Colpitis is an inflammation of the vaginal mucosa. In some cases, it spreads to the vulva. Most often, colpitis develops in women of childbearing age. Also, due to improper genital hygiene, little girls can also get it. And in postmenopausal women, when the level of female sex hormones in the body drops sharply, atrophic colpitis most often develops.
In most cases, inflammation is caused by sexually transmitted infections, and a little less often by nonspecific microorganisms - Escherichia coli and Pseudomonas aeruginosa, streptococci and staphylococci.
Colpitis must be treated under the supervision of a gynecologist. Otherwise, the disease will first become sluggish and then chronic. With stress, hypothermia, and hormonal changes, unpleasant symptoms will reappear, causing pain, weakness and anxiety.
The infection can travel up the genitourinary tract and cause inflammation of the bladder and kidneys. The inflammatory process in the genital tract provokes adhesions, vaginal dryness, and discomfort during sex.
Chronic colpitis negatively affects the ability to conceive and provokes the occurrence of ectopic pregnancy.
Classification of colpitis
Depending on the type of pathogen that provoked the disease, colpitis is divided into specific and nonspecific. Specific vaginitis is caused by gonococci, trichomonas, fungi and other infections.
According to the localization of the initial infectious focus, colpitis is divided into:
- primary, when the process immediately develops in the vagina;
- secondary, in case of infectious agents entering the vagina from other places (ascending - from the surface of the vulva and descending - from the uterine cavity).
The course of the disease is determined by the following forms:
- acute colpitis;
- subacute colpitis;
- chronic colpitis;
- sluggish vaginitis;
- latent (hidden) vaginitis;
- asymptomatic colpitis.
Separately, senile or atrophic (age-related) colpitis is distinguished.
Antiseptic drugs
It is not advisable to treat colpitis in women with antiseptics alone, since external treatment of the vagina will only relieve symptoms. Even if all the unpleasant signs of the disease completely disappear, the trigger itself will remain in the body.
Miramistin
It is a gentle analogue of the widely used antiseptic called Chlorhexidine. Miramistin is available in the form:
- Irrigation solution (with a special long nozzle);
- Ointments.
But chlorhexidine can be found in Hexicon suppositories (for colpitis, vaginal suppositories are the optimal form of use).
The vagina is irrigated directly with the solution every day (for 14 days) every 2 hours. You can also insert vaginal tampons soaked in 50 ml of Miramistin. Change 2-3 times a day (do not leave it overnight).
Hexicon can also be purchased in solution form and injected into the vagina 5-10 ml 2 times a day. However, it must be taken into account that, unlike Miramistin, the Chlorhexidine solution in Hexicon can provoke itching and burning. Therefore, it is much more convenient to use 2 candles. per day for 10 days.
These medications not only eliminate the main symptoms of vaginitis, but also speed up the process of restoring normal vaginal microflora.
Fluomizin
Available in the form of vaginal tablets. The treatment period is 6 days. It is necessary to administer one suppository once a day (before bedtime).
A distinctive feature of Fluomizin is that it can be used without fear throughout pregnancy. However, you need to make sure that the cause of the disease is bacteria that are sensitive to the action of dequalinium chloride (the active component of the medicine for colpitis).
Vaginal microflora is normal
Normally, in a healthy woman of childbearing age, the vaginal microflora consists of 95–98% lactobacilli or Doderlein bacilli. Doderlein rods break down glycogen, which is “received” from desquamated epithelial cells of the superficial layer of the vaginal mucosa. When glycogen is broken down, lactic acid is formed, due to which the pH of the vaginal environment shifts to the acidic side (4.5 or less). The acidic vaginal environment is a kind of protection against pathogenic microbes, as many of them are not able to grow and reproduce in such conditions. Lactobacilli also produce hydrogen peroxide and a number of antibiotic-like substances, which strengthens the defense and prevents the colonization of the vagina by unwanted microorganisms.
In addition to lactobacilli, bifidobacteria live in the vagina, which also protect it from infection. The vital activity and number of lactobacilli depends on the production of estrogen. Therefore, with the onset of premenopause, when estrogen production decreases, the vaginal mucosa becomes thinner and the number of lactic acid bacteria decreases, which leads to the development of age-related colpitis.
Also, under various other conditions that lead to a decrease in lactobacilli in a healthy and young woman, the vagina is very quickly populated by “invaders” - pathogenic microorganisms.
In addition to lacto- and bifidobacteria, other microorganisms are present in small quantities in the vagina:
- streptococci;
- enterococci;
- peptococci;
- staphylococci;
- bacteroides;
- fungi of the genus Candida and others.
Diet
A healthy diet for bacterial colpitis is necessary, first of all, to restore normal microflora in the vagina, as well as in the intestines.
Fermented milk products (kefir, sour cream, fermented baked milk, etc.) are rich in live bifidobacteria and lactobacilli They are the first to be included in your diet.
In addition, it is advisable to consume foods high in polyunsaturated acids (fish oil, shrimp, trout, cod, salmon, etc.).
During the course of bacterial vaginitis, a woman’s body may lack some vitamins and minerals. To make up for their deficiency, you should consume as much as possible :
- vitamin B (nuts, legumes, liver, spinach, garlic, mushrooms);
- vitamin C (sea buckthorn, currants, oranges, lemons, etc.);
- vitamins A and E (sweet potato, broccoli, seaweed, dried fruits, etc.);
- magnesium (seafood, nuts);
- zinc (buckwheat and oatmeal, beans, peas, poultry, lamb, etc.);
- calcium (cheese, cream, barley, etc.).
During treatment of bacterial vaginitis, as well as for its prevention, it is recommended to limit the consumption of sweets and alcohol, which can aggravate the treatment.
Causes of colpitis
As already noted, the disease is caused by the colonization of the vagina by pathogenic microorganisms or the activation of opportunistic pathogenic flora. Opportunistic pathogenic flora is represented by microbes that, in a normal state of immunity, are in equilibrium with the normal flora, but the balance is very fragile. Once the immune system is weakened, this flora becomes pathogenic. The following types of microorganisms can cause vaginitis:
- Trichomonas;
- fungi of the genus Candida;
- cytomegalovirus;
- myco- and ureaplasma;
- numerous intestinal flora;
- Proteus;
- staphylococci;
- streptococci;
- corynobacteria;
- gonococci;
- chlamydia;
- tuberculosis bacillus and others.
In girls, vaginitis can be caused by pathogens of childhood infections that penetrate the vagina through the bloodstream (secondary vaginitis). These can be pathogens of measles, diphtheria, scarlet fever and others.
But in order for the disease to begin to develop, certain conditions or predisposing factors are required:
- non-compliance or, on the contrary, excessive passion for intimate hygiene;
- hidden sexually transmitted infections;
- promiscuous sex life;
- endocrine pathology (thyroid diseases, diabetes mellitus);
- trauma to the genital organs (rough sexual intercourse, deflowering);
- tight synthetic underwear;
- pregnancy and menstruation (hormonal changes and weakened immunity);
- menopausal age;
- oncological diseases and their treatment (chemotherapy, radiation);
- acquired and congenital immunodeficiency states;
- lack of vitamins;
- allergic reactions;
- antibiotic treatment, especially uncontrolled;
- taking hormones;
- abnormalities of the genital organs (gaping genital cleft or prolapse of the vaginal walls);
- damage to mucous membranes during childbirth;
- ovarian hypofunction;
- use of an intrauterine device;
- improper and irrational nutrition;
- diseases of the digestive tract;
- spontaneous and artificial termination of pregnancy;
- curettage of the uterine cavity.
Clinical picture
The clinical picture of the disease is quite varied and is largely determined by the type of pathogen and the form of its course. The main signs of vaginitis are:
- burning, itching in the vagina;
- the amount of vaginal discharge increases significantly, the nature of which is different (curdled, purulent, homogeneous milky, foamy, bloody or mixed with blood);
- the discharge has an unpleasant odor
- possible redness and swelling of the labia;
- aching or nagging pain in the lower abdomen;
- pain during coitus;
- dysuric disorders (frequent and painful urination);
- temperature increase.
In the case of acute colpitis, all manifestations are pronounced: burning and itching are significant, heaviness in the lower abdomen suggests problems with internal organs, discharge is abundant. In severe cases of the disease, a significant increase in temperature is possible, up to 38 degrees or higher. As a rule, this picture is characteristic of specific colpitis (gonorrheal or trichomonas).
With chronic colpitis, the picture is less bright, the symptoms are erased. The disease lasts a long time, with periodic exacerbations. The discharge becomes moderate, serous or serous-purulent.
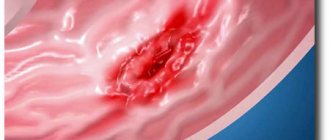
When examined on a chair in the mirrors, swelling, hyperemia and “looseness” of the vaginal mucosa are revealed. Petechial and pinpoint hemorrhages are noticeable on the mucosa; reddish nodules (infiltrates) and erosive areas may appear. In advanced cases, the cervix is involved in the inflammatory process, which leads to cervicitis or pseudo-erosion.
Trichomonas colpitis
This form of the disease is caused by Trichomonas, which is sexually transmitted. The household route of infection with Trichomonas, as some patients prefer to think, is impossible, since the pathogen quickly dies in the external environment. The symptoms of Trichomonas colpitis are so pronounced that the diagnosis is not difficult. Characterized by significant leucorrhoea, which has a very unpleasant odor. The discharge is usually foamy and has a yellowish tint. If nonspecific microflora attaches, the discharge becomes green. The infection spreads very quickly, affecting the cervix, the uterus itself and the urethra, which is manifested by dysuria and pain in the lower abdomen. Sexual intercourse is unpleasant and even painful, accompanied by discharge mixed with blood.
Atrophic colpitis
With atrophic colpitis, there are practically no symptoms. The disease progresses sluggishly, patients may or may not complain. The most common concerns are burning and itching, a feeling of “tightness” in the vagina and its dryness. Sexual intercourse is painful, after which bloody discharge appears or even minor bleeding occurs. Due to a decrease in the number of lactobacilli, which perform a protective function, opportunistic microorganisms actively multiply in the vagina, which provoke local inflammatory processes and increased discharge. Such discharge is watery and contains an admixture of blood after certain procedures (vaginal washing and douching, gynecological examination). When examined in the speculum, a pale pink, thinned mucosa with many pinpoint hemorrhages is revealed. In many cases, vaginal dryness makes insertion of speculum difficult.
Etiotropic therapy
As with any other infectious process, the key to a successful outcome is adequate etiotropic therapy, that is, the use of antibacterial agents. At the moment, their choice is quite wide.
Nonspecific bacterial vaginitis is no exception; it is increasingly being treated with new generation antibiotics.
However, the goal of therapy remains to normalize the quantitative composition of the facultative flora.
Antibiotics for vaginitis are used both systemically (that is, orally) and locally (that is, intravaginally). Experts give greater preference to local therapy .
This ensures a minimum of adverse reactions, convenience and ease of use, a reduction in the number of contraindications, and the possibility of use for concomitant diseases.
In addition, frequent use of antibiotics for chronic infection leads to changes in the composition of the patient’s own microflora and the emergence of resistant bacteria, which subsequently require adjustment of therapy.
Diagnostics
After collecting anamnesis and complaints, an objective examination of the patient is carried out, which includes:
- examination of the mucous membrane of the vaginal walls and cervix in gynecological speculum (discharge, its consistency and smell, the presence of ulcerations on the vaginal walls and pseudo-erosion or cervicitis on the cervix are assessed) - the examination is carried out without prior preparation (do not wash);
- bimanual palpation of the uterus and appendages to identify complications of vaginitis (endometritis and/or adnexitis);
- examination of the labia, urethra, clitoris and inner thighs for swelling and ulceration, maceration and fissures (flowing discharge may irritate the listed structures).
Laboratory tests are required:
- microscopy of secretions obtained from the cervical canal, posterior vaginal fornix and urethra (allows you to determine the bacterial flora, including Trichomonas and fungi, gardnerella and gonococci;
- bacteriological culture of vaginal discharge to identify the pathogen and determine its sensitivity to antibiotics (if possible, after a 3-week course of antibiotic therapy;
- PCR diagnosis of major sexually transmitted infections (Trichomonas, gonococci, herpes, cytomegalovirus, chlamydia and ureaplasma).
Colposcopy is prescribed and performed according to indications.
Additionally, general blood and urine tests, blood tests for syphilis and HIV infection are prescribed.
Treatment
Treatment of colpitis in women involves eliminating the pathogens that caused the disease, restoring normal vaginal flora and stimulating the immune system. Self-medication of vaginitis is not allowed. Therapeutic measures are prescribed to all patients, regardless of their age and form of the disease, or the presence of concomitant pathology.
General recommendations
During the period of illness, the patient is advised to maintain sexual rest. Sexual intercourse not only aggravates the discomfort, but also contributes to the rise of infection and re-infection. You also need to adhere to a certain diet. You should avoid spicy and salty foods (in the case of candidal vaginitis and sweets), and alcohol consumption is prohibited. The diet should be dominated by fresh vegetables and fruits, and lactic acid products.
If a specific pathogen is identified (for example, Trichomonas, gonococci), treatment is also prescribed to the sexual partner. In severe cases of the disease (significant increase in temperature and severe discomfort in the vagina), sexual rest is prescribed.
Compliance with intimate hygiene is mandatory. You need to wash yourself at least twice a day, in the case of menstruation, after each pad change. If a girl develops vaginitis, she should be washed after each visit to the toilet.
Vaginal douching
A vaginal douche or douching is prescribed for a period of 3–4 days, since a longer course of procedures promotes desquamation of epithelial cells of the surface layer of the mucosa and disrupts the healing process. Antiseptic solutions are used for douching:
- solution of potassium permanganate in a ratio of 1/5000 - 1/8000;
- 0.5% solution of rivanol;
- decoction of sage or chamomile;
- chlorophyllipt solution;
- soda solution (dilute 2 teaspoons in a liter of boiled water) is effective for viscous purulent leucorrhoea.
Douching is carried out three times a day. At the same time, sitz baths with decoctions of medicinal herbs or antiseptics are prescribed.
Vaginal suppositories and tablets
Suppositories for colpitis and vaginal tablets are used as local therapy:
Nonspecific vaginitis
- polygynax (contains polymyxin, neomycin and nystatin) – has anti-inflammatory, antibacterial and antifungal effects, prescribed for a course of 7 – 14 days twice a day;
- terzhinan (composition: ternidazole, neomycin, nystatin and prednisolone) – a similar effect, the course of treatment is 10 days, 1 suppository is administered per day;
- Vokadine (composition: povinone-iodine) course of therapy is 1 – 2 weeks, 1 suppository is administered per day;
- mycogynax (composition: metronidazole, chloramphenicol, nystatin and dexamethasone) - prescribed for 1 - 2 weeks, 1 - 2 suppositories per day.
Gardnerellosis
- "Dalacin" ointment (consists of tinidazole, sinestrol, vitamin C and lactic acid) - course of treatment for 7 - 10 days, tampons with ointment are inserted into the vagina in the morning and before bedtime;
- ginalgin (consists of metronidazole and chlorquinaldol) - duration of therapy is 10 days, 1 suppository per day;
- Klion-D (composition: metronidazole and miconazole) – antimicrobial and antifungal action, administered 1 vaginal tablet once a day for 10 days.
Trichomonas vaginitis
- metronidazole in the form of vaginal suppositories (ginalgin and Klion, Flagyl and Trichopolum) - course of treatment for 10 days, 1 suppository daily;
- tinidazole (active ingredient fasigin) – the course of treatment is similar;
- Hexicon - suppositories are administered 3 times a day for 7 - 20 days;
- neo-penotran (consists of metronidazole and miconazole) - course 1 - 2 weeks, 1 suppository twice a day.
Treatment courses for trichomoniasis are carried out three times, after each menstruation.
Candidal vaginitis
- nystatin – in the form of suppositories for 1 – 2 weeks;
- clotrimazole – a vaginal tablet is administered daily for 6 days;
- canesten (0.5 g) – single injection of a tablet into the vagina;
- pimafucin (natamycin) 1 suppository twice a day for a week;
- pimafucort (composition: natamycin, neomycin and hydrocortisone) - administered as an ointment on tampons into the vagina twice a day for 2 weeks.
Genital herpes
- acyclovir (analogues: Zovirax, Herpevir) - vaginal tampons with cream are administered up to 4 - 5 times a day, the course is about 10 days;
- 0.5% bonafton ointment – treatment duration is 10 days, applied to tampons and administered intravaginally 4 – 6 times a day;
- Viferon - suppositories are administered intravaginally in the morning and evening, course 5 - 7 days;
- a-interferon - suppositories are administered twice a day, course 1 week.
Read more about the treatment of genital herpes.
Systemic therapy
In case of severe colpitis or in case of chronicity of the process, treatment agents are prescribed, used orally or intramuscularly. In the case of specific colpitis caused by gonococci, intramuscular administration of cephalosporin antibiotics (ceftriaxone, cefixime) or tetracycline is indicated. For vaginitis caused by trichomonas, nitroimidazoles (trichopolum, tinidazole, metronidazole) are prescribed. Severe nonspecific colpitis requires the prescription of broad-spectrum antibiotics - amoxiclav (penicillins) or azithromycin (macrolides). In the treatment of colpitis of fungal origin, the following drugs are used: fluconazole, orungal, pimafucin, ketoconazole and others.
Atrophic colpitis
In the case of senile vaginitis, hormone replacement therapy is usually prescribed. Treatment with hormones can be both local and systemic. For local therapy, estrogen preparations are used in the form of vaginal tablets or ointments (Ovestin, estriol). The course of treatment lasts 2 weeks and is repeated if necessary. Cliogest, Climodien, Angeliq and other drugs (tablets, patches) are prescribed as systemic hormone therapy. Treatment is long and continuous (5 years). If a secondary infection occurs, treatment is carried out according to the principles of treatment of acute colpitis with the prescription of etiotropic drugs locally, and, if necessary, orally.
Restoration of vaginal microflora
Restoring the natural flora of the vagina refers to the second stage of treatment for vaginitis:
- bifidumbacterin - intravaginally 5 - 6 doses, which are diluted with boiled water and administered daily or 1 suppository twice a day - the course of treatment is 10 days;
- bifikol – intravaginal administration of 5 doses daily for up to 7 days;
- Lactobacterin – intravaginal administration of 5 doses in a course of 10 days;
- acylact – 1 suppository daily for 10 days.
At the same time, multivitamins and immunomodulators are prescribed.
Traditional methods
Folk remedies do not lose their relevance in the treatment of diseases. Traditional methods are used as an addition to the main (drug) treatment of colpitis. For douching, decoctions and infusions of medicinal herbs are used:
- chamomile (2 tablespoons boil in 1 liter of water for 15 minutes, filter the broth and cool);
- coltsfoot (leaves), stinging nettle, St. John's wort, thyme, buckthorn bark - take equal quantities of all herbs, mix and pour 2 tablespoons of the mixture into 0.5 liters of boiling water, leave for 2 hours, strain and cool;
- a decoction of yarrow, sage, rosemary and oak bark;
- calendula infusion;
- infusion of eucalyptus leaves;
- infusion of succession;
- juniper decoction and others.
What exactly to treat?
The main goal of treating colpitis in women is to suppress the growth of pathogenic microflora and restore balance.
If about 40 years ago streptococci were of primary importance, now this place has been taken by more antibiotic-resistant staphylococci.
At the moment, a mixed infection (that is, a mixed infection) is more often observed, when bacteria, protozoa and fungi are associated.
This combination creates unique resistance to therapy and promotes the creation of protective biofilms on the surface of the vaginal mucosa.
Pathogens become insensitive to monotherapy, the frequency of relapses increases, and the inflammatory process becomes chronic.
Prevention
To prevent the development of the disease, a number of rules should be followed:
- do not forget about condoms during casual sexual intercourse;
- maintain intimate hygiene (wash twice a day);
- refuse narrow and tight underwear, as well as synthetic underwear;
- lead a healthy lifestyle (giving up bad habits, playing sports, taking multivitamins, especially in the winter and spring);
- control weight (prevent obesity and excessive weight loss);
- use pads and tampons without fragrances;
- do not get carried away with douching;
- use detergents for intimate hygiene with a neutral environment and without fragrances;
- strengthen immunity;
- having one permanent sexual partner.