From this article you will learn:
- what is isotretinoin,
- Acnecutane and Roaccutane - instructions, reviews,
- differences between these drugs.
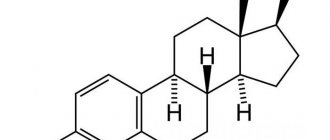
Isotretinoin is a retinoid that is also known as 13-cis-retinoic acid (Figure 1). This chemical compound is an isomer of tretinoin (trans-retinoic acid), which, like isotretinoin, is a structural analogue of vitamin A. Isotretinoin is best known as an oral systemic retinoid that is used to treat severe forms of acne. The latter include, for example, nodular and conglobate forms of acne, as well as forms of acne that are resistant even to oral antibiotics.
Systemic retinoids containing isotretinoin include drugs such as Acnecutane and Roaccutane. As we said above, they are intended for oral administration (available in capsule form). However, there are preparations with isotretinoin for external use that can be used to treat photoaging of facial skin. These drugs include those available on the Russian market - Retasol drugs, as well as retinoic ointment.
Isotretinoin (13-cis-retinoic acid) –
Reviews from dermatologists about Acnecutane and Roaccutane are the most positive, because in fact, these drugs with isotretinoin have made a real revolution in the treatment of severe forms of acne. They have improved the quality of life for many patients, including preventing the formation of scars. Isotretinoin therapy provides complete remission of the disease in almost all patients with acne, and after completion of the course of therapy, remission can last up to several months or even years.
However, therapy with systemic retinoids is associated with the risk of quite severe side effects, which we will discuss in detail below (they occur especially often if the dosage is incorrectly selected). Girls and women should take into account that these drugs have a pronounced teratogenic effect, and therefore they are prohibited both during pregnancy and breastfeeding. In addition, the entire period of use of the drug will require a two-level contraceptive system (both oral contraceptives and condoms).
How much do Roaccutane and Acnecutane cost in pharmacies -
For 2021, the price for Roaccutane will be from 1900 rubles - for a package of 30 capsules of 10 mg. It should be noted that this drug can now not be purchased in every pharmacy, which is apparently due to the current re-registration of the drug on the Russian market. For Acnekutan, the price for a package of 30 capsules of 8 mg will be from 1650 rubles, and for a package of 30 capsules of 16 mg - from 2600 rubles.
Analogs of Roaccutane include such drugs as Sotret (India) and Verocutan (Russia). The first one costs from 1350 rubles per pack of 30 capsules of 10 mg. As for the Russian drug Verokutan, it has currently disappeared from sale.
Forms of release of the drug
Isotretinoin is available in several forms: a drug for external use and internal. For oral administration, tablets or capsules with different dosages are provided.
For topical application, the product is produced in the form of:
- ointments;
- gel;
- solution.
Each form has a different dosage. In most cases, tablets and capsules are produced with a dosage of 10 or 20 mg of the active substance. With the exception of the drug Acnecutan, the amount of Isotretinoin in it can be either 8 mg or 16 mg.
This difference is due to the fact that Acnecutan is the softest and most gentle drug, it has a reduced number of contraindications and possible side effects. The ointment is available in a possible dosage of 0, 1 or 0.05 of the active ingredient. The ointment is called retinoic. Local retinoids are used at stages 2-3 of acne.
The solution for external use is produced in a concentration of 0.25, its volume is 50 ml.
The gel for external use is produced in a tube, the volume of which is 30 g. The gel contains additional active components that increase the effectiveness of the use of Isotretinoin.
The use of isotretinoin for the correction of wrinkles –
But the retinoid isotretinoin can be used not only systemically (orally).
There are a small number of drugs with isotretinoin for external use, which were initially used exclusively for the treatment of acne and pimples, but later these drugs began to be used to correct the symptoms of photoaging. As in the case of the retinoid tretinoin, preparations with isotretinoin also help to increase skin elasticity and reduce the depth of wrinkles. What effects do external forms of isotretinoin cause in the skin:
- Peeling effect - the thickness of the superficial stratum corneum of the epidermis decreases (due to exfoliation of dead skin cells). This evens out skin tone and texture, leaving skin looking more youthful and radiant—like you've had a few superficial chemical peels.
- Increasing the thickness of the deep layers of the epidermis - isotretinoin affects stem keratinocytes located at the basement membrane, increasing the rate of their division and differentiation. This leads to an increase in the thickness of the deep layers of the epidermis, consisting of living keratinocytes. As a result, the hydrophobicity of the epidermis increases, which contributes to less evaporation of moisture from the surface of the skin. In addition, it prevents skin photoaging.
- Stimulation of the production of collagen and hyaluronic acid - isotretinoin affects not only the epidermis, but also the dermis. It promotes the proliferation (reproduction) of fibroblasts, and also significantly stimulates their activity, which leads to an increase in their production of collagen, elastin and endogenous hyaluronic acid. This leads to an increase in the thickness of the dermis, a decrease in the depth of wrinkles, and an increase in skin elasticity. It is known that thicker skin is less susceptible to the aging process.
Optimal concentrations of external forms of Isotretinoin –
There are a number of clinical studies where scientists have determined the optimal concentration of isotretinoin for the treatment of photoaging.
1) “Armstrong RB, Lesiewicz J, Harvey G et al. Clinical panel assessment of photodamaged skin treated with isotretinoin using photographs. Arch Dermatol 1992; 128:352–6.” 2) “Sendagorta E, Lesiewicz J, Armstrong RB. Topical isotretinoin for photodamaged skin. J Am Acad Dermatol 1992; 27:S15–18.”
In these studies, the concentration of Isotretinoin was increased from 0.05% at the beginning of the study to 0.1% at the end of the study. Despite the increase in concentration, the drug was well tolerated by patients without causing significant skin irritation. As a result of the treatment of photoaging skin with 0.1% Isotretinoin, the skin condition gradually improved throughout the 36-week treatment, and a decrease in the depth of wrinkles and fine lines was achieved.
3) The study “Maddin S, Lauharanta J, Agache P et al. Isotretinoin improves the appearance of photodamaged skin: results of a 36-week, multicenter, double-blind, placebo-controlled trial. J Am Acad Dermatol 2000; 42:56–63.” In this study, a combination of 0.05% Isotretinoin plus SPF sunscreen was used to treat photoaging. The result was that the condition of skin with visible photodamage was significantly improved, which was recorded using profilometry.
Conclusions: if you are interested in preventing skin photoaging, it is best to use a 0.05% concentration in combination with sunscreen. If you want to achieve an increase in skin elasticity and a decrease in the depth of wrinkles, then the main treatment should be carried out using a 0.1% concentration (it is better to use a 0.05% concentration for the first month so that the skin gets used to retinoids).
Isotretinoin has a delayed effect - it will take at least 8-12 weeks before you notice any positive changes, although the first positive effect associated with improved skin tone and texture will be noticeable after 4-6 weeks. It must be admitted that abroad isotretinoin is used for the correction of photoaging much less frequently than other types of retinoids - tretinoin or pure retinol.
Preparations with isotretinoin for external use –
- “Retinoic ointment” (Fig. 8) – is available with an isotretinoin concentration of 0.05% or 0.1%. The cost will be from 300 rubles for a 15 g tube. About a tenth of the volume is ethyl alcohol, so you should not use this drug if you have dry and/or sensitive skin. In principle, the manufacturer writes in this regard that this drug is intended for the treatment of acne in patients with oily skin.
- "Retasol" (Fig. 9) - is a solution for external use, with an isotretinoin concentration of 0.025%. But keep in mind that this drug also contains alcohol, but in less quantity than retinoic ointment. In addition, the drug contains propylene glycol, which may cause irritation in patients with sensitive skin. Cost from 400 rubles per 50 ml bottle.
Composition of tablets, ointments, facial gel
The active ingredient in each form is isotretinoin. This component is active regardless of whether it is external or internal. The facial gel contains an additional component - Erythromycin. It increases the permeability of components through the skin, increases efficiency and allows you to achieve the desired results in a shorter period of time.
Additional substances differ in each of the release forms described above; they will be presented in the table:
| Pills | Ointment | Gel |
|
|
|
Almost all tablets and capsules whose active ingredient is Isotretinoin have a similar composition. Only minor differences may occur. The texture of ointment and gel differs significantly from each other. Due to the substances that make up the ointment, its consistency is very dense and heavy.
This should be taken into account during long-term and frequent use for skin prone to inflammation. Incorrect application threatens to clog the pores, which provokes the appearance of new inflammatory elements on the skin.
Reviews
Opinions about the drug are mixed. Almost everyone expresses their dissatisfaction with the side effects of the drug. In reviews of Isotretinoin, users ironically say that before there was one problem, but now there are several.
But those who had a short course are satisfied with the result. Young women who are desperate to find an effective remedy are doubly satisfied - an excellent result at a low cost. Young people who do not understand medicines and the intricacies of their use are satisfied with the result. They especially note the ease of use and the ability to independently adjust the dosage based on weight.
pharmachologic effect
Isotretinoin (the instructions for use contain a complete description of the pharmacological action of the drug) has a wide spectrum of action. Isotretinoin is considered a derivative of Vitamin A. There are some similarities in their structure, therefore, during treatment with Isotretinoin preparations, additional intake of vitamin supplements containing vitamin A is prohibited.
Due to the structural similarity, this can lead to overdose.
The exact mechanism of the effect of Isotretinoin on the skin and the entire human body has not been fully identified. It is believed that the positive effect is achieved by suppressing the activity of the sebaceous glands and changing the structure of sebum. Under the influence of this substance, skin sebum changes its consistency, it becomes more liquid. This is why skin pores are not clogged.
In addition, a course of treatment with Isotretinoin promotes a histological reduction in pore size. Excess sebaceous secretion causes the development of inflammatory elements on the skin. Too thick sebum, produced by the sebaceous glands in excess, leads to the formation of comedones.
As a result, acne of various types appears on the skin, as well as closed comedones, called “blackheads”. The action of Isotretinoin is aimed at suppressing this process. Medications containing Isotretinoin help normalize the process of cell differentiation. As a result, bacterial colonization of the sebaceous duct is suppressed.
Isotretinoin, for both internal and topical use, acts in three ways:
- The product reduces the size of the sebaceous glands. Excessive sebum production enlarges the pores, creating a gap in which sebum accumulates. By normalizing the activity of the sebaceous glands, it is possible to get rid of not only inflammatory elements, but also enlarged pores.
- Comedolytic action. The active substance is aimed at dissolving the substrate of the fat plug, which causes clogging of pores. Due to this action, it is possible to prevent the appearance of new acne, as well as eliminate old ones.
- Reducing the thickness of the surface epidermis layer. This action applies only to topical retinoids. The effect is due to the fact that when applied topically, Isotretinoin has a mild irritant effect. As a result, the stratum corneum begins to peel off and gradually renew itself. Dead cells disappear, the pores open, so the therapeutic drug penetrates them more effectively. When taking Ichotretinoin orally, peeling of the skin is also observed, but this is not due to an irritating effect, but to the fact that the epidermis becomes very dry.
Retinoic ointment based on isotretinoin is prescribed to treat acne and eliminate age-related skin changes. Since local Isotretinoin has a peeling effect, the skin becomes clean, its tone is evened out, and overall the face looks healthy and uniform.
Isotretinoin also increases the rate of division of epidermal stem cells. This helps the skin to retain moisture better and is not at risk of dehydration. Gradually, existing wrinkles are filled from the inside, which significantly reduces their severity.
https://youtu.be/b7sSlpmUw-0
Introduction
“Isotretinoin is a godsend for patients with scarring acne,” noted Stephen R. Feldman in his editorial commentary.
Isotretinoin, a derivative of vitamin A (retinol), is widely used in the treatment of acne vulgaris and has many pharmacological properties that affect the formation of the epidermis, sebaceous glands and collagen. Isotretinoin's tendency to interfere with these functions has led to questions about the potential for poor wound healing, keloids, and hypertrophic scars, particularly in patients undergoing dermatosurgical procedures while taking this drug. This has led to the legislative recommendation that cosmetic and dermatosurgical procedures should be avoided during and after taking the drug for 6–12 months. This recommendation is debated and there are differences of opinion on this issue.
This study reviews the current literature on this issue to determine whether the recommendation is based on evidence and whether change is warranted.
Literature search
A PubMed search was conducted on October 9, 2021 using the keywords “isotretinoin”, “isotretinoin side effects”, “isotretinoin” and “laser”, “isotretinoin” and “surgery”, “isotretinoin” and “keloid”, “isotretinoin” and "Healing", "Isotretinoin" and "Hypertrophic Scarring". A total of 403, 62, and 27 articles were found for “Isotretinoin” and “Surgery,” “Isotretinoin” and “Wound Care,” and “Isotretinoin” and “Laser,” respectively. Of these, 26 English language articles, which consisted of reports and studies related to isotretinoin and procedures, were considered relevant and included. Studies can be analyzed into two categories:
- Early studies that suggested a tendency for poor wound healing, development of keloids and hypertrophic scars in patients taking isotretinoin, either spontaneously or after dermatosurgical procedures.
- More recent studies seem to suggest that this trend is generally not noticed.
Several early studies documented the spontaneous appearance of keloids during isotretinoin treatment.
Ginarte et al documented the “spontaneous appearance” of a keloid on the trunk in a 16-year-old boy who was started on oral isotretinone 0.5 mg/kg/day. The keloid developed within 4 weeks of starting the drug and continued to progress despite discontinuation of isotretinoin. At 2-year follow-up, the keloids persisted despite intrafocal triamcinolone.
Dogan (2006) reported a patient who had no previous history of keloid but developed a truncated keloid after 8 weeks of oral isotretinoin 40 mg/day. In a study of 21 patients by Guadanhim et al, spontaneous occurrence of keloid was reported in one case.
Subsequently, several studies also reported keloids in isotretinoin-treated patients undergoing dermatosurgical procedures. Zachariae (1988) reported three cases. The first case was described after exposure to an argon laser on the cheek. In this case, the keloid developed after 8 weeks. In the other two cases, keloids developed 8 weeks and 6 months after dermabrasion.
Rubenstein et al presented a case series of 6 patients who underwent dermabrasion for acne scarring, 3 of whom were still taking isotretinoin and 3 of whom had stopped taking isotretinoin 5 to 6 months earlier. The dose of isotretinoin was 0.5–1 mg/kg/day for a treatment duration of 4 to 14 months. All of these patients developed keloid scars 1 to 3 months after dermabrasion. Topical and intrafocal corticosteroids have resulted in some clinical improvement or resolution of keloids.
The above studies, although small, highlight the possibility of keloids developing in patients treated with isotretinoin and subsequently lead to the recommendation that the procedures should not be performed in such patients for 6–12 months. However, as can be seen, the studies were few in number, had small sample sizes, many were case reports, and all were reported at a time when lasers were in their early stages of development.
Adverse effects have developed in response to aggressive procedures such as argon laser and dermabrasion, which are rarely performed in current practice. The recommendation also applies to all procedures, regardless of invasiveness (or lack thereof). The profile of treatments has changed over time, with minor procedures such as microdermabrasion, superficial peels and microneedling being increasingly performed. Laser machines have become safer, more accurate and less invasive. It is therefore interesting to examine more recent studies regarding each individual procedural intervention in patients taking isotretinoin.
Dermabrasion
It is interesting to note that in contrast to the aforementioned studies documenting the development of keloids, several recent studies have confirmed the safety of this procedure in this group of patients. As early as 1985, Roenigk et al documented a case series of 9 patients with acne scars who underwent full facial dermabrasion. Of these 9 patients, 4 had stopped taking isotretinoin 2–11 months earlier and 5 were still taking isotretinoin at the time of dermabrasion. The average dose of isotretinoin for all patients was 0.5–1 mg/kg/day. All patients showed normal wound healing.
Bagatin et al documented a prospective cohort study of 7 patients (six women, 1 man) who took isotretinoin for at least 1 month with a dose range of 10–40 mg/day. For each patient, a 1 cm treatment area was selected and manual diamond dermabrasion was performed. No complications, including hypertrophic or keloid scars, were observed in these patients during the 6-month follow-up period.
Picosse et al. reported results in 10 patients (4 women, 6 men) who underwent a medium-depth chemical peel with Jessner's solution and 35% trichloroacetic acid on the entire face, followed by manual dermabrasion with sterile sandpaper on the area with scars. All patients completed isotretinoin treatment for acne 1-3 months ago with a minimum total dose of 122 mg/kg per patient. No signs of hypertrophic or keloid scarring were found in any of the treated patients.
In a more recent study, Mahadevappa et al performed fractional erbium laser resurfacing (which is the laser equivalent of mechanical dermabrasion) on the face for chest keloids while taking isotretinoin. Postoperative follow-up for one year did not reveal any keloids on the face, and the existing chest keloid remained unchanged.
It is somewhat difficult to imagine why early studies with dermabrasion should document keloids in contrast to more recent studies. Such cases may represent a particular response to oral isotretinoin. However, as stated earlier, dermabrasion is rarely practiced nowadays, and therefore it is perhaps a situation that is rarely encountered in modern practice.
Laser hair removal
Table 1 shows various studies on laser hair removal and their side effects. Khatri (2004) performed diode hair reduction in 7 patients taking isotretinoin. No side effects, including keloids, were reported after 1 month.
Cassano et al. (2005) performed diode facial hair reduction in 6 patients taking isotretinoin. Again, no side effects, including keloids, were observed during the 4-year follow-up period. In a more recent study in 2006, Khatri and Garcia used long-pulse beams to epilate facial hair in 6 patients taking isotretinoin. Here, too, no keloids were reported over the next 6 months. Khatri, in another 2009 study, performed long-pulse neodymium laser facial hair removal on 11 patients taking isotretinoin. No keloid was reported after 12 weeks of follow-up.
Chandrashekar et al. (2014) published a retrospective study of hair removal in 5 cases. The devices used were a 980 diode with a long-pulse 1064 nm neodymium laser, intense pulsed light, and a follow-up period of 24 weeks. No adverse events were recorded.
Mahadevappa et al. (2016) performed 26 sessions of safe hair removal, of which 9 using intense pulsed light, 4 using a long-pulse neodymium laser, and 13 using a diode laser. The follow-up period was 1 year, and no keloids were reported.
Table 1: Laser and light hair removal in patients receiving isotretinoin
| Author | Purpose of publication | Number of patients | Oral isotretinoin | History of hypertrophied scar | Duration of observation | Laser application area | Operative and postoperative complications | Limitations of the study |
| Khatri 2004 | Diode hair removal in patients receiving oral isotretinoin | 7 | When taking isotretinoin 63 mg/day. within 4 months | No | 1 month | Axillary folds and pubis | Blisters in one patient that resolved after a week | Small sample |
| Cassano et al., 2005 | Diode hair removal in patients receiving oral isotretinoin | 6 | While taking isotretinoin | No | 4 years | Face | Erythema, crusting, resolved after a few days | Small sample |
| Khatri and Garcia 2006 | Long-pulse laser radiation | 6 | When taking isotretinoin 40-80 mg/day | No | 6 months | Axillary folds, pubis, face | No | Small sample |
| Khatri 2009 | Hair removal with a long-pulse neodymium laser during treatment with isotretinoin | 11 | Taking isotretinoin except on laser therapy days | No | 12 weeks after laser therapy course | Face and extrafacial zones | No | Retrospective case series |
| Chandrashekar et al., 2014 | Hair removal with neodymium laser/IPL during treatment with isotretinoin | 5 | Taking isotretinoin 0.5 mg/kg | No | Face | No | Study with control group | |
| Mahadevappa et al., 2016 | Laser/IPL hair removal with isotretinoin treatment or after it | 26 | Taking isotretinoin 2-110 mg/kg | No | Up to 1 year | Face | No | No control group |
In summary, these studies indicate that hair removal using lasers of all wavelengths and intense pulsed light systems is safe for patients taking isotretinoin.
Table 2: Lasers for post-acne scars
| Author | Purpose of publication | Number of patients | Oral isotretinoin | History of hypertrophied scar | Duration of observation | Laser application area | Operative and postoperative complications | Limitations of the study |
| Yoon et al., 2014 | Fractional laser therapy 1550 nm | 35 patients and 18 in the control group | Preceded by taking isotretinoin 10 mg/day, 7 sessions of laser therapy | No | 7 months after the end of laser therapy | Face | No keloids | Study with control group |
| Kim et al., 2014 | Fractional carbon dioxide laser facial peeling in patients receiving isotretinoin | 20 | 10-60 mg/day. | No | 6 months after the end of laser therapy | Face | No keloids | Retrospective study |
| Khatri et al., 2015 | Laser peeling for those receiving isotretinoin: Fractional 1540 nm Fractional 2940 nm Deep 2940 nm | 1 | 80 sg/day. | No | 6 months | Lower back | Scars in the deep peeling area after 6 months | Research based on medical records |
| Mahadevappa et al., 2016 | Surgical outcome in patients with previous exposure to oral isotretinoin after: a) Fractional erbium laser-102 sessions b) Fractional carbon dioxide laser – 19 sessions c) Deep facial peeling with fractional carbon dioxide laser – 19 sessions | 183 | 2-110 mg/day. | No | Up to 1 year | Face/ nose | Pigmentation after 15 carbon dioxide laser peeling sessions, no keloids | No control group |
Ablative, fractional ablative, and non-ablative lasers affect neocollagen synthesis and are used to treat surgical scars. Table 2 reviews four PubMed articles from 2014.
Yun et al. (2014) performed 3550 nm infrared laser therapy on 35 patients receiving isotretinoin for the treatment of acne scars. The control group consisted of 18 patients who did not receive isotretinoin. Both groups achieved a mean score of 3.1 after laser sessions without any keloids or hypertrophic scars.
A retrospective study by Chandrashekar et al (2014) included 25 cases (0.5 mg/kg/day isotretinoin) and a control group of 25 cases who did not take isotretinoin. Both groups received fractionated carbon dioxide laser treatment. Follow-up at 24 weeks did not reveal any keloids or hypertrophic scars in any of the groups. Kim et al. (2014) performed fractional carbon dioxide laser treatment on the face in a retrospective study on 20 cases in patients taking 10–60 mg/day isotretinoin. Follow-up after 6 months showed no side effects.
Mahadevappa et al. conducted a prospective study in 183 patients taking isotretinoin at doses ranging from 2 to 110 mg/kg. Laser facial resurfacing (both conventional full-face resurfacing and fractional carbon dioxide and erbium lasers) was performed on 45 patients with a 1-year follow-up. None of the patients developed a hypertrophic scar or keloid despite taking isotretinoin.
Khatri et al treated the lower back with three different lasers in a patient who was taking isotretinoin 80 mg/day. After 6 months, no hypertrophic scars were detected.
In summary, studies using conventional full-face and fractional lasers for acne scarring appear to indicate the absence of side effects and the safety of these procedures in patients taking isotretinoin.
Isotretinoin and chemical peels
Chemical peeling is performed to correct scars, reduce pigmentation and treat active acne, as well as photoaging of the skin. Superficial peels are commonly used, and there have been several studies documenting the use of peels in isotretinoin patients. There have been no reports of deep peels in patients treated with isotretinoin, possibly due to the lack of use of deep peels in current practice.
Picosse et al performed 10 medium-depth peels using Jessner's solution and 35% trichloroacetic acid followed by dermabrasion with sandpaper. No keloid was reported, although 3 cases had keloid before peeling.
The study conducted by Mahadevappa et al included 4 sessions of trichloroacetic acid peel, 30 sessions of salicylic acid peel, combination peel in 65 sessions and finally glycolic acid peel in 147 sessions. A keloid formed on the chest only in one case during peeling with glycoic acid. Although the safety of these peels appears to have been established by these studies, the development of keloid on the chest with facial peels cannot be explained. In 2014
Gerber et al reported a case of severe hyperpigmentation and scarring following a 70% glycolic acid peel in a 34-year-old woman who stopped taking isotretinoin 10 weeks before the peel. The authors noted that “the exact mechanism of atypical reepithelialization and scarring due to isotretinoin remains unclear. Oral retinoids can cause disruption of the stratum corneum and thus increase the depth of penetration of glycolic acid.
Hyperpigmentation, which is a known side effect of peels, may also be associated with increased sensitivity to sunlight after the peel in a patient with thinning skin due to isotretinoin. This report of hyperpigmentation with scarring suggests that caution should be used when performing glycolic acid peels in these patients, even if other peels, such as salicylic acid peels, appear safe.
Isotretinoin and radiofrequency procedure
A radiofrequency device is used to excise, coagulate, or remove skin lesions. In addition, it is used for collagen remodeling using dermal needles or epidermal bipolar or tripolar electrodes.
Chandrashekar et al. performed 13 treatments of acne scars using a radiofrequency device in patients taking 0.5 mg/kg oral isotretinoin. No one experienced any complications. In a study by Mahadevappa et al., radiofrequency ablation of a nevus was performed in a patient receiving a cumulative dose of 4000 mg isotretinoin who later developed a keloid at the ablation site. The exact cause has not been established.
Isotretinoin and other treatments
Other common procedures performed in dermatology include skin biopsy, excision, comedonal removal, acne scar lifting, microneedling for scars, microdermabrasion, and undercutting. Mahadevappa et al. 27 such interventions were performed in 11 cases. No one had any complications. This study also included 18 patients who underwent 44 sessions of microdermabrasion with aluminum crystals on the face. No side effects were reported. In a study by Chandrashekar et al, 12 cases used microneedles in the isotretinoin group and compared with 12 cases in the control group. After 24 weeks, no keloids or scars were noted.
Should the recommendations against surgery in patients taking isotretinoin be changed?
The above review overwhelmingly demonstrates that, with the exception of a few studies in small numbers of patients, the risk of hypertrophic scarring, keloid formation, and delayed wound healing is not observed after most dermatologic procedures. Therefore, the recommendation to avoid surgical procedures in patients treated with isotretinoin was, in our opinion, based on inadequate evidence and lack of relevance to current practice.
The studies on which this recommendation was based were small, of low quality, with small numbers of patients. The evidence can be classified as level 3 and the level of recommendation as level D (Harbour and Miller revised grading system)
Additionally, those studies that were documented in the early 1980s and 1990s relied on aggressive procedures such as dermabrasion, which are rarely performed today.
The recommendation was made at a time when laser technology and other minor procedures such as superficial peels and microdermabrasion were not yet fully developed. It should also be emphasized that in today's practice the procedures are much less invasive and the application of such a recommendation to these minimally invasive procedures should be questioned.
Therefore, the relevance of such evidence must be questioned, and the authors strongly believe that such a recommendation based on such low quality studies would never have been accepted by current standards of evidence-based practice had it been made. The authors believe that the recommendation discourages the use of procedures in such patients and creates fear among physicians of potential medicolegal situations. This was confirmed by a recent survey of nationally recognized laser surgery experts regarding the treatment of patients taking isotretinoin or having completed such treatment for 6 months. In this report, the maximum number of respondents (70%) confirmed that medico-legal concerns had a significant influence on their decision making regarding this group of patients, as opposed to concerns about atypical or poor wound healing (69%) and scars (66%). and hypertrophic or keloid scars (49%). What was interesting was that 76% of respondents had never seen any complications in their own clinical practice.
Thus, this recommendation only serves to deny patients safe treatment and instills unnecessary fear in the minds of physicians. As this review shows, most procedures in modern practice are less invasive, and the recent studies reviewed here, although admittedly small, suggest the relative safety of the procedures in this group of patients. It is therefore time to present a new recommendation on this issue. A recent publication of guidelines based on a systematic review of 32 relevant publications involving 1485 procedures found that there was insufficient evidence to support delaying manual dermabrasion, superficial chemical peels, skin surgery, laser hair removal and fractionated ablative and non-ablative laser procedures in patients who are currently receiving or have recently completed isotretinoin therapy.
The publication also stated that mechanical dermabrasion and fully ablative laser are not recommended during treatment with systemic isotretinoin. The review suggests that clinicians and patients should have an evidence-based understanding of the known risks of cutaneous surgical procedures before they are performed in the setting of systemic isotretinoin therapy. For some patients and some conditions, informed decision-making can lead to earlier and potentially more effective interventions.
The authors strongly agree with the above views and believe that the recommendation is inappropriate in current practice based on the current evidence available and should be withdrawn. The authors would also suggest that, if necessary, at the discretion of the physician, a test treatment be performed in individual patients before the main one.
Conclusion
The authors believe that recommendations to avoid procedures such as fractional resurfacing with carbon dioxide and erbium lasers, fractional infrared lasers-1550 nm, 1540 nm, laser hair removal, microdermabrasion using aluminum crystals, microneedling, microneedling using radiofrequency, scalpel excision surgery, skin biopsy in patients taking or who have taken isotretinoin is based on weak and limited data. Rather than avoiding these procedures, a preliminary test procedure to verify the safety of the intervention may be performed at the discretion of the treating physician.
Indications for use
Instructions for use imply the use of the drug Isotretinoin for the treatment of severe forms of acne, for the treatment of stage 3-4 acne.
Use at stages 1-2 of acne is not advisable, since the drug has many side effects for the whole body; for the treatment of mild forms of acne, it is better to give preference to external agents. The use of topical retinoids for mild acne is not prohibited.
In addition, Isotretioin is prescribed in the following cases:
- Seborrheic type dermatitis.
- Perioral type dermatitis.
- Rosacea.
- Subcutaneous mite (Demodex).
- Risk of formation of nodular cystic scars.
It is worth noting that isotretinoin for internal use can only be prescribed by a doctor.
You must first ensure that there are no contraindications for use. To do this, you will need to take a blood test, and diagnostics of liver parameters is also required. Before starting treatment, women must ensure that they are not pregnant, as Isotretinoin has a teratogenic effect.
Contraindications
Isotretinoin is an aggressive drug, so before starting treatment it is very important to read the instructions for use in detail. This is especially true for tablets and capsules for internal use.
Internal use of Isotretinoin is contraindicated in the following cases:
- Individual intolerance and sensitivity to the composition of the pharmaceutical product.
- Gestation and lactation period.
- Pregnancy planning.
- Severe kidney and liver dysfunction.
- High concentration of vitamin A in the blood.
- The presence of neoplasms of a malignant nature.
- High fat content in the blood.
- Combination with tetracycline antibiotics.
Caution: Oral isotretinoin is used for the following conditions:
- Diabetes mellitus of any type.
- Frequent consumption of alcoholic beverages.
- Disturbances in fat metabolism.
- Abnormally high body weight.
- Depressive and anxiety states.
Local retinoids are contraindicated during pregnancy and lactation, when taking tetracycline antibiotics, and are also not recommended for application to areas where the integrity of the skin is compromised.
Why does acne occur?
The content of the article
Acne is a group of diseases associated with disorders of the sebaceous glands. The most popular form of acne appears to be acne vulgaris, which usually affects teenagers and some adults. As a result of hormonal changes, the sebaceous glands produce excessive sebum. In addition, we often encounter increased keratosis of cells that clog the excretory ducts, which contributes to the formation of acne and purulent pustules.
Instructions for use of Isotretinoin gel for acne
Dermatologists recommend using isotretinoin in gel form for mild or moderate acne.
The gel is applied following the following sequence of actions:
- Carefully cleanse the skin of impurities and decorative cosmetics. For cleansing, only gentle products that do not contain aggressive components should be used.
- Apply the drug to the inflammatory elements on the skin; the gel layer should be thin. The product is applied locally to the inflammation, as well as to the surrounding tissue. In mild and medium stages, there is no need to apply the product to the entire face.
- The gel is applied 1-2 times a day. It is advisable to leave it overnight.
- It is necessary to allow the gel to be completely absorbed into the skin. After the stickiness disappears, you can apply decorative cosmetics. Cosmetics must be non-comedogenic.
The duration of treatment is determined by a dermatologist, taking into account the stage of the pathological process. The average course duration is 2 months.
How to use the ointment?
Isotretinoin-based ointment is intended for topical application. It is used for mild or moderate stages of acne. In some cases, it may be prescribed for severe acne as an additional remedy.
The product is applied to the inflammatory elements 2 times a day. It is not recommended to combine it with decorative cosmetics, as the ointment has a peeling effect. Under its influence, the protective layer of the epidermis becomes thinner, which increases the likelihood of irritation and redness. In addition, foundations increase the severity of peeling.
Isotretinoin. The instructions for use state that you should not apply makeup after the drug.
The average duration of treatment is 5-6 weeks. The ointment can be applied for isolated inflammations; it must be applied locally. To eliminate wrinkles, it is recommended to apply the ointment once a day, every other day. In case of severe peeling, reduce the number of uses.
Drug for signs of skin photoaging
Judging by the reviews and instructions, Isotretinoin has not only therapeutic properties. It makes the skin more elastic, soft, and helps reduce the depth of wrinkles. There have been no clinical studies confirming such effects. However, the drug does have some cosmetic effects.
- Peeling effect. Under the influence of the drug, the keratinized upper layer of the epidermis is eliminated. Blood supply and nutrition of tissue cells improves. Skin looks healthier and younger.
- Activation of the process of stem cell division. The drug helps accelerate the processes of division and transformation of the structural forms of stem keratinocytes into mature ones. The hydrophobic properties of the epidermis improve, the skin is well moisturized.
- Stimulation of the production of elastin, collagen and hyauronic acids.
Tablet regimen and dosage
Isotretinoin (the instructions for use contain a detailed description of the treatment regimen) must be taken in a strictly defined dosage. But it is worth considering that only a dermatologist can prescribe an exact treatment regimen after conducting all the necessary diagnostic examinations. The dosage depends on the age, weight of the patient, and the degree of acne.
The average dosage is 0.5 mcg per 1 kg of patient weight. If there are no side effects, the dose is increased to 1 mg. The tablets are taken orally while eating. It is advisable to take a small amount of oil together, since Isotretinoin is a fat-soluble element.
The treatment regimen can be adjusted if side effects are present, as well as if the therapeutic effect is weak.
The result appears within 4-7 weeks from the start of treatment. To achieve stable remission, treatment is carried out for 4-6 months. The main task when taking drugs based on Isotretinoin is to gain a cumulative dose over the entire period of treatment. On average it is 120 mg per 1 kg of weight. It is strictly not recommended to carry out such calculations on your own, as this should be done by a doctor.
When you start taking capsules or tablets, the number of inflammatory elements may increase; this does not require discontinuation of the drug and is considered an absolutely normal phenomenon. In case of exacerbation, it is allowed to reduce the established dosage.
Chemical properties
Under natural conditions, Isotretinoin is synthesized in the human body in small quantities. The substance is a trans isomer, which is called vitamin A. Some time after the formation of this compound, it interacts with internal microflora and turns into trans-retinoic acid .
Artificially synthesized 13-cis-retinoic acid is an orange or orange-yellow powder. Molecular weight of the compound = 300.4 grams per mole.
The drug is produced in the form of capsules or tablets for oral administration, ointment bases, and suppositories for rectal administration.
Features of use during pregnancy
Isotretinoin (the instructions for use strictly prohibit taking the drug internally or using it externally during pregnancy and lactation) is used only when pregnancy is definitely not possible.
Since the drug has a teratogenic effect, it is prohibited for women who are planning a pregnancy. In this case, isotretinoin is not used even in severe stages of acne. Internal use of drugs whose active substance is Isotretinoin is a direct indication for abortion if pregnancy does occur.
Drugs containing (Analogs)
Level 4 ATC code matches:
Adaklin
Isotrexin
Adapalene
Differin
Effezel
Klenzit
Retinoic ointment
Tretinoin
Retin A
We see
Structural analogues of this substance: 13-cis-Retinoic acid , Verocutan , Retasol , Retinoic ointment 0.05 and 0.1%, Sotret , Acnecutan , Isotretinoin , Retinoic ointment 0.01%, Roaccutane .
Side effects
The drug has many side effects that affect the entire body. All of them will be presented in the table below depending on the frequency of occurrence.
| Often | Rarely |
|
|
If any side effects occur, it is recommended to immediately consult a specialist. In case of pronounced negative reactions, the drug must be discontinued completely. In all other cases, side effects are almost always reversible.
The principle of therapeutic action of isotretinoin
Preparations containing isotretinoin have the following pharmacological effects:
- normalize the processes of differentiation (development) of sebaceous gland cells;
- inhibit the excessive formation of superficial cells lining the excretory ducts of the glands;
- suppress the formation of sebum;
- facilitate the removal of sebaceous gland secretions to the surface of the epithelium.
Due to this, the amount of sebum becomes smaller, the composition is normalized, secretion is facilitated, and inflammatory processes are suppressed.
Isotretinoin has the following therapeutic effects:
- antiseborrheic;
- anti-inflammatory;
- sebostatic (inhibition of the synthesis of skin secretions);
- immunomodulatory;
- keratomodulating (normalizing the balance of substances and skin cells);
- regenerating.
Systemic isotretinoin is absorbed in the intestine after taking the capsule orally. However, its bioavailability is low. A larger amount of the drug enters the bloodstream while ingesting food. It travels with the blood to the liver, where it is metabolized to form tretinoin. It is excreted from the body with urine and feces.
Interaction
It is necessary to stop taking vitamin complexes containing vitamin A, as this will lead to overdose symptoms. It is forbidden to take the drug together with tetracycline antibiotics, as this leads to an increase in intracranial pressure.
It is not recommended to take with hormonal drugs that contain a large dose of progesterone.
During treatment with Isotretinoin, it is necessary to avoid drinking alcoholic beverages, as they significantly increase the toxic effect on the body.
In what cases is Isotretinoin contraindicated?
Increased levels of vitamin A in the body can cause serious health problems. Isotretinoin is not recommended for use in the following cases:
- Planned or confirmed pregnancy.
- Breastfeeding period.
- Liver failure.
- A pathological condition caused by an excess of retinol (vitamin A) in the body.
- Severe hyperlipoproteinemia.
- Pathologies of the rectum (proctitis, hemorrhoids).
- Diabetes.
- A mental disorder characterized by a constant decrease in mood.
If there is at least one pathology, it is recommended to replace Isotretinoin with analogues or a completely different drug.
Also, the drug is not prescribed for treatment with antibacterial drugs with a condensed four-cyclic system of chemical structure (tetracyclines).
special instructions
Only doctors who are familiar with the effects of systemic retinoids can prescribe oral medications based on isotretinoin. Self-medication is strictly prohibited. During the course of taking the drug, the patient is prohibited from donating blood.
During treatment, it is necessary to closely monitor the condition of the body and regularly take blood tests to monitor liver parameters. In order to reduce peeling and irritation on the skin, it is recommended to additionally use moisturizers with a non-comedogenic composition.
Reviews of Isotretinoin
Reviews about this product vary greatly. Doctors most often speak well of the medicine and often prescribe it for acne of varying severity. Patients have divided opinions about the effectiveness and safety of using this drug.
Here are some reviews about capsules and tablets based on Isotretinoin:
- “... The doctor prescribed this drug to me for acne. I took it for a year. Now 1.5 years have passed and the effect still persists. The most difficult thing during treatment was choosing the right dosage; among the side effects, I most often felt dry lips, skin on the arms, hands and feet”;
- “... I’ve been taking Isotretinoin capsules for 2 months now. At first, the skin on my hands was very peeling and my lips were dry. Now I bought a good moisturizer and the dryness has gone away. After 14 days of treatment, the face became much cleaner, now there are practically no rashes”;
- “... I didn’t like the drug at all, during treatment my hair fell out, my skin peeled severely, my lips dried out so much that it was impossible to smile, I had a headache, and suffered from insomnia. After 1.5 months of suffering, I changed the doctor and switched to other medications.”
Cheap and expensive analogues
Isotretinoin comes in many forms, but prices vary greatly:
| Drug name | Price |
| Capsules Roaccutane 10 mg | 2000 rub. |
| Capsules Sotret 10mg | 1100 rub. |
| Capsules Acnecutan 8 mg | 1500 rub. |
| Retinoic ointment | 300 rub. |
| Isotretinoin gel | 450 rub. |
| Isotretinoin solution | 320 rub. |
| Isotretinoin capsules 10 mg | 1450 rub. |
All analogues have a similar composition and identical principle of action. The difference in their composition is not significant; it does not affect the final result of treatment.
Pharmacodynamics and pharmacokinetics
The medicine affects the terminal differentiation of keratinocytes and normalizes the processes of regeneration and OVR with the participation of vitamin A . The substance affects the internal microflora, disrupting the expression of the gene that is responsible for the synthesis of certain types of protein. Under the influence of this chemical compound, the production of sebaceous glands is suppressed and their number in general decreases.
Isotretinoin, when taken orally, has variable absorption capacity and low bioavailability. When eating at the same time, these indicators increase 2 times. The drug reaches its maximum concentration 2-4 hours after administration. The degree of binding to blood plasma proteins is about 99%.
Metabolism of the drug occurs in the liver, with the formation of 3 active metabolites: 4-oxo-isotretinoin , 4-oxo-retinoin and tretinoin + less significant metabolites, including glucuronides . The metabolic processes of both zotretinoin and tretinoin are closely related to each other. The enterohepatic circulation has a significant influence on the process. Metabolism occurs with the participation of CYP2C8 , CYP3A4 , CYP2B6 and CYP2C9 of the cytochrome P450 system . The half-life of the substance is approximately 20 hours, its metabolites - up to 30 hours. The medicine is excreted through the kidneys and bile.
Price of the drug in pharmacies in Moscow, St. Petersburg and regions
In addition, the cost depends on the region of sale.
Using Roaccutane as an example, you can notice the difference in price:
| Moscow and Moscow region | 2000 rub. |
| Saint Petersburg | 1800 rub. |
| Yaroslavl region | 1780 rub. |
| Vologda Region | 1900 rub. |
| Krasnodar region | 2100 rub. |
| Ryazan Oblast | 1650 rub. |
Any form of the drug can be purchased at an online pharmacy. The price depends on the dosage and form of the medication.
Reviews from dermatologists about the effectiveness of the product
Dermatologists note that to achieve maximum results, it is important to choose the right treatment regimen. This will help avoid unwanted consequences.
Isotretinoin is the most effective treatment for acne, but it is very important to follow the instructions for use. It is effective even when other drugs do not produce the desired result.
Author of the article: Victoria Kolenova
Article design: Oleg Lozinsky
Precautionary measures
The instructions for use for Isotretinoin contain clear instructions regarding measures to help avoid problems when using a dermatotropic agent.
During treatment, it is necessary to monitor lipid levels and liver function. Patients with diabetes should check their blood glucose levels more often.
If side effects occur, treatment is stopped. To avoid hypervitaminosis A, Isotretinoin is not prescribed to patients taking retinoid drugs.
During therapy, patients wearing contact lenses should temporarily use glasses. If a woman becomes pregnant during treatment, the drug should be discontinued.