended dose is 1 mg once during the first 24 hours after birth.
Considering the indications for use, experience with cabergoline in elderly patients is limited. Available data indicate no specific risk.
Overdose
There is no information about an overdose of the drug. Based on the results of animal experiments, one can expect the appearance of symptoms due to hyperstimulation of dopamine receptors: nausea, vomiting, decreased blood pressure, disturbances of consciousness/psychosis or hallucinations.
Treatment: if indicated, measures should be taken to restore blood pressure. In addition, with severe central nervous system symptoms (hallucinations), the use of dopamine antagonists may be required.
Drug interactions
The effect of macrolide antibiotics on plasma cabergoline levels when used together has not been studied. Given the possibility of increasing cabergoline levels, the drug is not recommended for use in combination with macrolides.
The mechanism of action of cabergoline is associated with direct stimulation of dopamine receptors, so it should not be used in combination with dopamine receptor antagonists (phenothiazines, butyrophenones, thioxanthenes, metoclopramide).
There is no information on the interaction of cabergoline with other ergot alkaloids, however, long-term use of this combination is not recommended.
Given the pharmacodynamics of cabergoline (hypotensive effect), it is necessary to take into account the interaction with drugs that lower blood pressure.
In clinical studies in patients with Parkinson's disease, no pharmacokinetic interaction was found with levodopa or selegiline.
Pharmacokinetic interactions with other drugs cannot be predicted based on available information on the metabolism of cabergoline.
Use during pregnancy and lactation
The drug is contraindicated during pregnancy and lactation (breastfeeding).
Before starting to take the drug, pregnancy should be excluded. It is recommended to avoid pregnancy for at least 1 month after stopping treatment. There are limited data on the use of the drug during pregnancy obtained during the first 8 weeks after conception. The use of cabergoline was not associated with an increased risk of abortion, preterm birth, multiple pregnancies, or congenital disorders. No other data has been received to date.
In experimental animal studies, no direct or indirect adverse effects of cabergoline on pregnancy, embryo/fetal development, childbirth or postnatal development were found.
Given the limited experience with the use of cabergoline during pregnancy, the drug should be discontinued when planning pregnancy. If pregnancy occurs during treatment, cabergoline should be discontinued immediately. Due to the possibility of expansion of a pre-existing tumor, signs of enlargement of the pituitary gland in pregnant women should be monitored.
Because cabergoline suppresses lactation, the drug should not be prescribed to mothers who choose to breastfeed their infants. Breastfeeding should be discontinued during treatment with cabergoline.
Side effects
Undesirable effects are usually dose dependent and decrease with gradual dose reduction.
Suppression of lactation: adverse events occur in approximately 14% of patients. The most common: decreased blood pressure (12%), dizziness (6%) and headache (5%). With long-term treatment, the frequency of these effects increases to 70%.
The frequency of adverse reactions is presented in accordance with the following gradation: often (≥1/100, <1/10), sometimes (≥1/1000, <1/100), rarely (≥1/10,000, <1/1000).
From the nervous system: often - depression, headache and dizziness, paresthesia, feeling of fatigue, drowsiness.
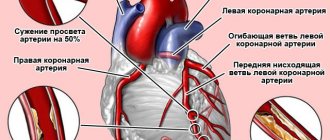
From the cardiovascular system: often - low blood pressure, increased heart rate and chest pain; sometimes - nosebleeds; rarely - fainting.
From the digestive system: nausea, vomiting, gastralgia, gastritis, constipation; rarely - liver dysfunction.
From the skin and subcutaneous tissue: often - hyperemia of the facial skin.
From the organ of vision: sometimes - hemianopia.
From the musculoskeletal system: rarely - cramps in the fingers and calf muscles.
Allergic reactions: rarely - skin rash.
A decrease in blood pressure (systolic by more than 20 mm Hg and diastolic by more than 10 mm Hg) was noted 3-4 days after a single dose of cabergoline 1 mg in women after childbirth.
Adverse effects usually develop during the first two weeks, then decrease or disappear. Discontinuation of the drug due to side effects was required in 3% of cases.
Post-marketing surveillance
Treatment with cabergoline has been associated with excessive daytime sleepiness and episodes of sudden sleep onset, especially in patients with Parkinson's disease.
There are reports of increased libido in patients with Parkinson's disease when treated with dopamine agonists, including cabergoline, especially at high doses. Also, during treatment with cabergoline, pleural effusions, pleural fibrosis, valvulopathy, and respiratory disorders (including respiratory failure) were noted.
Storage conditions and periods
The drug should be stored in a dry place, out of reach of children, in a tightly closed original bottle at a temperature not exceeding 30°C. Shelf life: 2 years.
Indications
- suppression of physiological postpartum lactation (only for medical reasons);
- suppression of already established lactation (only for medical reasons);
- disorders associated with hyperprolactinemia (including functional disorders such as amenorrhea, oligomenorrhea, anovulation, galactorrhea);
— prolactin-secreting pituitary adenomas (micro- and macroprolactinomas);
- idiopathic hyperprolactinemia.
Contraindications
- postpartum or uncontrolled arterial hypertension;
- severe liver dysfunction;
- adverse events from the lungs, such as pleurisy or fibrosis (including a history) associated with taking dopamine agonists;
— psychoses (including a history) or the risk of their development;
— pregnancy and preeclampsia and eclampsia that developed against it;
- lactation period (breastfeeding);
- hypersensitivity to cabergoline, other ergot alkaloids or any component of the drug.
The effectiveness and safety of cabergoline in children under 16 years of age have not been studied.
The drug should be prescribed with caution to patients with cardiovascular disease, arterial hypotension, Raynaud's syndrome, peptic ulcers or gastrointestinal bleeding, in patients with end-stage renal failure or on hemodialysis, in elderly patients.
special instructions
To open the bottle, first press the cap, then twist it as shown on the cap. Do not remove the capsule with silica gel from the bottle and do not ingest it.
Data on the efficacy and safety of cabergoline in patients with hepatic or renal impairment are limited. The pharmacokinetics of cabergoline does not change significantly in moderate or severe renal failure and has not been studied in patients with end-stage renal disease or hemodialysis. Therefore, the drug should be used with caution in such patients.
The effect of alcohol on the overall tolerability of cabergoline has not been established.
Cabergoline may cause symptomatic hypotension, especially when taken together with drugs that lower blood pressure. It is recommended to regularly measure blood pressure in the first 3-4 days after starting treatment.
Hyperprolactinemia in combination with amenorrhea and infertility may be associated with pituitary tumors, therefore, before starting treatment with cabergoline, it is necessary to find out the cause of hyperprolactinemia.
It is recommended to check serum prolactin levels every month, since after achieving an effective therapeutic regimen, normal prolactin levels remain for 2-4 weeks.
After discontinuation of the drug, hyperprolactinemia usually occurs again. However, some patients experience a persistent decrease in prolactin concentrations over several months.
Cabergoline restores ovulation and fertility in women with hyperprolactinemic hypogonadism. Since pregnancy can occur before the resumption of menstruation, pregnancy tests are recommended during the period of amenorrhea, and after the restoration of the menstrual cycle - in all cases of a delay of more than 3 days. Women who do not wish to become pregnant are advised to use effective non-hormonal contraception during and after treatment with cabergoline. Women planning a pregnancy are recommended to conceive no earlier than 1 month after discontinuation of the drug. In a number of patients, the ovulatory cycle persisted for 6 months after discontinuation of the drug.
With long-term use of cabergoline, like other ergot derivatives, pleural effusions/pulmonary fibrosis and heart valve damage may occur. Sometimes these phenomena were observed in patients who had previously received dopamine agonists from the ergot group. Discontinuation of cabergoline in the event of the development of this pathology led to an improvement in the patient's condition.
If new clinical symptoms from the respiratory system appear, fluoroscopy of the lungs is recommended. In patients with pleural effusions/fibrosis, an increase in ESR was noted, and therefore, if the ESR is elevated without obvious clinical signs, an x-ray examination should also be performed.
When using cabergoline, drowsiness and episodes of sudden sleep may occur, especially in patients with Parkinson's disease. Sudden falling asleep during daily activities, developing in some cases without warning, is rare.
The drug contains lactose. Patients with rare hereditary forms of galactose intolerance, lactase deficiency or glucose-galactose malabsorption should not take cabergoline.
Impact on the ability to drive a car and operate machinery
Cabergoline lowers blood pressure, which may impair reaction time in some patients. This must be taken into account in situations that require concentration, such as driving a car or operating machinery. Patients should be informed of the need to exercise caution when driving or operating machinery.
Patients who have already experienced drowsiness and/or sudden sleep episodes while being treated with cabergoline should avoid driving or engaging in other risky activities where impaired reaction time may pose a risk of serious injury or death to themselves and others. Sometimes it is advisable to reduce the dosage or discontinue the drug.
Preclinical safety data
As shown in preclinical studies, cabergoline is safe over a wide range of doses and has no teratogenic, mutagenic or carcinogenic effects.
Use for renal impairment
Data on the efficacy and safety of cabergoline in patients with impaired renal function are limited. The pharmacokinetics of cabergoline does not change significantly in moderate or severe renal impairment. Not studied in patients with end-stage renal disease or hemodialysis. Therefore, the drug should be used with caution in such patients.
Use for liver dysfunction
Data on the efficacy and safety of cabergoline in patients with impaired liver function. Therefore, the drug should be used with caution in such patients.
Conditions for dispensing from pharmacies
The drug is available with a prescription.
AGALATES: DOSAGE
Cabergoline is taken orally, preferably with meals.
For the treatment of disorders associated with hyperprolactinemia, the recommended starting dose is 500 mcg per week in 1 or 2 divided doses (eg, Monday and Thursday). The dose is increased gradually, usually by 500 mcg per week at intervals of 1 month until the optimal therapeutic effect is achieved. Maintenance dose - 1 mg/week (0.25-2 mg/week); in some cases in patients with hyperprolactinemia - up to 4.5 mg/week.
When using the drug in doses above 1 mg/week, it is recommended to divide the weekly dose into 2 or more doses depending on tolerability.
To suppress lactation, the recommended dose is 1 mg once during the first 24 hours after birth.
Considering the indications for use, experience with cabergoline in elderly patients is limited. Available data indicate no specific risk.
How to properly end breastfeeding
If a decision is made to wean a child from breastfeeding, then this must be done correctly.
The correct process for weaning a baby is as follows:
We teach the child to fall asleep without the breast.
This stage can take from 1 to 3 weeks depending on the age and readiness of the child. For a detailed plan and teaching methods, see the online course How to teach a child to fall asleep and sleep without breastfeeding?
- We reduce chaotic breastfeeding during the day.
- We gradually switch to 1–3 daily feedings.
- We are trying to cancel night feedings or reduce them (about night feedings, read my article How long should you feed your baby at night>>>).
- We completely remove feedings.
To stop milk production on your own, you don’t have to take special medications.
By gradually reducing the number of daily and nightly breastfeeding, you help your breasts readjust and produce less milk.
After completing breastfeeding, if you feel a slight filling of the breasts, you should pump the breasts until relief, but not completely.
Within a week the milk goes away.
You should not choose a medication option to stop lactation if there are no objective reasons for this. After all, breastfeeding is the key to a child’s health. And you can always cope with temporary difficulties, for example, simply by expressing breast milk.
And it is also worth understanding that only a doctor can prescribe medicine. Of course, you should take into account the recommendations of the instructions for use of Agalates to stop lactation, but the exact dosage and duration of the course must be confirmed by a doctor.
If you want to finish breastfeeding gently, without harming the baby and your body, watch the online course Weaning Formula: how to breastfeed after a year and smoothly end breastfeeding>>>
Complete lactation correctly!
- How to restore breasts after feeding?
- A child hangs on his chest after a year: reasons and what to do?
- Hair loss during breastfeeding
Drug interactions
The effect of macrolide antibiotics on plasma cabergoline levels when used together has not been studied. Given the possibility of increasing cabergoline levels, the drug is not recommended for use in combination with macrolides.
The mechanism of action of cabergoline is associated with direct stimulation of dopamine receptors, so it should not be used in combination with dopamine receptor antagonists (phenothiazines, butyrophenones, thioxanthenes, metoclopramide).
There is no information on the interaction of cabergoline with other ergot alkaloids, however, long-term use of this combination is not recommended.
Given the pharmacodynamics of cabergoline (hypotensive effect), it is necessary to take into account the interaction with drugs that lower blood pressure.
In clinical studies in patients with Parkinson's disease, no pharmacokinetic interaction was found with levodopa or selegiline.
Pharmacokinetic interactions with other drugs cannot be predicted based on available information on the metabolism of cabergoline.
Pregnancy and lactation
The drug is contraindicated during pregnancy and lactation (breastfeeding).
Before starting to take the drug, pregnancy should be excluded. It is recommended to avoid pregnancy for at least 1 month after stopping treatment. There are limited data on the use of the drug during pregnancy obtained during the first 8 weeks after conception. The use of cabergoline was not associated with an increased risk of abortion, preterm birth, multiple pregnancies, or congenital disorders. No other data has been received to date.
In experimental animal studies, no direct or indirect adverse effects of cabergoline on pregnancy, embryo/fetal development, childbirth or postnatal development were found.
Given the limited experience with the use of cabergoline during pregnancy, the drug should be discontinued when planning pregnancy. If pregnancy occurs during treatment, cabergoline should be discontinued immediately. Due to the possibility of expansion of a pre-existing tumor, signs of enlargement of the pituitary gland in pregnant women should be monitored.
Because cabergoline suppresses lactation, the drug should not be prescribed to mothers who choose to breastfeed their infants. Breastfeeding should be discontinued during treatment with cabergoline.
How does sudden cessation of breastfeeding affect a baby?
A child who is used to receiving your milk is not ready to suddenly lose it in 1 day.
The World Health Organization says that the duration of breastfeeding should be up to 2 years or more, if there is consent of the mother and child. About the importance of long-term feeding in the article Breastfeeding after a year: why?>>>. From the psychological side, the question is more individual
Some children are ready to stop breastfeeding a little earlier, while others are not yet ready to stop breastfeeding at 2 years of age.
From the psychological side, the question is more individual. Some children are ready to stop breastfeeding a little earlier, while others are not yet ready to stop breastfeeding even at 2 years old.
If you stop breastfeeding early without good reason, you can harm your baby. Since mother’s milk supplies his body with valuable components responsible for the child’s growth. Milk contains immunoglobulins, which provide the baby with immunity.
You won’t find such components even in the most expensive and high-quality baby food.
Psychologically, abrupt weaning will have a negative impact on the child. After all, it is breastfeeding that provides an additional relationship between mother and child. For the baby, this loss will be real stress.
It is for this reason that do not use medications, as well as old grandmother’s methods: bandaging the chest, leaving the child for a couple of days, and so on.
The cessation of lactation should be gradual.
AGALATES: SIDE EFFECTS
Undesirable effects are usually dose dependent and decrease with gradual dose reduction.
Suppression of lactation: adverse events occur in approximately 14% of patients. The most common: decreased blood pressure (12%), dizziness (6%) and headache (5%). With long-term treatment, the frequency of these effects increases to 70%.
The frequency of adverse reactions is presented in accordance with the following gradation: often (≥1/100,
From the nervous system: often - depression, headache and dizziness, paresthesia, feeling of fatigue, drowsiness.
From the cardiovascular system: often - low blood pressure, increased heart rate and chest pain; sometimes - nosebleeds; rarely - fainting.
From the digestive system: nausea, vomiting, gastralgia, gastritis, constipation; rarely - liver dysfunction.
From the skin and subcutaneous tissue: often - hyperemia of the facial skin.
From the organ of vision: sometimes - hemianopia.
From the musculoskeletal system: rarely - cramps in the fingers and calf muscles.
Allergic reactions: rarely - skin rash.
A decrease in blood pressure (systolic by more than 20 mm Hg and diastolic by more than 10 mm Hg) was noted 3-4 days after a single dose of cabergoline 1 mg in women after childbirth.
Adverse effects usually develop during the first two weeks, then decrease or disappear. Discontinuation of the drug due to side effects was required in 3% of cases.
Post-marketing surveillance
Treatment with cabergoline has been associated with excessive daytime sleepiness and episodes of sudden sleep onset, especially in patients with Parkinson's disease.
There are reports of increased libido in patients with Parkinson's disease when treated with dopamine agonists, including cabergoline, especially at high doses. Also, during treatment with cabergoline, pleural effusions, pleural fibrosis, valvulopathy, and respiratory disorders (including respiratory failure) were noted.
Use of the drug
Agalates is a hormonal drug that is used to suppress the secretory function of the pituitary gland. The cessation of lactation occurs after 1–15 days. The drug method is only suitable for emergency cases, as it has many contraindications. To avoid side effects, self-medication is strictly prohibited!
Agalates is used to stop milk production for the following medical indications:
- severe purulent mastitis;
- tuberculosis (open form);
- malignant formation;
- absence of milk ducts in the mammary glands;
- taking potent medications.
One tablet will be enough to stop milk production. If you are weaning your newborn from breastfeeding, take ¼ of the tablet at 12-hour intervals within 48 hours. Take the tablet with a glass of still water.
Contraindications
- postpartum or uncontrolled hypertension;
- severe liver dysfunction;
- adverse events from the lungs,
- such as pleurisy or fibrosis (incl.
- in the anamnesis),
- associated with dopamine agonists;
- psychoses (incl.
- history) or the risk of their development;
- pregnancy and preeclampsia and eclampsia that developed against it;
- lactation period (breastfeeding);
- hypersensitivity to cabergoline,
- other ergot alkaloids or any component of the drug.
The effectiveness and safety of cabergoline in children under 16 years of age have not been studied.
The drug should be prescribed with caution to patients with cardiovascular disease, arterial hypotension, Raynaud's syndrome, peptic ulcers or gastrointestinal bleeding, in patients with end-stage renal failure or on hemodialysis, in elderly patients.
Reviews
According to reviews from women who have tried the effect of the drug on themselves, Agalates is an effective hormonal remedy for stopping milk production. The drug is able to stop lactation in a short time. In most cases, Agalates is well tolerated by patients. To stop breastfeeding, 1 tablet is enough.
Women are satisfied with the effectiveness, inexpensive cost of the drug and short course of treatment. Many nursing mothers use this particular medication to stop lactation. You can find information about other drugs to stop lactation at this link.
In some cases, Agalates causes side effects such as allergies, nausea, swelling or dizziness. This is due to hypersensitivity of some components of the drug or dosage violation.
Thus, Agalates is allowed to be used only after a doctor’s prescription.
The medication is strictly prohibited if a lactating woman is allergic to any component of the drug or has other contraindications. Self-medication can have dangerous consequences for the health of mother and child! Subscribe to our VKontakte group
special instructions
To open the bottle, first press the cap, then twist it as shown on the cap. Do not remove the capsule with silica gel from the bottle and do not ingest it.
Data on the efficacy and safety of cabergoline in patients with hepatic or renal impairment are limited. The pharmacokinetics of cabergoline does not change significantly in moderate or severe renal failure and has not been studied in patients with end-stage renal disease or hemodialysis. Therefore, the drug should be used with caution in such patients.
The effect of alcohol on the overall tolerability of cabergoline has not been established.
Cabergoline may cause symptomatic hypotension, especially when taken together with drugs that lower blood pressure. It is recommended to regularly measure blood pressure in the first 3-4 days after starting treatment.
Hyperprolactinemia in combination with amenorrhea and infertility may be associated with pituitary tumors, therefore, before starting treatment with cabergoline, it is necessary to find out the cause of hyperprolactinemia.
It is recommended to check serum prolactin levels every month, since after achieving an effective therapeutic regimen, normal prolactin levels remain for 2-4 weeks.
After discontinuation of the drug, hyperprolactinemia usually occurs again. However, some patients experience a persistent decrease in prolactin concentrations over several months.
Cabergoline restores ovulation and fertility in women with hyperprolactinemic hypogonadism. Since pregnancy can occur before the resumption of menstruation, pregnancy tests are recommended during the period of amenorrhea, and after the restoration of the menstrual cycle - in all cases of a delay of more than 3 days. Women who do not wish to become pregnant are advised to use effective non-hormonal contraception during and after treatment with cabergoline. Women planning a pregnancy are recommended to conceive no earlier than 1 month after discontinuation of the drug. In a number of patients, the ovulatory cycle persisted for 6 months after discontinuation of the drug.
With long-term use of cabergoline, like other ergot derivatives, pleural effusions/pulmonary fibrosis and heart valve damage may occur. Sometimes these phenomena were observed in patients who had previously received dopamine agonists from the ergot group. Discontinuation of cabergoline in the event of the development of this pathology led to an improvement in the patient's condition.
If new clinical symptoms from the respiratory system appear, fluoroscopy of the lungs is recommended. In patients with pleural effusions/fibrosis, an increase in ESR was noted, and therefore, if the ESR is elevated without obvious clinical signs, an x-ray examination should also be performed.
When using cabergoline, drowsiness and episodes of sudden sleep may occur, especially in patients with Parkinson's disease. Sudden falling asleep during daily activities, developing in some cases without warning, is rare.
The drug contains lactose. Patients with rare hereditary forms of galactose intolerance, lactase deficiency or glucose-galactose malabsorption should not take cabergoline.
Impact on the ability to drive a car and operate machinery
Cabergoline lowers blood pressure, which may impair reaction time in some patients. This must be taken into account in situations that require concentration, such as driving a car or operating machinery. Patients should be informed of the need to exercise caution when driving or operating machinery.
Patients who have already experienced drowsiness and/or sudden sleep episodes while being treated with cabergoline should avoid driving or engaging in other risky activities where impaired reaction time may pose a risk of serious injury or death to themselves and others. Sometimes it is advisable to reduce the dosage or discontinue the drug.
Preclinical safety data
As shown in preclinical studies, cabergoline is safe over a wide range of doses and has no teratogenic, mutagenic or carcinogenic effects.
What is Dostinex
Dostinex is a medical drug with the active component cabergoline, which is prescribed to women to reduce the level of prolactin produced. The hormone prolactin regulates milk production in the body during lactation. The drug is intended to suppress the lactation process and complete breastfeeding. This medicine is also prescribed for a pathological increase in the synthesis of prolactin in the body.
The product is sold in dark glass-plastic bottles with 2 or 8 oblong flat tablets per bottle. In addition to suppressing lactation processes, taking Dostinex tablets:
- restores the menstrual cycle and reduces the likelihood of an anovulatory cycle;
- the concentration of estrogen in the body increases;
- symptoms characteristic of a number of other painful conditions are reduced.