Cheilitis, or another name for “jam,” is an inflammatory process that occurs on the lips, affecting their skin, mucous membrane and red border. Cheilitis can be either an independent disease or a clinical manifestation of diseases of the internal organs and oral mucosa.
Symptoms of the disease have pronounced external signs, these include: peeling, swelling, redness, the formation of small bleeding ulcers, the formation of purulent crusts. The patient feels a burning sensation, pain when eating and when opening the mouth.
Often the disease has a long-term relapsing course. For young people, the prognosis is more favorable. They have a chance of complete self-cure, but in older people complications (for example, leukopathy) may occur, and there is also a high risk of cheilitis degenerating into a malignant neoplasm.
Causes
The causes of cheilitis largely depend on the level of health of the body. So, if a person has a healthy immune system, a rational healthy diet, then most pathological factors, such as injuries, unfavorable climatic conditions and others, are terrible for him. But still, among the main causes of cheilitis are:
- Injury to the mucous membrane of the lips with a violation of its integrity, especially frequent;
- Infection under the mucous membrane of the lips, mainly streptococci, staphylococci, candida fungi, herpes virus and others;
- Unusual and unfavorable climatic conditions for the body - ultraviolet radiation, very low or high air temperature, exposure to strong winds;
- Weakened immunity, which is most often facilitated by hypothermia, frequent stress, the presence of various diseases (especially infectious ones);
- Allergic factor - irritation of the lips by certain chemicals (lipsticks, denture material, toothpastes and others);
- The presence of diseases and pathological conditions such as atopic dermatitis, neurodermatitis, macrocheilitis, eczema, xeroderma, erythematosis, dermatoses, diabetes mellitus, tuberculosis, AIDS, psoriasis, lichen planus, anemia, hepatitis, hypovitaminosis (especially deficiency of vitamins B2 in the body, C and E), broken bite;
- Failure to comply with personal hygiene rules, including using someone else’s lipstick, toothbrush, dental floss, dishes and other accessories, touching lips and other parts of the face with unwashed hands;
- Bad habits – alcohol abuse and smoking.
By the way, the pathological plaque on the lips largely depends on the type of infection - yellowish (streptococci and staphylococci), whitish (Candida fungi).
What triggers the development of the disease
There is practically no protective layer on human lips, so they are highly susceptible to external factors. For this reason, people are often concerned about the drying out of the mucous membrane, which leads to the appearance of microcracks and further infection.
The most common causes of the problem are the following:
- changes in air temperature, sun, wind - these natural factors dry out the skin and it cracks,
The sun, wind, sudden changes in temperature can affect the condition of the lip mucosa - the use of low-quality lipstick or hygiene balms - the lanolin they contain can clog the pores with a secretion that does not allow the skin to breathe,
- dermatoses, allergic reactions - dangerous chemical compounds in contact with the surface of the epithelium cause rashes, cracks or wounds,
- the predominance in the diet of spicy, sour, salty or hot foods that irritate the epithelium and mucous membranes,
- congenital, acquired diseases of the thyroid gland, immunodeficiency states - these pathologies negatively affect the skin,
- skin tuberculosis, venereal infectious diseases, lichen,
- diseases of the central nervous system - because of them, patients may feel itching,
- chemotherapy,
- vitamin deficiency - a lack of nutrients in the body negatively affects the functioning of all its systems,
- mechanical damage.
If a child breathes through his mouth during sleep, his lips may become dry.
Sometimes pathology occurs in a child if he breathes through his mouth during sleep. However, if an adult has a chronic runny nose, he will also breathe through his mouth. With such a violation of the physiological state, the sensitive skin and oral mucosa dries out, then unpleasant defects appear.
Classification
Depending on the predisposing factors of formation, the disease can be:
- primary – develops independently and is not accompanied by symptoms of any other disease;
- secondary - is a consequence or part of the clinical picture of another pathology.
The primary category of this disease includes:
- glandular - such damage to the lips is caused by an increase in the volume of the salivary glands and their subsequent infection;
- exfoliative – only the red border of the lips is involved in the pathological process;
- allergic – based on the name it is clear that the main cause is a delayed allergic reaction;
- meteorological - its occurrence is caused by increased sensitivity to environmental conditions. Actinic cheilitis (the second name of the disease) is divided into dry and exudative.
Secondary, or symptomatic, varieties of such lip pathology are:
- atopic – considered one of the manifestations of atopic dermatitis;
- eczematous is a disease caused by eczema, which causes inflammation of the upper layers of the skin;
- candidiasis – the main pathogen is yeast-like fungi;
- hypovitaminosis – occurs due to a lack of B vitamins in the body;
- angular - is a consequence of the pathological influence of pathogenic microorganisms, for example, streptococci.
Symptoms
There are a number of varieties of cheilitis (see photo), each of which has characteristic symptoms. Cheilitis on the lips can develop as an independent disease, but sometimes it becomes a consequence of the appearance of pathologies of internal organs and systems.
The following symptoms are common to all forms of disease:
- manifestation of symptoms exclusively on the red border of the lips - signs of cheilitis do not appear either on the tissues surrounding the lips, or on the tongue, or in the oral cavity;
- burning, itching;
- Painful plaques or pus may ooze;
- the skin becomes covered with small cracks.
There are many types of cheilitis. The classification of cheilitis is based on symptoms and causes. The characteristic manifestations of different types of cheilitis can be found in the photo accompanying the article, and brief descriptions of each of the most common forms of pathology are presented below.
Catarrhal type
Catarrhal cheilitis is the most common and harmless of this group of diseases. Inflammation is caused by damage. Most often these are abrasions, scratches, microtraumas, damage by aggressive substances - bacteria penetrate through the wound, and the development of lip disease begins. The appearance of this type of cheilitis is also often caused by the habit of biting and licking lips outside in cold weather or in strong winds. Among the characteristic symptoms are:
- burning, itching, pulsation of the red border of the lips;
- the appearance of many scales and bleeding cracks;
- swollen, edematous lips of a rich crimson or reddish hue.
Meteorological cheilitis
Occurs as a result of prolonged exposure to cold air, scorching sun or exposure to strong winds. The dry form does not have pronounced symptoms; peeling and dryness may appear. When exudative, small painful wounds, blisters, and crusts form on the surface of the lips, which are accompanied by itching and burning.
The occurrence of atopic cheilitis in most cases is associated with dermatitis. The condition is characterized by the appearance of small rashes not only on the surface of the lips, but also on the elbows, neck, and face. The disease may be hereditary or develop against the background of allergic reactions to foods, cosmetics, and medications.
Macrocheilitis is often accompanied by paralysis of the facial nerve and develops due to the presence of infectious diseases or allergic reactions in the body. Genetic predisposition and the state of the immune system play an important role. Main signs: increase in lip size, itching, facial distortion.
Treatment of meteorological cheilitis begins with stopping or minimizing the adverse effects of meteorological factors. Local therapy involves the use of hormonal ointments and protective creams with a high UV filter. Patients with meteorological cheilitis are recommended to take vitamins B, PP, C and other vitamin complexes.
Exfoliative cheilitis
Disease of only the red border of the lips, accompanied by peeling. It is more common in women.
Among the causative factors are dysfunction of the nervous system - anxiety, depression. In addition, a connection has been established between increased thyroid function and exfoliative cheilitis. In recent years, the role of heredity and changes in the immune system has been recognized in the development of exfoliative cheilitis.
With the exfoliative form of cheilitis, there is no spread of the process to the mucous membrane or skin. The part of the red border of the lips bordering the skin and the area of the corners of the mouth are kept free from damage.
In the dry form, patients are bothered by dry lips, sometimes burning, and the appearance of scales that usually bite. This condition lasts for years.
Upon examination, the following is determined: one lip or both are dry, there are scales that are tightly fused in the center with a red border, their edges are raised. After removal of the scales, erosion usually does not occur; only a focus of bright redness is noted. After 5-7 days, mica-like scales form again. The course of the disease is long, without a tendency to self-heal.
The exudative form of exfoliative cheilitis is characterized by severe pain, swelling of the lip, and the presence of abundant crusts that make speech and eating difficult.
In the treatment of exfoliative cheilitis, the main thing is the effect on the psycho-emotional sphere. A consultation with a neurologist or psychoneurologist is necessary, followed by the prescription of sedatives and tranquilizers. If necessary, correction of the functioning of the endocrine glands is carried out. Local treatment of exfoliative cheilitis consists of laser therapy, ultrasound treatment in combination with hormonal drugs, and sometimes radiation therapy is used. To eliminate dry lips, use moisturizing hygienic lipsticks. All patients are recommended to undergo a course of vitamin therapy; autohemotransfusion, UVOC and other methods of increasing the body's reactivity have a positive effect on the course of cheilitis. Several months of complex therapy are enough to achieve complete cure; clinical improvement occurs earlier.
Eczematous cheilitis
This type of disease, also called atopic cheilitis, occurs due to local allergic inflammation. The provoking factor is the use of allergenic cosmetics, the presence of allergies to certain foods. A lack of riboflavin also provokes the development of eczematous cheilitis.
Granular cheilitis
It was first described in 1870. Its pathogenesis involves congenital or acquired proliferation of small salivary glands, which provokes their infection. There are two types of this disease:
- Primary granular cheilitis.
- Secondary granular cheilitis.
This disease affects people of both sexes, mainly after the age of 30, and it is noted that damage to the lower lip occurs in patients twice as often. Patients with chronic periodontal diseases, tartar and caries are at risk, as they contribute to infection of the dilated ducts of the salivary glands.
A direct connection has been established between the occurrence of primary granular cheilitis and the presence of a congenital anomaly in the functioning of the salivary glands. The salivary glands hypertrophy under the influence of various factors (dental pathology, periodontal disease, pathology of the dentition, gums, etc.), and the intensity of saliva production increases. According to one of the scientists' hypotheses, the appearance of the disease may be influenced by heredity.
Characteristic of secondary granular cheilitis is the fact that the resulting inflammation affects the glandular tissue. However, these are not typical cases.
Granular cheilitis has a specific clinical picture; its characteristic signs are red dots - dilated mouths of the salivary glands, from which drops of saliva are released (the “dew drops” symptom). The main complaints of patients are the presence of dryness, erosions and cracks. Dryness occurs due to the constant moistening of the lips with saliva and its evaporation. Then the skin of the lips gradually undergoes keratinization, starting from red dots and spreading further. If the disease lasts for a long time and cracks appear, this may be a harbinger of the formation of pre-cancer lesions. The resulting cracks can remain forever, as the elasticity of the skin of the lips is impaired.
A pyogenic (purulent) infection often penetrates the ducts of the salivary glands. Symptoms of granular cheilitis in purulent form are marked by swelling, pain, discharge of pus, and covering the lip area with thick crusts that are black-brown and yellowish-green in color. If the ducts of the glands are blocked, abscess formation may begin.
Treatment of glandular cheilitis involves the use of anti-inflammatory ointments. Tetracycline, erythromycin and oxolinic ointments are indicated; ointments with glucocorticosteroids also have a good effect. A radical method of treating glandular cheilitis is electrocoagulation of hypertrophied salivary glands or their surgical removal; good results are observed when using laser ablation. After treatment, to prevent relapses of glandular cheilitis, measures to eliminate dry or weeping lips, sanitize foci of chronic infection in the oral cavity and normalize the microflora of the oral cavity are indicated. Patients with glandular cheilitis should be monitored for some time after treatment to ensure timely prevention of relapses.
Atopic cheilitis
This type of cheilitis is a sign of atopic dermatitis or neurodermatitis.
A typical clinical sign of diffuse neurodermatitis is itching of the skin followed by the development of redness and scratching. In the development of atopic cheilitis, great importance is given to hereditary factors that can create conditions for the development of an allergic reaction. Allergens can be medications, cosmetics, food products, as well as bacterial and physical factors.
Patients with atopic cheilitis complain of itching of the lips, redness, and peeling of the red border of the lips. Damage to the corners of the mouth is typical. As the acute symptoms of inflammation subside, peeling and lichenification are observed. Infiltration and dryness of the corners of the mouth lead to the formation of cracks. Changes in the lips are combined with dryness and flaking of the facial skin.
When treating atopic cheilitis, it is necessary to eliminate irritating factors. Local treatment consists of using ointments with antipruritic, anti-inflammatory and antiallergic effects. Hormone-containing ointments are usually used. Antihistamines are taken internally - clemastine, fexofenadine, loratadine and others. During the treatment of atopic cheilitis, it is important to follow a hypoallergenic diet, excluding foods that sensitize the body from the diet: strawberries, red fish and caviar, spices, citrus fruits, spicy foods and alcohol.
Candida
Caused by fungi of the genus Candida in people who have the habit of frequently licking their lips. In this case, the lips become dry and prone to cracking, and infection occurs. Whitish thin scales form on the lips. These manifestations are accompanied by itching, severe pain, difficulty in eating spicy and hot foods.
Other types of cheilitis
A lip disease such as cheilitis is divided into more than 10 varieties. Each of them has its own characteristics - both in terms of symptoms and in matters of organizing the treatment of cheilitis. In addition to exfoliative, atopic and candidal types of the disease, a number of its forms are also distinguished. A list of frequently encountered ones is presented below:
- Allergic cheilitis - sometimes called eczematous. If the lips are inflamed, red, itchy and painful, and lichen-like crusts appear on the surface, then this is allergic cheilitis.
- Lupus cheilitis - the surface of the lips turns red, gray spots and erosions appear, and over time, atrophic processes of the red border develop. Symptom of lupus erythematosus. Treatment is effective only in combination with therapy for the pathology that caused it.
- Cheilitis in hypovitaminosis form. Scales and vertical cracks form on the red border, and a burning sensation and dryness are felt around.
How to treat cheilitis on the lips?
To effectively treat cheilitis, you must first identify the cause that caused the development of the disease. It is not recommended to independently select and carry out treatment for cheilitis - it is better to contact a specialist who, based on a comprehensive diagnosis, will select the optimal and effective therapeutic strategy.
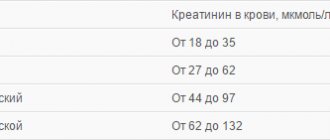
To identify the disease and determine its cause and type, diagnosis is necessary; the clinic usually carries out:
- skin tests and smears;
- Ultrasound of internal organs (thyroid, pancreas, liver, etc.);
- blood tests (general, biochemistry, antibodies, allergens, etc.) and urine;
- biopsy and histology of epithelial cells.
Treatment is selected according to the diagnosis:
1. General strengthening measures:
- systematic oral and facial hygiene;
- sanitation of the lip mucosa with aseptic solutions;
- getting rid of irritants (nicotine, alcoholic beverages, the habit of biting or licking lips, hypersalivation, contact with allergens, solar radiation, etc.);
2. Drug therapy
- local treatment, antibacterial or glucocorticosteroid ointment (as indicated);
- taking antihistamines;
- pain relief for severe pain;
- a course of antibiotics, antiviral, immunostimulating agents (depending on the type of cheilitis).
3. Physiotherapy:
- ultrasound;
- UHF;
- electrophoresis.
4. Surgical treatment:
- electrocoagulation;
- laser cauterization;
- cryodestruction.
Diagnostic features
If inflammation appears on the lip, it is advisable to visit a therapist, for children a pediatrician, if indicated, an infectious disease specialist, a dentist, or other specialized specialists. Diagnosing cheilitis is usually not difficult - a specialist will conduct an examination, listen to complaints and prescribe a series of tests. If the allergic nature of the disease is suspected, allergy tests may be recommended, and if plaque appears, it is advisable to take a scraping. To detect endocrine and other disorders that may cause the disease, biochemical blood tests and other diagnostic methods are often prescribed. In rare cases, a biopsy is required to differentiate cheilitis from other pathologies. This will help to exclude the malignant or precancerous nature of inflammatory formations and prescribe the correct treatment.
Drug treatment
All medications are prescribed exclusively by a doctor, since the form of cheilitis that has developed is of great importance. In some cases, antiviral agents are required (Bromonaphthoquinone, Acyclovir, etc.), in others, hormonal and antihistamine tablets (Loratadine, Clemastine), and in the third case, simply increasing the body’s general immunity and vitamin therapy is sufficient. The latter, by the way, is mandatory for every patient.
Be sure to select local remedies that can relieve inflammation, itching and other symptoms. Usually preference is given to ointments with hormones. The following medications help in treatment:
- Metrogyl Dent is classified as a dental gel with a broad antibacterial effect. It is often prescribed in severe cases because it not only reduces the symptoms, but also prevents further spread of the infection.
- Triderm ointment contains corticosteroids, so it is better not to use it for a long time. This remedy has very good effectiveness; as a rule, within 14 days the symptoms will become less pronounced.
- Flucinar. This medication has an affordable price and copes well with even the most complex types of cheilitis. However, it should only be used in combination with other medications.
- Mycozolon. It is prescribed if the disease is fungal in nature.
- Prednisolone ointment is intended for those types of disease that manifest themselves against the background of dermatitis, allergies, and also with the formation of weeping erosions.
- Zinc ointment. It is used for rapid healing of cracks and wounds. They should be pre-treated with antiseptics.
- Any healing ointments (Panthenol, Methyluracil, Vishnevsky ointment, Naftalan ointment, etc.) will promote rapid healing and relieve the inflammatory reaction. Additionally, they also relieve symptoms such as burning and itching.
If treatment for cheilitis is started in a timely manner and there are no signs of malignancy, the prognosis is favorable; a long course of cheilitis, on the contrary, increases the likelihood of developing precancerous and cancerous diseases.
Ointment that has shown effectiveness
Corticosteroid ointments have shown the greatest effectiveness in the treatment of cheilitis.
In dry forms of the disease they are used in the form of creams or ointments, in wet forms in the form of aerosols:
- Prednisolone ointment. Suitable for outdoor use. It has an anti-allergenic effect, relieves inflammation, swelling and helps reduce vascular permeability.
- Lorinden S. The drug has antifungal and antibacterial effects. N has shown high effectiveness in the treatment of dermatitis, eczema, dermatoses and other forms of skin diseases.
- Dexocort. The drug is available in the form of aerosols. Indicated for allergic skin diseases. The main contraindications to its use are bacterial, viral and fungal skin diseases.
- Hydrocortisone ointment. A product that is actively used for various forms of skin diseases: dermatitis, psoriasis, dermatosis and others. Has anti-allergenic and anti-inflammatory effects.
All medications should be used only after consultation with a doctor, according to the instructions for use.
Folk remedies
If the pathology is not of a serious nature, then traditional medicine can be used to eliminate it. Below are some home remedy recipes that will help eliminate inflammation on the lips.
Calendula decoction recipe
Ingredients:
- dry calendula - 1 tbsp;
- water - 200 ml.
Preparation: Boil water. Pour the calendula into a jar, pour boiling water over it, and close the lid well. Let the broth brew.
Usage: Perform the procedure before going to bed. Soak a clean cloth in the warm broth and apply it to your lips for a quarter of an hour. Pat your lips dry with a towel.
Chamomile infusion recipe
Ingredients:
- dry chamomile - 1 tbsp;
- water - 100 ml.
Preparation: Boil water. Pour boiling water over the herb and let the broth brew.
Usage: Soak gauze in a warm broth, apply it to the sore lips, wait a quarter of an hour.
Result: Chamomile eliminates inflammation and itching, relieves redness, softens hard crusts.
Recipe with oak bark
Ingredients:
- crushed oak bark - 1 tbsp;
- water - 100 ml.
Preparation: Boil water. Pour boiling water over the bark, then place the mixture in a water bath for 30 minutes.
Usage: Soak gauze in warm broth. Apply it to your lips for ten minutes. Dry your lips with a towel and lubricate them with oil.
Other folk remedies:
- If large cracks appear in the corners of your lips, lubricate them with soft beeswax. Perform this procedure every 3 hours, and after a few days you will notice how the crack begins to heal. But remember, it is forbidden to open your mouth too much while eating or talking.
- Kalanchoe, like aloe, neutralizes minor inflammation and tightens cracks in the corners of the lips. For treatment, use a large cut leaf of the plant. Apply the cut to the inflamed area and secure with a bandage. After 2 hours, remove the patch; do not drink or eat while wearing it.
- Oil masks will help fill the lack of vitamin E and collagen. If your lips are dry, lubricate them with olive, linseed or any other vegetable oil. These foods contain large amounts of vitamin E.
Possible complications
Cheilitis on the lips is a disease that, in the case of improperly organized treatment, or the complete absence of a therapeutic course, is dangerous for the development of complications.
They are as follows:
- the formation of benign cysts inside the mucous glands of the lips, which change the shape of the tissues, creating the effect of chronic edema;
- in conditions of low-grade inflammation, degeneration of epithelial cells and the development of lip cancer cannot be ruled out;
- it is possible that a bacterial, viral, or fungal infection may occur, which will aggravate the course of the disease and lead to the appearance of abscesses and the release of purulent masses;
- decreased quality of life, feeling of severe pain, inability to fully accept sour, salty, pickled foods;
- transition of the inflammatory process to the oral mucosa with the formation of trophic wounds;
- gingivitis of the gums in the area of the front lower and upper teeth;
- necrosis of epithelial tissue, which will require surgical intervention to remove the affected part of the lip.
Timely treatment of cheilitis on the lips can completely eliminate the risk of the above complications. The prognosis for recovery is positive, but provided that therapy is carried out under the supervision of a specialized doctor on an outpatient basis or in an inpatient department.
Treatment of the disease at home can lead to the appearance of scars, deformities, and keloids on the lips.
Article design: Oleg Lozinsky
Prevention
In order to avoid encountering this unpleasant disease, patients at risk are recommended to:
- be examined by a dentist at least once every six months and promptly remove sharp edges of teeth, tartar, and damaged dental crowns that injure the lip;
- dentures should be made only from high-quality materials to suit the individual characteristics of the patient’s jaw apparatus;
- give up bad habits that destroy your health;
- do not stay in the sun for a long time, use protective equipment, including oil-based lipstick;
- pay attention to and begin treatment of chronic diseases of the gastrointestinal tract, endocrine system, and internal organs.
Cheilitis is an inflammatory disease of the lips, but there are so many varieties of it that it is impossible to independently understand which form of symptoms appeared. The diagnosis can only be made by an experienced specialist, and the sooner treatment is prescribed, the better for the patient.
Forecast
Timely contact with a doctor and therapy under his supervision are the main conditions for a quick recovery. It must be remembered that this disease can spread to nearby healthy skin if you delay and try to cure it yourself. By the time you visit the hospital, the infection will have become more resistant to drugs, which means that the course of treatment can last 3-7 months.
The most dangerous thing about delay is that signs of transformation of normal tissue into malignant tissue may appear, which increases the risk of being diagnosed with precancerous and cancerous conditions.
Bartholinitis Hepatitis C: first signs and treatment regimen Psoriasis Pancreatitis Glaucoma Menopause in women
When to see a doctor
Cheilitis is not a dangerous disease, but the lack of timely treatment can lead to irreversible consequences and complications. Degeneration of the tissues and mucous glands of the lips cannot be ruled out, which can lead to a change in their shape and inflammatory deformation of the soft tissues.
In this regard, it is recommended to consult a dentist, dermatologist or surgeon in the first days after discovering single or multiple signs of cheilitis. Self-therapy at home can lead to progression of the disease.