On TV you can often see advertisements about all kinds of remedies against such a terrible disease as dysbiosis. However, such a diagnosis does not exist in the international classification of diseases. But who among us has not experienced bloating, flatulence or discomfort after eating? How did it happen that there are symptoms, but no disease?
Let's take a closer look at what intestinal dysbiosis is, the symptoms and causes of this pathological condition, and whether it needs to be treated or whether it goes away on its own.
What is intestinal microflora and why is it needed?
The largest number of microorganisms is found in the intestines. These are various lacto- and bifidobacteria, E. coli, yeast and enterococci. Some of them are beneficial to the body, and some are conditionally pathogenic, that is, capable of leading to disease under certain circumstances.
But as long as the balance between them is maintained, the human body receives a number of useful functions from its carriers. This is strengthening the immune system, destroying toxins and carcinogens, providing cells with additional energy, and producing certain vitamins.
Lacto- and bifidobacteria are beneficial microorganisms. Their goal is to fight pathogenic microbes and curb the growth of their numbers.
But sometimes an imbalance occurs in the intestines, which is associated with a decrease in the number of “good” bacteria and, accordingly, an increase in pathogenic microflora. This condition is usually called dysbiosis. It occurs as a result of other pathological changes in the body. Thus, dysbiosis is a set of symptoms that signal that problems have arisen in the body.
Historical reference
At the beginning of the 20th century, the Russian scientist Mechnikov studied bacteria inhabiting the intestines. He was the first to use bifidobacteria to treat digestive disorders in children.
The term “dysbacteriosis” was proposed in 1916 by the German scientist Nisle. In 1956, the first drug for restoring microflora in adults, Eugalan, was developed in Germany.
And 8 years later, the drug for children Lactana-B-milk was released. This was especially true for bottle-fed children. Later, bacteria began to be added directly to baby food.
Dysbacteriosis (dysbiosis) is not included in the official list of diseases.
Prevalence
Almost every person experiences dysbacteriosis. Up to 90% of the adult population and over 95% of children suffer from a violation of the intestinal flora . This condition does not leave immunity and may recur.
This prevalence of the problem is associated with deteriorating living and nutritional conditions and an increase in stress. And also because pathogenic bacteria are more tenacious. When exposed to harmful factors, beneficial microorganisms die faster than harmful ones.
Dysbacteriosis is often underestimated. Namely, it is from this problem that many diseases begin and the body as a whole is weakened.
How dangerous are pathogenic microflora?
Balance in the gut is a stimulant of the immune system. With dysbacteriosis, the immune system is suppressed, which leads to frequent colds, as well as exacerbation of chronic pathologies.
Long-term dominance of pathogenic microorganisms in the intestine can lead to inflammatory processes of the mucous membrane. This increases the risk of developing various pathological neoplasms.
Microbial imbalance can also lead to incomplete absorption of nutrients from food. Lack of microelements and vitamins leads to anemia, vitamin deficiency and other deficiency conditions.
Often, intestinal problems provoke skin diseases. For example, acne in adulthood is a frequent companion to dysbiosis.
Therefore, despite the fact that this syndrome is not a disease, seeing a doctor and treatment is still necessary.
Prevention
Fermented milk products are a source of beneficial bacteria, and fiber-rich foods create a nutritious environment for them. By eating the right foods, you can prevent the development of dysbiosis. Fresh vegetables and fruits suppress pathogens and create favorable conditions for normal intestinal function.
You cannot self-medicate and choose your own medications. Your doctor will warn you if the medicine affects your intestinal flora.
After taking potent medications, in severe stressful situations, or after suffering from viral diseases, you should take preventive courses of probiotics.
For infants, the best prevention is breastfeeding for at least one year. No formula can replace the unique composition of mother's milk. Also, do not rush into complementary feeding. All products should be introduced in a timely and gradual manner. If you have a negative reaction to any food, it is better to wait a while before introducing it.
Main causes of dysbiosis
A variety of factors can lead to a pathological condition of the intestines. But the main reason is taking antibiotics. Antibacterial drugs, even with the correct dose selection, have a negative effect on positive microorganisms. Therefore, together with such medications, you should always take drugs that are aimed at protecting the intestinal microflora.
Other reasons doctors include:
- gastrointestinal diseases (irritable bowel syndrome, colitis, intestinal infections);
- parasitic infection;
- immunodeficiency states (after chemotherapy, HIV);
- malformations of the digestive system.
The intestinal microflora is very sensitive, and a variety of reasons can lead to imbalance. It can also be climate change, poor nutrition, strict diets, frequent stress, eating on the go.
Kinds
Depending on the cause of its occurrence, intestinal dysbiosis syndrome in modern medicine is divided into several types.
- Dysbacteriosis that occurs in healthy people:
- Professional (violations occur due to harmful professional activities)
- Age-related (flora is disrupted due to aging of the body)
- Nutritional (associated with poor nutrition)
- Seasonal (flora changes depending on the time of year, mainly in cold weather).
By severity:
- light;
- medium-heavy;
- heavy.
With the flow:
- acute (up to 30 days);
- prolonged (up to 4 months): with clinical manifestations (continuous or recurrent) and without clinical manifestations;
- chronic (more than 4 months): with clinical manifestations (continuous or recurrent) and without clinical manifestations.
Dysbacteriosis of the small intestine
Dysbacteriosis of the small intestine begins to manifest itself when it is over-contaminated. In this case, the microbial composition changes, which provokes disruption of the normal functioning of the gastrointestinal tract. The pain is localized in the navel area.
Dysbacteriosis of the large intestine
Colon dysbiosis is an extremely common pathology that disrupts the microflora simultaneously in the stomach, duodenum, and intestines. The disease can be long-lasting, take a more severe form and disrupt a person’s normal lifestyle.
How does pathology manifest itself?
Signs of dysbiosis depend on the individual characteristics of the organism. They can be divided into local and general.
Local
- flatulence;
- abdominal discomfort;
- pale skin;
- constipation;
- swelling;
- bloating.
Are common
- intoxication;
- anemia;
- dehydration;
- weight loss;
- metabolic disease.
If dysbiosis occurs, symptoms in adults may manifest themselves in decreased performance, deterioration in general well-being, as well as food allergies to certain foods.
Symptoms
Intestinal dysbiosis develops slowly and occurs for a long time without pronounced symptoms. In the latent phase, only minor clinical signs may appear when a healthy diet is disrupted. Diagnosis always takes into account the severity of symptoms and their specificity.
At different stages of development of microflora imbalance, the following set of symptoms is observed:
- nausea;
- diarrhea;
- change in stool color and odor;
- impurities of mucus and blood in the stool;
- pain and cramps in the abdomen;
- flatulence;
- pale skin;
- dehydration of varying degrees of severity.
Severe dysbiosis is often accompanied by a disorder in the immune system, frequent allergic skin reactions, and anemia. In severe cases, a pronounced intoxication syndrome develops with the addition of pathogenic microflora.
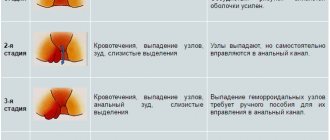
Forms and stages of dysbiosis
This painful condition develops in stages, so symptoms in the initial stages are either absent or insignificant.
- Stage I
Characterized by a slight decrease in the number of Escherichia coli (Escherichia coli). They fight putrefactive microorganisms and also participate in water-salt and lipid metabolism. The number of bifidobacteria and lactobacilli remains normal.
- Stage II
The number of E. coli decreases. As a result, the growth of pathogenic flora begins. There is a deficiency of lacto- and bifidobacteria.
- Stage III
The number of beneficial bacteria is significantly reduced. An imbalance arises. Pathogenic microorganisms begin to have a negative impact on the functioning of the gastrointestinal tract.
- IV stage
Lactobacilli and/or bifidobacteria are completely absent. Pathogenic microflora leads to destructive processes in the intestines.
Dysbacteriosis can develop in both the small and large intestines. This pathological condition can occur not only in the intestines. There is also vaginal dysbiosis, which occurs in a woman’s vagina. It can be caused by hormonal changes, abuse of local antiseptics, taking antibiotics and immunomodulators.
Answers to popular questions
- Can dysbiosis go away on its own? In some cases, it is indeed possible to independently rid the body of a minor disturbance in the intestinal microflora. For example, when the cause of the disorder is an emotional shock experienced, or the process of acclimatization. If the disease has not progressed beyond the first degree, then dysbiosis may go away on its own. However, in this case, a person is unlikely to notice at all that he has had a disturbance in his intestinal microbiocenosis. If more severe symptoms develop, you should not hope for self-healing; you must seek help from a specialist.
- Is dysbiosis contagious? Dysbacteriosis itself is not a contagious disease, because it occurs against the background of any conditions in the human body. However, some of the reasons that provoke it can pose a danger to others. For example, if dysbacteriosis develops against the background of helminthiasis.
- Can there be a temperature with dysbacteriosis? An increase in body temperature with dysbacteriosis is possible. It can be caused both by the cause of the development of dysbiosis, and by the dysbiosis itself, as a result of which symptoms of intoxication are often observed.
Doctor's appointment and diagnostics
If you experience unpleasant intestinal symptoms, as well as general poor health, you should consult a gastroenterologist. If a microflora disturbance occurs as a result of an infectious disease, then consultation with an infectious disease specialist is recommended.
A preliminary examination and laboratory diagnostics will allow us to determine the true cause that led to the pathological change in the microflora.
Important! Dysbiosis has common symptoms with other gastrointestinal disorders, so it is difficult to make a correct diagnosis based on symptoms alone.
To do this you need to undergo the following studies:
- Ultrasound of the abdominal organs.
- Pass a coprogram and biochemical analysis of stool.
- General blood and urine tests.
- GC/MS (gas chromatography) - determination of the amount of hydrogen in exhaled air.
If you suspect vaginosis, you should consult a gynecologist. In addition to the examination, the doctor will prescribe a vaginal culture.
What examination is needed
Symptoms of dysbacteriosis are nonspecific. The same symptoms may mask pathology of the digestive system or hypovitaminosis. Therefore, dysbiosis is considered a clinical and laboratory syndrome.
Diagnosis begins with a scatological examination, which allows you to assess digestive function, the state of enzyme systems, peristalsis and the speed of movement of the food bolus.
But a change in the composition of feces does not indicate dysbacteriosis. It is necessary to confirm changes in the composition of bacteria in the intestinal lumen. In Moscow, many clinics use gas-liquid and ion chromatography methods. They make it possible to determine the composition of the microflora based on the resulting metabolites.
Bacteriological testing is often used. To do this, swabs from the intestinal mucosa, feces or scrapings are sown on special nutrient media. This method allows you to obtain colonies of bacteria and determine their type with high accuracy. A special stool test for dysbacteriosis is also used. But a mandatory condition is that the biological material must reach the laboratory no later than an hour after it is received from the patient. Feces must be kept warm so as not to cause the death of bacteria. The method does not justify itself by providing an idea only of the state of the colon flora.
The gold standard for diagnosing dysbacteriosis is intestinoscopy. This is an endoscopic method during which a flexible probe with a video camera is inserted into the cavity of the small intestine through the mouth and stomach or rectum and colon. It is necessary to examine the intestinal mucosa and obtain an aspirate of its contents. The resulting liquid is also inoculated onto a nutrient medium. The disadvantage of this method is the need for general anesthesia, special bacteriological media and a long wait for the result. Sometimes a breath test with labeled H2 is used to diagnose dysbiosis.
How to treat intestinal dysbiosis
Therapy is selected individually, based on test results. The general scheme includes:
- Reducing the excess number of pathogenic microorganisms.
- Restoration of beneficial microflora.
- Improved bowel function.
All drugs must be prescribed taking into account the tests, otherwise the treatment will be ineffective.
If a large number of opportunistic bacteria have been detected, treatment is carried out using bacteriophages and intestinal antiseptics. These drugs quickly and gently deal with excess bacterial growth, thereby freeing up space for the “population” of positive microorganisms. Taking such medications lasts at least a week. Only after this is a course of drugs with the necessary lacto- or bifidobacteria, which are in short supply. Probiotics (eubiotics) are used for this purpose. They must be taken for at least 3 weeks.
Therapy may also include taking prebiotics. These funds are aimed at enhancing the growth of one’s own beneficial microflora. They improve digestion processes, strengthen the immune system, and help reduce the formation of gases in the intestines.
The use of eubiotics is also effective.
When helminths are detected, antiparasitic therapy is carried out.
Antibacterial agents
Antibiotics for the treatment of dysbiosis should be selected by a doctor and only in exceptional cases. For example, their use is justified in case of rapid growth of pathogenic flora, as well as if serious disturbances in the processes of absorption and digestion of food are identified.
In other cases, taking antibacterial drugs will worsen the microflora.
Immunomodulators
During a microbial imbalance, the immune system is suppressed, so at the final stage of treatment, the doctor may recommend taking such drugs to increase local immunity.
Their independent prescription and use is prohibited. Correct use of immunomodulators has a beneficial effect on the outcome of treatment. Helps reduce the risk of relapse of pathology.
Antibacterial drugs, intestinal antiseptics, bacteriophages
Their use should be very careful, prescribed only by a gastroenterologist, when the degree and form of dysbiosis is known, based on the laboratory-determined sensitivity of the bacterium to a specific drug:
Antibacterial drugs
- Staphylococcus - for example, if dysbiosis is caused by the proliferation of staphylococcus, then staphylococcal or pyobacteriophage is indicated, treatment for 14 days. If we are dealing with a combined lesion (inflammation of the navel in a newborn, risks of sepsis in premature infants), then macrolides (azithromycin, clarithromycin, josamycin) or aminoglycosides.
- Enterococci - if enterococci predominate (the most common of which is Klebsiella), then Klebsiella bacteriophage or nitrofurans (Ersefuril, Furazolidone, Stop-diar, Enterofuril), macrolides, levomycetin or semi-synthetic penicillins are indicated.
- Protea - modified E. coli or Protea are most often sensitive to nitrofurans - the most effective are nitrofurans (Ersefuril, Enterofuril), nalidixic acid derivatives - Nevigramon, as well as Sulgin, Fthalazol - sulfonamide drugs.
- Pseudomonas aeruginosa - to suppress its reproduction, polymyxin, carbenicillin or aminoglycosides - Kanamycin, Gentamicin - are most often used.
- Candidiasis - dysbacteriosis caused by the growth of fungi of the genus Candida or other fungal agents is treated with antifungal drugs, such as Fluconazole (Diflucan, Mikosist, Flucosan, Fluconorm, etc.), Terbinafine (Lamisil, Terbizil, Terbinox, Exittern, Bramisil), amphotericin B (Ambisome, Amphocil, Amphoglucamine, Ampholip, Fungizone).
- Clostridia - when it comes to pseudomembranous colitis caused by clostridia, a course of metronidazole (Trichopol) is first prescribed, and if it is ineffective, a course of the antibiotic vancomycin is prescribed.
Bacteriophages
Bacteriophages are special viruses that act on a specific type of bacteria; they can be used as an independent treatment or in combination with other antimicrobial therapy, used in the form of enemas or for oral administration. Currently, the following bacteriophages are produced: Proteus, staphylococcal, coliproteus and Pseudomonas (more about treatment with bacteriophages).
Restoring microflora with nutrition
An important step in restoring balance in the intestines is adherence to the principles of proper nutrition.
Food should be rich in dietary fiber and fiber. This is porridge, rye bread. After consultation with your doctor, you can include dietary fiber supplements in your diet.
All fermented milk products that are enriched with beneficial probiotics will be beneficial. Fruits and vegetables must be fresh.
You should eat often, but in small portions. Eliminate all foods that can cause flatulence. These are legumes, carbonated drinks, sweets.
Long breaks between meals should be avoided. All diets are excluded. During treatment, it is better to refrain from “dry drinks” and snacks on the run.
The list of prohibited products includes:
- fatty broths;
- sausages, sausages;
- pasta;
- alcohol;
- coffee;
- mushrooms;
- bakery;
- preservation, marinades.
You should drink it 1-2 hours after eating. This diet is recommended for a month after treatment.
Risk factors
People more prone to dysbiosis:
- after viral diseases;
- with diseases of the gastrointestinal tract;
- with weakened immunity;
- after taking antibiotics, hormones, chemotherapy;
- living in an unfavorable ecological zone;
- travelers.
In addition, children who are bottle-fed and during the period of introducing complementary foods are at risk.
Traditional therapy for dysbiosis
Herbal medicine will also help improve your intestinal health. Some types of herbs help to gently cope with stool disorders, improve intestinal motility, and have a calming and anti-inflammatory effect.
Dysbacteriosis often occurs due to frequent stress and emotional stress. Infusions of chamomile, valerian or mint help relieve tension without having a negative effect on the gastrointestinal tract.
Also, the following herbal infusions have proven themselves to be effective in eliminating abdominal discomfort:
- dill, eucalyptus and mint help reduce bloating and gas;
- flax seeds, plantain, dandelion help cope with constipation;
- lemon balm and St. John's wort will have an antiseptic effect and reduce pain;
- Oak root, St. John's wort and bird cherry are recommended for strengthening stool.
You need to take only fresh decoction. For this, 1-2 tbsp. spoons are brewed with boiling water and allowed to brew. It is better to do this in a small thermos. The drink should be consumed throughout the day in equal proportions.
Degree of severity of the disease and features of the clinical picture
The diagnosis takes into account the symptoms that determine the type of dyspepsia caused by a violation of the microflora in the intestines. According to the type of dyspepsia, putrefactive and fermentative forms of intestinal dysbiosis are distinguished. According to the severity of the clinical picture, 4 degrees of severity are distinguished.
The differences between each degree are presented in the table:
| I degree | II degree | III degree | IV degree |
|
|
|
|
The degree of severity is determined during the diagnostic process and is taken into account when selecting therapeutic methods, as well as in prescribing symptomatic treatment.