Dosed nasal spray 50 mcg/1 dose
in the form of a white or almost white suspension.
Excipients: dispersed cellulose (microcrystalline cellulose treated with carmellose sodium) - 20 mg, glycerol - 21 mg, citric acid monohydrate - 2 mg, sodium citrate dihydrate - 2.8 mg, polysorbate 80 - 0.1 mg, benzalkonium chloride (in the form of a 50% solution ) - 0.2 mg, purified water - 950 mg.
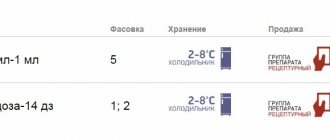
60 doses (10 g) - polyethylene bottles (1) complete with a dosing device - cardboard packs. 120 doses (18 g) - polyethylene bottles (1) complete with a dosing device - cardboard packs. 120 doses (18 g) - polyethylene bottles (2) complete with a dosing device - cardboard packs. 120 doses (18 g) - polyethylene bottles (3) complete with a dosing device - cardboard packs.
GCS for local use. It has anti-inflammatory and antiallergic effects when used in doses at which systemic effects do not occur.
Inhibits the release of inflammatory mediators. Increases the production of lipomodulin, which is an inhibitor of phospholipase A, which causes a decrease in the release of arachidonic acid and, accordingly, inhibition of the synthesis of arachidonic acid metabolic products - cyclic endoperoxides, prostaglandins. Prevents the marginal accumulation of neutrophils, which reduces inflammatory exudate and the production of lymphokines, inhibits the migration of macrophages, and leads to a decrease in the processes of infiltration and granulation. Reduces inflammation by reducing the formation of a chemotaxis substance (impact on late allergy reactions), inhibits the development of an immediate allergic reaction (due to inhibition of the production of arachidonic acid metabolites and a decrease in the release of inflammatory mediators from mast cells).
In studies with provocative tests with the application of antigens to the nasal mucosa, the high anti-inflammatory activity of mometasone was demonstrated, both in the early and late stages of the allergic reaction.
This was confirmed by a decrease (compared with placebo) in histamine concentrations and eosinophil activity, as well as a decrease (compared with baseline) in the number of eosinophils, neutrophils and epithelial cell adhesion proteins.
When administered intranasally, the systemic bioavailability of mometasone furoate is 1%), identified during clinical studies in patients with allergic rhinitis or nasal polyposis, and during post-registration use of the drug, regardless of the indication for use, are presented in Table 1. Adverse reactions are listed in accordance with classification of systemic organ classes MedDRA. Within each systemic organ class, adverse reactions are classified by frequency of occurrence.
Nosebleeds, as a rule, were moderate and stopped on their own, the frequency of their occurrence was slightly higher than when using placebo (5%), but equal or less than when prescribing other intranasal corticosteroids, which were used as an active control (in some of In them, the incidence of nosebleeds was up to 15%). The incidence of all other adverse events was comparable to that observed with placebo.
GCS for local use, the effect of which is manifested when applied in doses in which the drug does not cause systemic effects. With long-term treatment, it does not suppress the function of the hypothalamic-pituitary-adrenal system. Has anti-inflammatory and anti-allergic effects. The onset of a clinically significant effect is observed within the first 12 hours after the first use of the drug.
Allergic rhinitis (seasonal or year-round) in adults and children over 12 years of age. Chronic sinusitis (exacerbation, as part of complex therapy).
Hypersensitivity, infectious diseases of the nasal mucosa, recent surgery or trauma to the nose (until the wounds heal completely), children (up to 12 years). Caution. Tuberculosis (active or latent), fungal, bacterial, systemic viral infection, Herpes simplex with eye damage, long-term therapy with systemic corticosteroids, pregnancy, lactation.
Burning, itching, irritation, dryness and atrophy of the mucous membrane, nosebleeds, pharyngitis, candidiasis, bronchospasm, stretch marks, hypertrichosis, secondary infection. With long-term use, systemic side effects are possible. Newborns whose mothers used corticosteroids during pregnancy have adrenal insufficiency.
For adults and children over 12 years of age, the preventive and therapeutic dose is 2 inhalations of 50 mcg in each nasal passage, 1 time per day; daily dose - 200 mcg. If necessary, the dose can be increased to 4 inhalations in each nasal passage; daily dose - 400 mcg. After the symptoms of the disease disappear, a dose reduction is recommended. Maintenance dose - 50 mcg in each nasal passage; daily dose - 100 mcg. When treating sinusitis - 2 inhalations (100 mcg) into each nasal passage 2 times a day. Children from 3 to 12 years old - 1 inhalation (50 mcg) into each nasal passage per day. After the initial “calibration” period, during the first 6-7 presses of the spray button, a stereotypical supply of drugs is established, in which with each press of the button 50 mcg of mometasone suspension is released.
Do not use in ophthalmology. During treatment, it is necessary to examine the nasal mucosa: if a bacterial or fungal infection develops, treatment should be discontinued. Before using the inhaler, perform 6-7 calibration clicks. After a break in treatment for 2 weeks or more, re-calibration is carried out before use. Shake the bottle before use.
Nasonex as a treatment for adenoiditis in a 4-year-old child. Has anyone come across this?
My son is 4.5. Nasonex was prescribed for adenoids. How long can it be used? And is it safe?
Our pharmacies are stocked with antiallergic drugs. The showcases are full of beautiful packaging, and TV screens and the pages of glossy magazines obsessively talk about happy allergy sufferers who don’t care about flowers and herbs after being treated with pills. But not a single advertising medium says how often tablet drugs are powerless against allergies. And the unaware sufferers, who have tried all the advertised medicines and continue to sneeze and sniffle, may never know that the most effective remedy remains unknown. We're talking about Nasonex, the drug of choice for moderate to severe allergies.
>> The site presents an extensive selection of medications for the treatment of sinusitis and other nasal diseases. Enjoy it for your health!
Clinical studies have confirmed that within the first 12 hours after starting treatment with Nasonex, a pronounced effect is obtained by 28% of patients with allergic rhinitis (simply, allergic rhinitis). 36 hours after the start of therapy, allergy symptoms subsided in half of the patients.
Surprisingly, Nasonex nasal spray can also relieve ocular allergic symptoms: redness, itching and lacrimation.
Mometasone works great not only for allergies. Thus, in patients suffering from nasal polyps, treatment with Nasonex leads to noticeable clinical improvement. In particular, after a course of therapy, nasal congestion, traditional for nasal polyps, is greatly reduced, their size decreases, and even the sense of smell is restored.
Nasonex is also used in the complex therapy of rhinosinusitis, including sinusitis.
The anti-inflammatory effect of mometasone can significantly alleviate the course of the disease. Treatment with mometasone has been clinically proven to reduce facial pain and sinus pressure, rhinorrhea and nasal congestion. Moreover, the effect in acute and chronic sinusitis is long-lasting, lasting for at least 15 days after the end of treatment.
Yes, you say, it’s wonderful that Nasonex is so effective for diseases of the nasopharynx. But, however, it is not the safest drug - corticosteroid hormones. This is dangerous!
In fact, only the first sentence is true, the second is partly true, and the third is completely false. Indeed, Nasonex is a hormonal drug. And in fact, long-term use of oral corticosteroids is associated with a high risk of severe side effects. But intranasal drugs behave differently in the body.
It has been established that after intranasal spraying of mometasone, less than 1% of the active substance penetrates into the blood. Even if you were somehow miraculously able to swallow the medicine, it is practically not absorbed from the gastrointestinal tract due to very low absorption. Those trace amounts that are still absorbed are almost completely excreted in bile or urine.
Thus, the corticosteroid mometasone administered intranasally, that is, in the form of a nasal spray, does not act systemically. And, therefore, it cannot cause side effects. Therefore, Nasonex is one of the safest drugs for the common cold, despite the fact that it contains a real hormonal substance.
So, let's list the diseases for which mometasone spray is prescribed. Among them:
- seasonal or year-round allergic rhinitis. Let us add that Nasonex is used both for the treatment of allergies and for prevention before the allergy season;
- acute sinusitis (including acute sinusitis). Nasonex in such cases is only an integral part of complex treatment, often against the background of concomitant antibiotic therapy;
- nasal polyps with active symptoms (nasal congestion and loss of smell).
Nasonex is a dosed drug, so it is very important to correctly calibrate the bottle. Only after careful calibration, each press will release a strictly adjusted dose of mometasone furoate, amounting to 50 mcg per 100 mg of medicinal suspension. The calibration itself is quite simple.
Before the first use, you need to press the sprayer 10 times in succession. As a result of these simple steps, a standardized supply of mometasone furoate is established.
If you have not used Nasonex for two weeks or longer, a follow-up calibration is necessary. To do this, you need to press the sprayer twice - this is enough to resume the regular supply of the active substance.
- firstly, Nasonex spray is a suspension in which the active substance is not dissolved, but is unevenly suspended in a solvent. Therefore, the bottle must be shaken before each use;
- secondly, the nozzle on the bottle may become clogged - after all, we are dealing not with a solution, but with a suspension. If you notice that this has happened, you need to remove the plastic cap, and then the nozzle, which should be rinsed with warm water. After drying it thoroughly, you can put it in place and treat it with Nasonex.
It is strictly forbidden to clean a clogged nozzle with a needle (knitting needle, hairpin, etc.). This may cause the dispenser to break down and the dispenser to malfunction. As a result, the final dosage of Nasonex may not correspond to the 50 mcg we need.
Composition and release form
The drug Nasonex is available in one single dosage form - a spray for intranasal use. In pharmacies you can find it in special bottles with a spray dispenser measuring 10 g (for 60 doses) and 18 g (for 120 doses).
The main active ingredient of this drug is mometasone furoate , which belongs to the group of synthetic glucocorticosteroids. It is for this reason that an involuntary question arises: can this spray be used by children, because it contains a hormone? The fact is that when entering through the nasal passages, this medicine “works” only in the nasal area, and if it enters the bloodstream, it is in an extremely small amount, so there is no need to worry.
One dose (one spray, roughly speaking) of the drug contains 50 mcg of this active substance. As for the excipients, these include: dispersed cellulose, glycerol, purified water, sodium citrate dihydrate, citric acid, benzalkonium chloride, polysorbate 80.
Operating principle
The active substance of the drug Nazonek has antiallergic and anti-inflammatory properties . Thanks to him, this tool:
- inhibits the release of prostaglandins - the main mediators of inflammation;
- enhances the production of lipocortin, which, in turn, reduces the synthesis of arachidonic acid, also a kind of mediator of inflammation and allergic reactions;
- relieves tissue swelling, reducing the amount of inflammatory exudate;
- blocks infiltration processes (penetration of allergens into tissues);
- promotes regeneration of the epithelium of the nasal cavity, etc.
The therapeutic effect due to the use of Nasonex is observed already 12 hours after the start of use. A big plus is the fact that mometasone furoate is not at all addictive, even with long-term use.
special instructions
In cases of long-term use of Nasonex, periodic examination of the nasal mucosa by an otolaryngologist is required. It is recommended to stop treatment if the development of a local fungal infection of the pharynx and nose is detected (special therapy is required). Discontinuation of the drug is required if irritation of the mucous membrane of the pharynx and nose persists for a long period.
Signs of suppression of the function of the hypothalamic-pituitary-adrenal system were not observed during long-term therapy with Nasonex.
Particular attention should be paid to patients receiving the drug after long-term treatment with systemic GCS. This is due to the fact that withdrawal of GCS in such patients may lead to the development of adrenal insufficiency, the recovery of which may take several months. If symptoms of adrenal insufficiency appear, it is recommended to resume taking systemic corticosteroids and take other necessary measures.
In some patients, when switching from treatment with systemic corticosteroids to the use of Nasonex, withdrawal symptoms of systemic corticosteroids may occur (for example, depression, fatigue, muscle and/or joint pain), despite a decrease in the severity of symptoms associated with damage to the mucous membrane nose In such cases, patients should be specifically avoided in order to ensure continued drug therapy. Changing treatment can also help identify previously developed allergic diseases (eczema and allergic conjunctivitis), which were previously masked by the use of systemic corticosteroids.
It should be taken into account that in patients receiving GCS, immune reactivity is potentially reduced. In this regard, they should be warned about the increased risk of infection when contacting patients suffering from infectious diseases (including chickenpox and measles), as well as the need to consult a doctor if such contact occurs.
If signs of a severe bacterial infection appear (for example, swelling in the periorbital or orbital area, persistent and sharp toothache or pain on one side of the face, fever), you should immediately consult a doctor.
No atrophy of the nasal mucosa was observed after using the drug for 1 year. Conducted studies of biopsy samples of the nasal mucosa revealed that mometasone furoate tended to contribute to the normalization of the histological picture.
No growth retardation was observed in children receiving the drug for a year at a dosage of 0.1 mg per day in placebo-controlled clinical studies.
Indications
The nasal spray we are considering is indicated for:
- constant allergic rhinitis;
- seasonal allergic rhinitis;
- acute or chronic sinusitis during exacerbation;
- rhinosinusitis;
- prevention of seasonal rhinitis caused by the flowering of certain plants;
- polyposis in the nose.
Contraindications and side effects
The drug we are considering is contraindicated for:
- individual intolerance to any of its components;
- recent trauma or surgery in the nasal area;
- tuberculosis respiratory tract infection;
- the presence of fungal, viral or bacterial infections of the nasal cavity;
- under 2 years of age.
In children, Nasonex can also in rare cases cause the following side effects:
- headache;
- burning in the nose;
- nosebleeds;
- frequent sneezing;
- ulcerations in the nose;
- pharyngitis;
- impaired sense of smell;
- bronchospasm;
- allergic reactions.
Nasonex spray naz.doz.50mkg/dose 120doses 103962
Description
Nasonex® Latin name Active substance ATC: Pharmacological group Nosological classification (ICD-10) Description of the dosage form Pharmacological action Pharmacodynamics Pharmacokinetics Indications of the drug Nasonex® Contraindications Use during pregnancy and breastfeeding Side effects Interaction Overdose Precautionary measures Storage conditions of the drug Nasonex® Shelf life of the drug Nasonex® Schering-Plough ( USA) spray for nasal use, dosed 50 mcg/dose; polyethylene bottle (bottle) with a dosing valve 18 g with a safety cap, cardboard pack 1; EAN code: 4602210000588; No. P N014744/01, 2009-03-17 from Schering-Plough Labo NV (Belgium) Nasonex® Mometasone * (Mometasonum) R01AD Corticosteroids Glucocorticoid for topical use [Glucocorticosteroids] J30 Vasomotor and allergic rhinitis J31 Chronic rhinitis, nasopharyngitis and pharyngitis J32 X White's chronic sinusitis or almost white suspension in a spray bottle. Pharmacological action - antiallergic, anti-inflammatory. Mometasone furoate is a synthetic glucocorticosteroid for topical use. It has anti-inflammatory and antiallergic effects when used in doses at which systemic effects do not occur. Inhibits the release of inflammatory mediators, increases the production of lipomodulin, which is an inhibitor of phospholipase A, which causes a decrease in the release of arachidonic acid and, accordingly, inhibition of the synthesis of arachidonic acid metabolic products - cyclic endoperoxides, PGs. Prevents the marginal accumulation of neutrophils, reduces inflammatory exudate and the production of lymphokines, inhibits the migration of macrophages, and leads to a reduction in the processes of infiltration and granulation. Reduces inflammation by reducing the formation of a chemotaxis substance (impact on “late” allergy reactions), inhibits the development of an “immediate” allergic reaction (due to inhibition of the production of arachidonic acid metabolites and a decrease in the release of inflammatory mediators from mast cells). In studies with provocative tests when applying antigens to the nasal mucosa, the high anti-inflammatory activity of Nasonex was demonstrated both in the early and late stages of the allergic reaction, which was confirmed by a decrease (compared to placebo) in the level of histamine and eosinophil activity, as well as a decrease in ( compared with baseline) numbers of eosinophils, neutrophils and epithelial cell adhesion proteins. Mometasone furoate has negligible bioavailability (≤0.1%) and when administered by intranasal inhalation, it is practically undetectable in blood plasma (even when using a sensitive detection method with a sensitivity threshold of 50 pg/ml). Therefore, there are no relevant pharmacokinetic data for this dosage form. The suspension is very poorly absorbed from the gastrointestinal tract, so the small amount that can enter the gastrointestinal tract after inhalation into the nasal cavity undergoes active primary metabolism even before excretion with urine or bile. treatment of allergic rhinitis (seasonal and year-round) in adults, adolescents and children over 2 years of age; exacerbation of sinusitis (complex therapy with antibiotics) in adults (including the elderly) and children over 12 years of age; prevention of moderate and severe seasonal allergic rhinitis (recommended 2–4 weeks before the expected start of the dusting season). hypersensitivity to any component of the drug; the presence of an untreated local infection involving the nasal mucosa; recent surgery or trauma to the nose (before the wound heals); tuberculosis infection (active or latent) of the respiratory tract, untreated fungal, bacterial, viral systemic infection or infection caused by Herpes simplex with eye damage (as an exception, the drug can be prescribed in these cases as directed by a doctor with great caution); children under 2 years of age (no data on safety of use). After intranasal use of the drug at the maximum therapeutic dose, mometasone is not detected in the blood plasma even at the minimum concentration; therefore, fetal effects can be expected to be negligible and potential reproductive toxicity very low. However, due to the fact that special, well-controlled studies of the drug's effect in pregnant women have not been conducted, Nasonex should be prescribed to pregnant women, breastfeeding mothers, or women of childbearing age only if the expected benefit from its use justifies the potential risk to the fetus and newborn. Newborns whose mothers used corticosteroids during pregnancy should be carefully examined to identify possible adrenal hypofunction. For the treatment of seasonal or year-round allergic rhinitis. In adults: - nosebleeds (obvious or discharge of blood-stained mucus or blood clots) - pharyngitis, - burning sensation in the nose, - irritation of the nasal mucosa. Nosebleeds, as a rule, stopped on their own and were not severe; they occurred at a rate slightly higher than with placebo (5%), but equal to or less than with other intranasal corticosteroids used as active controls (in some of them the incidence of nosebleeds was up to 15% ). The incidence of all other adverse events was comparable to that observed with placebo. In children: - nosebleeds, - headache, - irritation in the nose, - sneezing. The incidence of these adverse events in children was comparable to the incidence when using placebo. In the treatment of exacerbations of sinusitis (when using Nasonex spray as an adjuvant). In adults and adolescents: - headache, - pharyngitis, - burning sensation in the nose, - irritation of the nasal mucosa. Nosebleeds were moderate, and their incidence with Nasonex was also comparable to the incidence of nosebleeds with placebo (5% versus 4%, respectively). Very rarely, with intranasal use of GCS, cases of perforation of the nasal septum or increased intraocular pressure have been reported. Combination therapy with loratadine was well tolerated by patients. Interaction studies with other drugs have not been conducted. Symptoms: with long-term use of GCS in high doses, as well as with the simultaneous use of several GCS, inhibition of the function of the hypothalamic-pituitary-adrenal system is possible. Treatment: due to the low (less than 0.1%) systemic bioavailability, it is unlikely that in case of accidental or intentional overdose, any measures will be required other than monitoring the patient and then continuing treatment at the recommended dose. As with any long-term treatment, patients using Nasonex® nasal spray for several months or longer should be periodically examined for possible changes in the nasal mucosa. If a local fungal infection of the nose or pharynx develops, it is necessary to either discontinue the drug or carry out special treatment. Irritation of the nasal or pharyngeal mucosa that persists for a long time may also be an indication for discontinuation of the drug. In placebo-controlled clinical trials in children, when Nasonex® nasal spray was used at a daily dose of 100 mcg for a year, no growth retardation was observed in children. With long-term treatment with Nasonex® nasal spray, no signs of suppression of the function of the hypothalamic-pituitary-adrenal system were observed. Patients who switch to treatment with Nasonex® nasal spray after long-term therapy with systemic GCS require special attention. Discontinuation of systemic GCS in such patients may lead to adrenal insufficiency, which may require appropriate measures. During the transition from treatment with systemic GCS to treatment with Nasonex® nasal spray, some patients may experience symptoms of GCS withdrawal, for example, joint and/or muscle pain, fatigue, depression; despite a decrease in the severity of symptoms associated with damage to the nasal mucosa; such patients must be specifically convinced of the advisability of continuing treatment with Nasonex® nasal spray. A change in therapy may also reveal previously developed allergic diseases, such as allergic conjunctivitis, eczema, which were previously masked by systemic GCS therapy. Patients receiving treatment with GCS have a potentially reduced immune reactivity; they must be warned about the increased risk of infection in case of contact with patients with infectious diseases (varicella, measles), as well as the need for medical consultation if such contact occurs. At a temperature of 2–25 °C. (do not freeze) Keep out of reach of children. 3 years. Do not use after the expiration date stated on the package. 2000-2015. Register of Medicines of Russia The database is intended for healthcare professionals. Commercial use of materials is not permitted.
Compound
Composition and release form Dosed nasal spray 1 dosamomethasone furoate (in the form of monohydrate) 50 mcg excipients: dispersed cellulose BP 65 cps; glycerol; sodium citrate dihydrate; citric acid monohydrate; polysorbate 80; benzalkonium chloride; phenylethyl alcohol; purified water in a plastic bottle with a dosing valve for 120 doses; 1 bottle in a cardboard box.
Application
Method of administration and dosage: Intranasal. Nasonex® is used in the form of intranasal inhalation of a suspension contained in a spray bottle. Inhalations are carried out using a special dispensing nozzle on the bottle. Before using Nasonex® nasal spray for the first time, it is necessary to “calibrate” it by pressing the dispensing device 6-7 times. After “calibration”, a stereotypical delivery of the drug is established, in which with each press of the button approximately 100 mg of mometasone furoate suspension is released, containing mometasone furoate monohydrate in an amount equivalent to 50 μg of chemically pure mometasone furoate. If the nasal spray has not been used for 14 days or longer, recalibration is necessary before using it again. Before each use, shake the spray bottle vigorously. Treatment of seasonal or year-round allergic rhinitis For adults (including the elderly) and adolescents over 12 years of age, the usually recommended preventive and therapeutic dose of the drug is 2 inhalations (50 mcg each) into each nostril, once (total daily dose 200 mcg). After achieving the desired therapeutic effect for maintenance therapy, it is advisable to reduce the dose to 1 inhalation in each nostril 1 time per day (total daily dose 100 mcg). If a reduction in the symptoms of the disease cannot be achieved by using the drug at the recommended therapeutic dose, the daily dose can be increased to 4 inhalations into each nostril once a day (total daily dose 400 mcg). After the symptoms of the disease decrease, a dose reduction is recommended. The onset of action of the drug is usually noted clinically within the first 12 hours after the first use of the drug. Children 2–11 years of age: the recommended therapeutic dose is 1 inhalation (50 mcg) into each nostril once a day (total daily dose is 100 mcg). Auxiliary treatment of exacerbations of sinusitis Adults (including the elderly) and adolescents over 12 years of age: the recommended therapeutic dose is 2 inhalations (50 mcg) into each nostril 2 times a day (total daily dose 400 mcg). If a reduction in the symptoms of the disease cannot be achieved by using the drug at the recommended therapeutic dose, the daily dose can be increased to 4 inhalations into each nostril 2 times a day (total daily dose - 800 mcg). After the symptoms of the disease decrease, a dose reduction is recommended. After 12 months of treatment with Nasonex® nasal spray, there were no signs of atrophy of the nasal mucosa; In addition, mometasone furoate tended to contribute to the normalization of the histological picture when examining biopsy specimens of the nasal mucosa.
Possible product names
- Nasonex naz spray 50mcg/dose 120doses N1
- NASONEX 50 MCG/DOSE NASAL. SPRAY 120 DOSES
- NASONEX SPRAY 50 MCG/DOSE 120 DOSES (18G) FL.DOSE. DEVICE+COL. X1
- NASONEX REF. NAZ. DOSER. 50 mcg/dose FL. 18G (120DOZ) No. 1
- NASONEX 50MCG/DOSE NASAL SPRAY DOSER. 120DOZ (18G) FL. X1 (R)
- (Nasonex) Nasonex nas spray 50 mcg/dose 120 doses N1
Directions for use and dosage
Before you start using the drug, you must make sure that its dispensing nozzle is ready. To do this, it should fit comfortably on the bottle and, when pressed, dispense a dose of the drug equal to approximately 100 mg (for this, the first time you use it, you need to press it about 6 times for full “calibration”).
For direct use, the end of such a nozzle must be inserted into the nasal passage and pressed on the dispensing device to spray (1 press = 1 spray). The head and bottle with the drug must be kept strictly vertical.
The daily therapeutic dose of this drug is:
- for children from 2 to 11 years old - 1 injection into each nasal passage 1 time per day;
- for children over 12 years of age and adults – 2 injections into each nasal passage 2 times a day (the dose can be increased to 4 injections into each nasal passage 2 times a day);
- for children over 12 years of age and adults for prevention purposes - 2 injections into each nasal passage 1 time per day.
To prevent the dispensing nozzle from malfunctioning, it must be washed regularly under the tap.
Reviews from parents about spray treatment
Nasonex did not suit my daughter; on the contrary, the swelling began even worse. ENT called the representatives of this medicine, they said - remove it. Sometimes it happens. Now we take Flixonase and there is an improvement.
Olesya
https://vladmama.ru/forum/viewtopic.php?f=1103&t=75754&start=80
It really helps us, but we have grade 1 adenoids - they have hardly shrunk, but the runny nose went away already on the 2nd day. His daughter is 2 months old. prescribed 1 spray per day.
Anna
https://www.u-mama.ru/forum/kids/child-health/548439/index.html
After the acute phase, one ENT specialist prescribed 1 injection of Nasonex for 2 weeks. The other one is for a month, and it is better to spray it twice, morning and evening. Now we seem to be holding on, going to kindergarten, but I’m afraid that we’ll cancel it, whether everything will start all over again. The adenoids have grown to grade 2-3. Snoring doesn't bother me. I would like to take my child to the pool again, but I’m also afraid.
Natalia
https://www.u-mama.ru/forum/kids/child-health/548439/index.html
A year ago, my daughter was diagnosed with stage 2 adenoids. They prescribed Nasonex and had been sick very often before it. After the course (10 days) everything was fine, my nose didn’t bother me even with a cold, there were no complications to my nose. Six months later, the adenoids reminded themselves, and again 10 days of Nasonex. We took it to the south in the summer, everything was fine. Homeopathy was used for prevention. Now my nose is stuffy again and it’s running down the back wall. The doctor started talking about Nasonex again...
Zhanna https://deti.mail.ru/forum/zdorove/detskoe_zdorove/nazoneks_pri_adenoidah_by_zhannet_0579_mail_ru/
Overdose
An overdose of this drug is possible with long-term use in large doses or with simultaneous use with other glucocorticosteroids, and can negatively affect the functioning of the adrenal glands. In such cases, it is necessary to seek qualified medical help.
Interaction with other drugs
Nasonex is a drug that can be used in combination therapy with other medications.
For the treatment of moderate allergic sinus diseases, it is prescribed in combination with antihistamines, for example, loratadine. As the instructions say, this combination is safe and does not cause any side effects in the patient.
To date, there is no information regarding the interaction of Nasonex with other drugs.
Analogs
The following drugs can be analogues of Nasonex for children:
- Flix (approved for use from 2 years);
- Allertek Naso (approved for use from 2 years);
- Glenspray (approved for use from 2 years);
- Metaspray (approved for use from 2 years);
- Rizonel (approved for use from 2 years);
- Avamis (approved for use from 6 years of age);
- Nasobek (approved for use from 6 years).
Which is better for a child: Nasonex or Avamis
Very often, consumers compare these two medications. And it is not surprising, because they have a similar therapeutic effect, method of application and indications. However, these funds also have a number of significant differences:
- Compound . Thus, the active substance of the drug Nasonex is mometasone furoate, and the drug Avamis is a substance called fluticasone furoate. If we compare these two components, we can safely say that mometasone furoate has a more gentle effect on body tissue.
- Contraindications . Thus, Avamis has fewer contraindications than Nasonex spray, but it can only be used from 6 years of age, while Nasonex can be used from 2 years of age.
- Price . Nasonex is a more expensive drug than Avamys (about twice as expensive).
But do not forget that, despite the similarity of these two drugs, they are still not interchangeable, and what to prescribe - Nasonex or Avamis - is decided solely by the doctor in each specific situation.
What can replace Nasonex?
Nasonex is not the only steroid drug that can be used in the treatment of inflamed adenoids. There are other hormonal analogue drugs. They differ not only in the active substance, but also in price. Despite the similar action, their age restrictions are different. However, this is explained by the fact that the company producing the product has not conducted studies on the effects of the product on children of a certain age.
Medicinal analogues of the drug
| Drug name | Active substance | Age restrictions | Price |
| Avekort | Mometasone | For allergic rhinitis, it is allowed from the age of two; for exacerbation of sinusitis and for the prevention of seasonal allergic rhinitis, it is used from the age of 12 | From 174 rubles depending on the release form |
| Asmanex twisthaler | Mometasone | From 12 years old | From 795 rubles depending on the volume of the drug |
| Aldecin | Beclomethasone | From 6 years old | From 128 rubles |
| Beclazone Eco easy breathe | Beclomethasone | From 4 years old | From 642 rubles depending on the volume of the drug |
| Rhinoclenil | Beclomethasone | From 12 years old | From 400 rubles |
| Azmacort | Triamcinolone | From 6 years old | On request |
Drugs that can replace Nasonex, pictured
Azmacort is a steroid drug based on triamcinolone
Rinoclenil is a hormonal drug based on beclomethasone.
Beclazon Eco easy breathing is allowed for children from four years of age
Aldecin is a steroid drug based on beclomethasone
Asmanex twisthaler is an analogue of Nasonex in terms of the active substance, approved for children from 12 years of age
Avecort is a complete analogue of Nasonex
Homeopathy and physiotherapy
Therapy with homeopathic remedies and physiotherapy are alternative options for treating adenoids.
The most popular drugs in homeopathy to solve this problem are:
- diluted thuja oil;
- Job the Kid;
- Phthision;
- Lymphomyosot;
- Euphorbium compositum;
- Calcarea carbonica 6.
They are prescribed by doctors either as independent remedies or as components of complex therapy. Their main disadvantage is that they are designed for long-term use (from six months or more), and traditional medicine completely denies any proven effectiveness of drugs.
Physiotherapy is rarely prescribed in the treatment of adenoids without concomitant medication, but has proven itself to be a fairly effective way to combat adenoiditis.
Types of procedures:
- electrotherapy: electrophoresis, magnetic therapy, EHF therapy (extreme high frequency therapy). After exposure, swelling of lymphoid tissue decreases;
- inhalation. Made with the addition of mineral water, diphenhydramine, calcium chloride. Hot inhalations for adenoiditis are contraindicated, as they contribute to even greater tissue swelling;
- nebulizer treatment. Used as a replacement for conventional inhalations. The principle of operation is fine cold spraying of medicinal substances onto growing tissues;
- cryotherapy. The adenoids are exposed to liquid nitrogen, which stops the growth of tissue.
Reviews
Ekaterina: “My child has had a seasonal allergy to flowers almost since birth. At the same time, a river flows from the nose! Previously, we struggled somehow, using regular nasal drops, but everything went away completely only at the end of the season. This year, one competent doctor prescribed Nasonex spray for us during such allergic rhinitis. I had a lot of doubts about him, because he is hormonal. However, the doctor assured me that there was nothing to worry about, since this remedy acts locally in the nose and does not enter the bloodstream. I want to tell you that the result was obvious already on the second day of use. The amount of snot decreased noticeably, and the child began to breathe without problems. So we survived this allergic season without any problems thanks to Nasonex. The product is not cheap, but it works as expected.”
Maria: “Nasonex was prescribed to me, an adult woman, by an otolaryngologist, supposedly to boost local immunity after an illness. I used it for two days as directed, and on the third day I developed a severe allergy: the mucous membranes were swollen, my nose was burning, my snot was flowing non-stop! I read several forums about this product and found that I was not the only one who experienced such side effects after using this spray.”
Anna: “After a long illness, my son developed adenoiditis, and the ENT doctor prescribed us this spray to treat it. Initially, I was against Nasonex, because hormonal drugs are often scary, however, when I opened the Internet, I found many positive reviews there that it was effective in treating adenoids for children. And in fact, this tool helped us. Within a week or two, my son began to breathe fully through his nose, and we forgot about these problems.”
Yana: “My daughter has hay fever, and at the end of summer - at the beginning of September, when ragweed blooms, her life turns into flour: her eyes water, her nose is stuffy, snot flows in streams. Under such circumstances, Nasonex helps us a lot. Within a couple of days after using it, it becomes much easier. It’s just a pity that it’s expensive, but it definitely helps.”
Valeria: “Nasonex was prescribed to my daughter by an ENT specialist for stage 2 adenoids. We used it for a whole month, but the result was “0”. He didn’t justify himself.”
Expert opinions on the treatment of adenoids with hormonal drugs
Treatment with steroid drugs is considered dangerous by many, as there are still many myths regarding their side effects. Therefore, the opinion of specialists about this kind of medicine is interesting.
Otolaryngologist Ivan Vasilyevich Leskov describes in detail the principle of action of the drug and talks about the side effects:
Nasonex suppresses lymphoid tissue, which actually leads to a reduction in adenoids. It usually has to be used for a long time - in case of severe inflammation, Nasonex is not very effective. As a hormonal drug, it additionally suppresses local immunity, so when it is discontinued, inflammation in the adenoids resumes.
Moreover, he urges careful use of Nasonex:
Nasonex is not contraindicated in children under 18 years of age - this drug is absolutely not absorbed into the blood, however, its use for the treatment of adenoids, and especially sinusitis, does not stand up to criticism - if sinusitis and enlarged adenoids are of an inflammatory nature, Nasonex is simply ineffective.
But otolaryngologist Evgenia Vladimirovna Filatova has the opposite point of view and advises using a steroid medication:
Nasonex is a hormonal drug, but the hormone in a special form for local use does not have a general effect on the body (since it is almost not absorbed from the nasal mucosa). Don't be afraid to use it.
Doctor of the highest category, Evgeny Olegovich Komarovsky, that the use of any drugs for adenoiditis is useless:
Everyone thinks that there are some magic pills, some drops that can be given to a child, and he will not have adenoids, or they will go away. <…> In fact, if adenoiditis is of allergic origin, then, naturally, the active use of antiallergic drugs can reduce allergic swelling of the adenoid tissue. But if a child often suffers from viral infections, then there are no pills that can affect the adenoids.