Write a review
Reviews: 0
Manufacturers: Sanavita Gesundheitsmittel Gmbh & Co.Kg
Active ingredients
- Phenoxymethylpenicillin
Disease class
- Purulent and unspecified otitis media
- Acute and subacute endocarditis
- Nonspecific lymphadenitis
- Acute pharyngitis, unspecified
- Pneumonia without specifying the pathogen
- Chronic sinusitis
- Bronchitis, not specified as acute or chronic
- Lichen ruber planus
- Rheumatism, unspecified
- Scarlet fever
- Erysipelas
- Acute tonsillitis, unspecified
Clinical and pharmacological group
- Not indicated. See instructions
Pharmacological action
- Antimicrobial
- Antibacterial
- Bactericidal
Pharmacological group
- Penicillins
Pharmacological properties of the drug Phenoxymethylpenicillin
Phenoxymethylpenicillin is a β-lactam antibiotic of the penicillin group. Acts bactericidal. It is acid-stable and well absorbed from the digestive tract, allowing it to be taken orally. Destroyed by penicillinase. Active against pyogenic and hemolytic streptococci, pneumococci, gonococci and meningococci, listeria. Erysipelothrix insidiosa , corynebacteria, anthrax bacillus, actinomycetes, Clostridia tetanus and other anaerobic clostridia, Treponema pallidum and most strains of Leptospira are sensitive to phenoxymethylpenicillin Less sensitive are Streptococcus viridans (active against 70–80% of strains), enterococci (20–40% of strains are sensitive), and in high concentrations have an effect on some gram-negative E. coli, for example Escherichia , some forms of Proteus and Salmonella. All strains of Staphylococcus aureus that produce penicillinase (90% of all hospital strains of staphylococcus), Staphylococcus epidermidis , group D streptococci ( Streptococcus faecalis ), pseudomonas, Brucella, Francisella, Bordetella, mycobacteria, mycoplasma, rickettsia, bedsonia, fungi, protozoa are resistant; From the group of anaerobic microbes, B. fragilis . In recent years, there has been a change in the sensitivity of gonococci and hemolytic streptococci to penicillin. In addition to most gram-negative bacteria, rickettsia, viruses, protozoa, and fungi are resistant to phenoxymethylpenicillin. The maximum concentration in blood plasma is observed 1 hour after ingestion on an empty stomach or 2 hours after ingestion with food; The therapeutic concentration is maintained for 4 hours. Compared to benzylpenicillin, phenoxymethylpenicillin penetrates tissues more easily and in large quantities and is released from the body more slowly. The biological half-transformation period is about 30 minutes. Within 6 hours, about 30–40% is excreted unchanged in the urine. Penetrates the placental barrier and enters breast milk. Removed by hemodialysis.
Pharmacodynamics and pharmacokinetics
The principle of action is based on suppressing the process of cell wall synthesis.
Phenoxymethylpenicillin has a bactericidal effect against most gram-positive bacteria (streptococci, staphylococci), a small part of gram-negative cocci (neisseria), treponemas, corynobacteria, listeria.
The drug has no effect on Streptococcus spp., the main difference of which is the ability to independently produce penicillinase (a specific enzyme that breaks down and inactivates beta-lactam antibiotics).
Phenoxymethylpenicillin does not affect the activity of viruses, causative agents of amebiasis , most gram-negative cocci, and rickettsia.
The active component is considered acid-resistant and is destroyed upon contact with penicillinase.
Indications for use of the drug Phenoxymethylpenicillin
Used for the treatment of infectious diseases caused by microorganisms sensitive to penicillin (mainly for moderate infections). It is a first-line drug for the treatment of streptococcal infections (primarily tonsillitis and pharyngitis), as well as for the prevention of associated complications (acute rheumatic fever and minor chorea, rheumatoid arthritis, endocarditis and glomerulonephritis), as well as a means for the prevention of bacterial endocarditis after minor surgical procedures. interventions (tonsillectomy, tooth extraction, etc.). May be prescribed to intensify or continue parenteral penicillin therapy.
Side effects
The antibiotic can cause allergic responses in the form of rhinitis, hyperemia (local redness) of the skin, angioedema, conjunctivitis, and urticaria.
anaphylactic shock , eosinophilia, serum sickness, fever and arthralgia develop during treatment
Phenoxymethylpenicillin tablets can provoke the development of leukopenia, pancytopenia, hemolytic anemia , thrombocytopenia and agranulocytosis.
Digestive tract: vesicular cheilitis (caused by the irritating effect of the active component on the mucous walls), stomatitis, glossitis , dyspeptic disorders (diarrhea syndrome, vomiting, epigastric discomfort and nausea), dry mouth, perversion of taste perception, loss of appetite, pseudomembranous enterocolitis ( rarely occurs).
During treatment, the development of pharyngitis, vasculitis, and interstitial neuritis .
Use of the drug Phenoxymethylpenicillin
Prescribed orally 0.5–1 hour before meals. The daily dose is divided into 4–6 doses. The average single dose for adults is 0.25 g, the daily dose is 1.5 g or more. For children under 5 years of age, the drug is prescribed at a dose of 25-30 mg/kg body weight, from 5 to 12 years - 0.6-0.9 g, over 12 years - 0.8-1 g per day. At the same time, ascorbic acid can be prescribed, as it increases the bioavailability of phenoxymethylpenicillin. The duration of treatment is at least 5-7 days, for infections caused by β-hemolytic streptococcus - 7-10 days (prescribed every 4 hours, if improvement is achieved - every 6 hours). To prevent streptococcal infections, a 10-day intake in medium therapeutic doses is prescribed. To prevent relapses of rheumatic attack and/or minor chorea, 500 mg is prescribed 2 times a day. To prevent endocarditis after minor surgical interventions, adults and older children (body weight more than 30 kg) are prescribed 2 g 30–60 minutes before surgery, and then 500 mg every 6 hours for 2 days or more after surgery. children weighing less than 30 kg - 1 g before surgery, and then 250 mg every 6 hours for 2 days or more. In case of renal failure, it is necessary to reduce the dose or increase the interval between doses.
Instructions:
Clinical and pharmacological group
06.001 (Antibiotic of the penicillin group, destroyed by penicillinase)
Release form, composition and packaging
Syrup in the form of an orange-yellow suspension.
| 5 ml (1 sc.l.) | |
| phenoxymethylpenicillin (as benzathine salt) | 750 thousand IU |
Excipients: propyl parahydroxybenzoate, simethicone, sodium saccharin, methyl parahydroxybenzoate, citric acid monohydrate, fruit flavor, yellow iron oxide, sodium carmellose, sodium cyclamate, magnesium aluminum silicate, trisodium citrate dihydrate, sorbitol, purified water.
60 ml - dark glass bottles (1) complete with a dosing spoon - cardboard packs.
pharmachologic effect
An antibiotic of the penicillin group for oral administration, destroyed by penicillinase. It has a bactericidal effect against sensitive reproducing microorganisms by suppressing the biosynthesis of bacterial cell membranes.
Active against Streptococcus groups A, C, G, H, L and M (including Streptococcus pneumoniae), which do not produce penicillinase Staphylococcus spp. and Neisseria spp.
Erysipelotrix rhusiopathiae, Listeria spp., Corynebacterium spp., Bacillus anthracis, Actinomyces spp., Streptobacillus spp., Pasteurella multocida, Spirillium minus, Leptospira spp., Treponema spp., Borellia spp., anaerobic pathogens (Peptococcus spp. , Peptostreptococcus spp., Fusobacterium spp., Clostridium spp.).
Of the enterococcal strains (group D streptococci), only some showed sensitivity to the drug.
Not active against Staphylococcus spp., producing penicillinase, Mycobacterium tuberculosis, most gram-negative bacteria, viruses, Rickettsia spp., Entamoeba histolytica.
Acid resistant; destroyed by penicillinase.
Pharmacokinetics
Suction
Phenoxymethylpenicillin is stable in an acidic environment, as a result of which the drug is not inactivated by gastric acid. Absorbed quickly. Cmax in serum and tissues is achieved within 30-60 minutes.
Distribution
Plasma protein binding is 55%. It easily penetrates into the kidneys, lungs, liver, skin, mucous membranes, muscles and most body fluids, especially in the presence of inflammatory processes, and less well into bone tissue.
Removal
T1/2 is 30-45 minutes. It is excreted by the kidneys unchanged (25%) and in the form of metabolites (35%), about 30% in feces. A small part of the dose taken is excreted through the bile ducts.
Pharmacokinetics in special clinical situations
T1/2 is prolonged in newborns, elderly patients, and with renal failure.
Dosage
Children aged 1 to 6 years (with a body weight of 10-22 kg) are prescribed 375 thousand IU (1/2 scoop) 3 times a day; children aged 6 to 12 years (with a body weight of 22-38 kg) - 750 thousand IU (1 scoop) 3 times a day; for adolescents and adults - 1,500 thousand IU (2 scoops) 3 times a day. If necessary, the daily dose can be increased.
Treatment should be continued for at least 3 days after the symptoms of the disease disappear.
When treating streptococcal infections, take the drug for at least 10 days.
In case of contact with patients with streptococcal diseases (for example, tonsillitis, scarlet fever), taking the drug for 10 days in therapeutic doses can prevent the development of the disease.
To prevent rheumatic fever, chorea minor and sickle cell anemia, adults and children weighing >30 kg are prescribed 375 thousand IU (1/2 scoop) 2 times a day; Children weighing <30 kg are recommended to be prescribed other forms of Ospena in a lower dosage.
To prevent endocarditis (after minor surgical interventions / tonsillectomy, tooth extraction/), children weighing <30 kg are prescribed 1500 thousand IU (2 scoops) approximately 1 hour before surgery, then 375 thousand IU (1/2 scoops each). 2 scoops) every 6 hours for 2 days after surgery.
Adolescents and adults are prescribed 3,000 thousand IU (4 scoops) approximately 1 hour before surgery, then 750 thousand IU (1 scoop) every 6 hours for 2 days after surgery.
Due to the low toxicity of phenoxymethylpenicillin, the required dose for patients with renal and/or liver failure should not be reduced. If necessary, a dose reduction can be made according to individual indications. For anuria, the dose should be reduced or the interval between doses of the drug increased.
Overdose
Currently, no cases of overdose of Ospen 750 have been reported.
Drug interactions
Since penicillins are active only against reproducing microorganisms, phenoxymethylpenicillin should not be combined with bacteriostatic antibiotics (macrolides, chloramphenicol, lincosamides, tetracyclines). Combination with other antibiotics is allowed if a synergistic or additive effect is expected. Combination antibiotics are prescribed in full dose. However, in the case of a combination with a proven synergistic effect, the dose of the more toxic drug may be reduced.
With simultaneous use, antacids, glucosamine, laxatives, aminoglycosides slow down and reduce the absorption of phenoxymethylpenicillin, while ascorbic acid increases it.
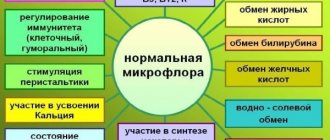
Phenoxymethylpenicillin increases the effectiveness of indirect anticoagulants by suppressing intestinal microflora and thereby reducing the formation of vitamin K.
With simultaneous use, phenoxymethylpenicillin reduces the effectiveness of oral contraceptives and drugs, during the metabolism of which para-aminobenzoic acid is formed.
Phenoxymethylpenicillin increases the risk of breakthrough bleeding while taking ethinyl estradiol.
Diuretics, aminopurinol, phenylbutazone, NSAIDs and other drugs that reduce tubular secretion increase the concentration of phenoxymethylpenicillin when used simultaneously.
When used simultaneously with phenoxymethylpenicillin, allopurinol increases the risk of allergic reactions (skin rash).
Use during pregnancy and lactation
During pregnancy and lactation, phenoxymethylpenicillin should be prescribed with caution and only when the expected benefit to the mother outweighs the potential risk to the fetus or newborn.
To date, there is no evidence indicating that phenoxymethylpenicillin used during pregnancy has an embryotoxic, teratogenic or mutagenic effect. However, phenoxymethylpenicillin crosses the placental barrier and is found in small quantities in the milk of nursing mothers.
Side effects
From the digestive system: sometimes - nausea, diarrhea, vomiting, feeling of fullness in the stomach, stomatitis and glossitis. If diarrhea occurs, the development of pseudomembranous enterocolitis should be excluded.
From the hematopoietic system: rarely - eosinophilia, positive direct Coombs test, hemolytic anemia, thrombocytopenia, agranulocytosis.
Allergic reactions: urticaria, angioedema, erythema multiforme, exfoliative dermatitis, fever, arthralgia, anaphylactic shock, collapse, anaphylactoid reactions (asthma, purpura, gastrointestinal symptoms). These adverse reactions when taken orally are observed less frequently and are less pronounced than when treated with parenteral forms of penicillin.
Storage conditions and periods
List B. The drug should be stored in a place protected from light, out of reach of children at a temperature of 8° to 15°C. Shelf life: 2 years.
Indications
Treatment and prevention of mild to moderate infections caused by microorganisms sensitive to penicillin:
- infections of the ear, throat and nose (including scarlet fever, tonsillitis, ulcerative gingivitis /Vincent's sore throat/, pharyngitis, tonsillopharyngitis, purulent rhinopharyngitis, acute otitis media, sinusitis);
- respiratory tract infections (including bacterial bronchitis, bacterial pneumonia, bronchopneumonia /except for those where parenteral administration of penicillins is required/);
— skin infections (including erysipelas, pyoderma / contagious impetigo, furunculosis/, abscesses, phlegmon);
- chronic migratory erythema or other clinical manifestations of Lyme disease;
- infected wounds and burns.
Prevention:
— streptococcal infections and their complications (including rheumatic fever or minor chorea, polyarthritis, endocarditis, glomerulonephritis);
— bacterial endocarditis in patients with congenital or rheumatic heart defects before and after minor surgical interventions (tonsillectomy, tooth extraction);
— pneumococcal infections in children with sickle cell anemia.
Contraindications
- severe gastrointestinal diseases accompanied by diarrhea and vomiting (as absorption of the drug may be reduced);
- hypersensitivity to penicillin drugs (in patients with known hypersensitivity to cephalosporins, possible cross-allergy to penicillins should be kept in mind);
- hypersensitivity to sorbitol or preservatives (for syrup).
The drug should be prescribed with caution for allergic diathesis and bronchial asthma.
special instructions
If allergic reactions develop in patients, the drug should be discontinued and appropriate treatment prescribed.
For staphylococcal infections, bacteriological studies should be carried out.
In patients receiving penicillin to prevent rheumatic fever, the dose should be doubled before undergoing planned surgical interventions (tonsillectomy, tooth extraction) and during postoperative prophylaxis.
During long-term therapy with Ospen 750, a detailed blood test should be performed along with a study of liver and kidney function.
During long-term treatment, the potential for the growth of resistant strains of microorganisms and fungi should be kept in mind.
If prolonged diarrhea develops during treatment with Ospen 750, pseudomembranous colitis (loose, watery stools with mucus and streaks of blood, diffuse or cramping abdominal pain, fever and, sometimes, tenesmus) should be excluded. Since this condition can threaten the patient’s life, the drug should be immediately discontinued and, based on the results of bacteriological testing, appropriate treatment should be prescribed (for example, vancomycin orally 250 mg 4 times a day). Drugs that inhibit gastrointestinal motility are contraindicated.
In the acute stage of severe pneumonia, empyema, sepsis, pericarditis, endocarditis, meningitis, arthritis and osteomyelitis, parenteral forms of penicillin should be used.
Treatment with phenoxymethylpenicillin may cause a false-positive reaction in non-enzymatic urine glucose determination and urobilinogen testing. Also, the results of quantitative determination of amino acids in urine using the ninhydrin method may be false positive.
Use for renal impairment
Due to the low toxicity of phenoxymethylpenicillin, the required dose for patients with renal failure should not be reduced. If necessary, a dose reduction can be made according to individual indications. For anuria, the dose should be reduced or the interval between doses of the drug increased.
Use for liver dysfunction
Due to the low toxicity of phenoxymethylpenicillin, the required dose for patients with liver failure should not be reduced. If necessary, a dose reduction can be made according to individual indications.
Conditions for dispensing from pharmacies
The drug is available with a prescription.
Special instructions for the use of the drug Phenoxymethylpenicillin
With hypersensitivity to cephalosporin antibiotics, there may be a cross-allergy to penicillins (5–10% of cases). Phenoxymethylpenicillin should be prescribed with caution to patients with allergic diathesis and asthma. If allergic reactions occur, stop taking phenoxymethylpenicillin and, depending on the severity of the reaction, prescribe epinephrine, corticosteroids and antihistamines. For patients taking drugs of the penicillin group for the prevention of rheumatic diseases, it is advisable to switch to prophylactic use of any other antibacterial agents a week before surgical interventions (tonsillectomy, tooth extraction, etc.); after surgery, in order to prevent possible bacteremia, their use should be resumed. With long-term use of phenoxymethylpenicillin, it is recommended to periodically examine the cellular composition of peripheral blood and evaluate the functional state of the kidneys.
Release form and composition
Phenoxymethylpenicillin is available in the following forms:
- tablets: flat-cylindrical, round, white or almost white, with a bevel (dosage 100 mg) or with a bevel and a score (dosage 250 mg) (10 pcs. in blister or blister-free packages; in a cardboard pack of 1, 2 or 3 contour packaging);
- powder for the preparation of a suspension for oral administration: white or almost white, with a specific odor (2.5 g in bags, 30 bags in a cardboard box, complete with or without a plastic cup; 5 g in bags, 15 bags in a cardboard box complete with or without a plastic cup).
Composition per 1 tablet:
- active ingredient: phenoxymethylpenicillin – 100 mg or 250 mg;
- auxiliary components: talc, lactose monohydrate, calcium stearate, potato starch.
Composition for 1 sachet of powder for preparing the suspension:
- active ingredient: phenoxymethylpenicillin – 37.5 mg or 75 mg;
- auxiliary components: sodium benzoate, sucrose, citric acid monohydrate, raspberry flavor.
Drug interactions Phenoxymethylpenicillin
Sodium bicarbonate reduces the absorption of phenoxymethylpenicillin in the intestine. Combined administration with sulfonamides and bacteriostatic antibiotics (tetracyclines, chloramphenicol, erythromycin, etc.) mutually reduces the effectiveness of the drugs. When phenoxymethylpenicillin is prescribed simultaneously with hormonal contraceptives, the effectiveness of the latter is reduced. Probenecid, phenylbutazone, salicylates and indomethacin slow down the excretion of phenoxymethylpenicillin by the kidneys and thus prolong its action. Combination with aminoglycoside antibiotics enhances the antibacterial effect against enterococci and streptococci.
List of pharmacies where you can buy Phenoxymethylpenicillin:
- Moscow
- Saint Petersburg
Contraindications
Absolute:
- aphthous pharyngitis and stomatitis;
- gastrointestinal diseases accompanied by diarrhea and vomiting;
- decreased activity of the muscular apparatus of the stomach, increased intestinal motility or spasm of the cardiac esophagus;
- severe infections (including severe pneumonia in the acute stage);
- lactase/sucrase deficiency, lactose/fructose intolerance, glucose-galactose malabsorption syndrome;
- children under 3 years of age (for tablets);
- children up to 3 months (for powder for preparing a suspension);
- hypersensitivity to the ingredients of the drug and other beta-lactam antibiotics (cephalosporins, penicillins, carbapenems).
Relative (Phenoxymethylpenicillin is used with caution):
- diabetes;
- bronchial asthma;
- diathesis;
- hay fever;
- history of allergic reactions.
Cautions for use
The drug should be used with caution in patients with allergic diathesis and bronchial asthma. During pregnancy and breastfeeding, it is possible to take Phenoxymethylpenicillin, but before starting treatment, you should carefully weigh the expected benefits of its use for the mother and the potential risk for the fetus or child. In case of renal failure, it is necessary to reduce the dose or increase the interval between doses. Patients with an allergic reaction to cephalosporin antibiotics (cephalexin, cefazolin, ceftriaxone, cefotaxime, etc.) may experience a cross-allergy to Phenoxymethylpenicillin.