A long-awaited pregnancy is a wonderful event in the life of a married couple. But, unfortunately, it does not always proceed well, and complications are possible even in the very early stages. One of them is hydatidiform mole - a rather rare disease that occurs when the fertilization process is disrupted and is accompanied by pathological development of placental tissue. According to average estimates, one in a thousand pregnant women experiences a hydatidiform mole.
Hydatidiform mole belongs to the group of trophoblastic diseases, since abnormal changes occur in the outer layer of embryonic cells (trophoblast), which are responsible for implantation of the embryo and development of the placenta. With hydatidiform mole, the chorionic villi degenerate and a benign tumor (chorionadenoma) is formed - a mass of cysts, which are clusters of bubbles with liquid contents. The size of the bubbles can range from a millet grain to a large grape. If there are few bubbles, and not the entire fleecy surface of the embryo is affected, they speak of an incomplete (partial) form of hydatidiform mole. Partial hydatidiform mole most often develops in the second trimester of pregnancy. Sometimes it is possible to give birth to a living, viable child, but in most cases the fetus dies.
A complete hydatidiform mole is characterized by a pathological proliferation of cysts, with degeneration of all villi occurring, and the embryo dies at an early stage of development, before placental circulation is established. The most severe course of the disease is accompanied by the germination of vesicles into the thickness of the muscular layer of the uterus. Once in the bloodstream, particles of hydatidiform mole are spread throughout the body and form metastases in other internal organs, most often in the lungs and vagina.
The causes of hydatidiform mole are not reliably known, but there is a hypothesis that this disease occurs when a healthy or anucleate egg is fertilized simultaneously by two sperm or one sperm with a double set of chromosomes. Consequently, an embryo formed in such an anomalous way, instead of the standard set of 46 chromosomes (23 maternal and 23 paternal), has, respectively, either a triple set of chromosomes (23 maternal and 46 paternal) or a double set (46) of paternal chromosomes with the complete absence of maternal ones.
What is a “hydatidiform mole”?
Hydatidiform mole is a deviation in the development of the fertilized egg. If this pathology occurs, the formation of the placenta does not occur. The chorionic villi degenerate into bubbles, inside of which there is liquid. It has a yellowish color and consists of:
- amino acids;
- human chorionic gonadotropin;
- albumin.
The diameter of the bubbles does not exceed 25 ml. Hydatidiform mole occurs in 0.02-0.8% of pregnancies. There are several types of the disease, which include:
- Complete or simple hydatidiform mole. The disease is characterized by pathological changes throughout the chorion.
- Partial hydatidiform mole. Pathological changes affect the chorion only partially.
- Destructive hydatidiform mole. This is the most severe form of the disease. It is malignant in nature.
The first type of pathology appears in a woman during the first trimester of pregnancy. In the presence of this form of the disease, the fetus dies and then dissolves.
Partial hydatidiform mole may appear after the first trimester of pregnancy. In this situation, the pregnancy is not terminated. There is a possibility that it will end in a live birth of a child. In most cases, birth occurs prematurely. However, the baby may appear on time. If the pathology appears during a multiple pregnancy, it can affect only one placenta or both of them.
Complications of the condition, prognosis for mother and baby
The prognosis for pregnancy and birth of a baby with hydatidiform mole is, unfortunately, unfavorable. Even with a partial hydatidiform mole, molar pregnancy is futile due to chromosomal abnormalities and severe fetal developmental abnormalities.
Termination of pregnancy is often a serious psychological trauma for the woman and her relatives. However, expectant management and prolongation of pregnancy are inappropriate due to the high risk of serious complications for the mother’s body.
The most common complication of hydatidiform mole is uterine bleeding. Chronic blood loss entails the development of severe anemia and oxygen starvation of organs and tissues. Massive blood loss can become a threat to the mother's life if urgent measures are not taken. The second most common complication is preeclampsia, which is expressed in a persistent increase in blood pressure, edema and loss of protein in the urine. After removal of the hydatidiform mole, these phenomena disappear on their own.
Photo: https://pixabay.com/photos/woman-person-desktop-work-aerial-3187087/
In general, the prognosis after treatment for hydatidiform mole is favorable and subsequent pregnancy develops safely. But still, in 15% of cases, the development of a malignant trophoblastic tumor with the spread of metastases to the lungs, brain, liver and other organs is possible. If a trophoblastic tumor is confirmed, chemotherapy and observation by a gynecological oncologist are indicated.
Nonspecific complications of molar pregnancy after instrumental removal include infectious and inflammatory diseases of the uterus (endometritis, metroendometritis). Like any intrauterine intervention, uterine curettage may cause female infertility in the future. However, the potential benefits far outweigh the possible risks.
If an unplanned pregnancy could not be avoided within the specified period after removal of a hydatidiform mole, a thorough examination and monitoring of the mother’s condition and the development of the baby will be required in the future. According to statistics, women with a history of molar pregnancy are more likely to experience complications in the form of incoordination of labor and postpartum hemorrhage.
What does a hydatidiform mole look like from a photo?
If a woman has developed a hydatidiform mole, the villi of the outer membrane turn into cysts. This is the name given to bubbles containing liquid. Additionally, proliferation of the villous epithelium is observed. Pathology can lead to fetal death. To better understand what a hydatidiform mole looks like, it is recommended that you familiarize yourself with the photo.
If the pathology develops in the first 1-2 weeks of pregnancy, all primary villi of the fetal egg are degenerated. Severe hyperplasia is present in the trophoblast layers. In this situation we are talking about the appearance of 1 form of pathology. Sometimes this type of disease is called early hydatidiform mole. This is explained by the timing of the onset of the pathology. During this period of pregnancy, hydatidiform mole is characterized by:
- proliferation of trophoblasts lining the villi from the inside;
- swelling of the villi and their increase are observed;
- the villous epithelium is not defined or undergoes dystrophic changes;
- there are no blood vessels in the villi;
- the embryo is resorbed.
If the pathology develops from 3 months to 34 weeks inclusive, usually only part of the chorionic villi is degenerated. In this case, we are talking about the so-called incomplete hydatidiform mole. In this case, the villi that have not degenerated have a normal appearance. Their blood supply is preserved. In this case, the fetus is observed in the uterus. However, pathology can lead to his death.
In the case of multiple pregnancies, the problem may affect only one placenta. At the same time, 2 is able to remain in its normal form and continue to function.
Invasive hydatidiform mole can occur against the background of a complete or partial type of pathology. Varieties of the disease have the following symptoms:
- bubbles can grow into the muscular layers of the uterus;
- villi can penetrate blood vessels and the lymphatic network, grow through the serous cover of the uterus and myometrium, spreading throughout the body, and also affect internal organs;
- the placental structure of the villi is preserved.
The destructive form of the disease is the most severe. It occurs in 5-6% of cases.
The first signs of a hydatidiform mole
If a woman has developed a hydatidiform mole, one of the signs of the disease is early toxicosis. It may be accompanied by an increase in temperature, as well as moisture in the skin. The patient often feels nauseous. Vomiting occurs against the background of nausea. It appears due to severe disturbances in water and electrolyte balance.
An alarming sign is the appearance of bloody discharge. They occur as a result of uterine bleeding. Bloody discharge may occur in early pregnancy and continue until childbirth or surgery to remove the egg. The discharge is dark in color and liquid-like in thickness. They are not abundant, but appear regularly.
Another sign is an abnormal size of the uterus. So, a three-month period can correspond in size to 5 months.
Is pregnancy possible after illness?
Hydatidiform mole, the consequences of which can be very dire, is not a disease that leads to complete infertility. But it is worth considering that throughout the entire period of observation of the patient by the oncologist, she is not recommended to become pregnant. The main method of contraception at this time is taking hormonal drugs. This is due to their positive effect on the regulation of ovarian function, impaired as a result of the disease.
It is necessary to plan your next pregnancy no earlier than 2 years after the operation. This is especially true if the patient has undergone chemotherapy. After conception occurs, a woman should be under the close supervision of medical personnel, since there is a high probability of complications during pregnancy and childbirth.
A patient who has suffered a hydatidiform mole and wants to become pregnant again should not set herself up for a worse outcome and the inability to have children. Thanks to modern medicine, almost 70% of women experience the joy of motherhood after overcoming this disease.
Symptoms and signs of hydatidiform mole
Symptoms of hydatidiform mole may manifest differently in different women. The fact is that pathology can develop at different stages of pregnancy. The forms of the disease also differ. All this affects the clinical picture of the pathology.
Usually, a woman who is faced with a problem begins to worry about uterine bleeding. The discharge is dark in color. Bleeding ranges from minor to heavy. Symptoms of toxicosis occur. Women often mistake them for signs of pregnancy. The patient is often bothered by nausea and vomiting. She may experience increased drooling and dizziness. No appetite. Against this background, exhaustion may occur.
In severe cases, hydatidiform mole can grow into the walls of the uterus. This leads to a violation of its integrity, which in turn provokes intra-abdominal bleeding. Symptoms require immediate hospitalization and adequate therapy. Otherwise, there is a risk of death.
The visual size of the uterus does not correspond to the duration of pregnancy. This can be confirmed by visual examination and ultrasound. A woman suffering from pathology has bilateral fluid ovarian cysts. Their size can reach 10 cm or more. Cysts are easily detected during ultrasound. However, this symptom does not appear in all women who experience hydatidiform mole. There is no treatment in this situation. They will disappear on their own after the uterine cavity is cleared of hydatidiform mole.
HCG in pathology is several times higher than normal. During treatment, the doctor will check this indicator without fail until it returns to normal. Even when the hCG level returns to normal, the woman will still have to undergo this test regularly for six months. The action is performed for preventive purposes. Symptoms of hydatidiform mole can appear in the early stages of pregnancy and mimic its symptoms. Therefore, diagnosing the problem during this period is quite problematic.
If the disease becomes malignant, the blisters can spread to other organs, mainly the lungs. The prognosis in this case is unfavorable. Quite often death occurs. For this reason, it is important to detect pathology as early as possible and begin its treatment. This will allow us to count on the fact that the process will regress irrevocably, and the woman’s health will suffer minimally. There are other complications of the disease, which include:
- the occurrence of infertility;
- the appearance of intrauterine infection;
- septicemia;
- the occurrence of thrombosis;
- amenorrhea.
Diagnostics
The disease requires differential diagnosis with acute polyhydramnios, pregnancy with more than one fetus or against the background of myomatous nodes, spontaneous abortion and ectopic pregnancy. After collecting anamnesis and complaints, an examination is carried out at a gynecological clinic, during which the following is revealed:
- the size of the uterus exceeds the size of the expected gestational age;
- heterogeneous structure of the uterus: against the background of a softened uterus, nodular compactions are revealed;
- in 50% of cases, bilateral luteal ovarian cysts are palpated (with an increase in ovarian size of more than 6 cm), which appear within the first 2 weeks and are considered an unfavorable prognostic sign;
- the presence of tumor-like formations in the vagina and vulva.
With a large abdomen, reliable signs of pregnancy are not detected (fetal heartbeat, palpation of large parts of the fetus).
Additional diagnostic methods are used:
- Ultrasonography. Reveals significant size of the uterus, the absence of an embryo or fetus, a characteristic sign is the presence of tissue of a homogeneous fine-grained structure (a “snow storm” symptom), luteal cysts. The diagnostic value of ultrasound is 100%.
- Chest X-ray. Allows you to detect metastases in the lungs.
- Hysterosalpingography. HSG allows you to clarify the diagnosis and monitor the effect of chemotherapy. In the hysterogram, in the invasive form, the contour penetration of the contrast is visualized at the site of villi penetration into the myometrium.
- Diagnostic laparoscopy, hysteroscopy. Carried out if necessary.
- Testing the level of hCG in the blood. In non-pregnant women, hCG is normally absent in the blood serum. During gestation, hCG appears on the 8th day after conception, and its peak occurs on the 60th day and is 5000 - 10000 units. If the hCG level remains high after 12 weeks, a hydatidiform mole is suspected.
- Immunochemical method. Consists in determining trophoblastic beta globulin in the blood. When this disease develops, its level is 76–93%.
- Histological method. Helps determine the morphological variant of the disease (material - scraping from the uterine cavity).
Causes and prevention of signs of hydatidiform mole
Mole is a pathology of a chromosomal nature. It is impossible to find out the reasons for the development of the disorder. Doctors have put forward several theories to shed light on the causes of the pathology. During the process of fertilization of the egg, the maternal genes are lost. At the same time, the paternal ones replace them, duplicating themselves. Pathology can also appear if an egg that lacks a nucleus is fertilized by 2 sperm. According to other theories, viruses and parasites can cause the problem.
Separately, there are categories of women who are at greater risk of developing the disease than others. The risk group includes girls who are not yet ripe for pregnancy. The problem may arise if conception occurred at the age of 14-15 years. The risk of pathology is also present if a woman is over 40 years old. Other reasons that increase the likelihood of a hydatidiform mole are:
- the woman gave birth many times;
- conception occurred between close relatives;
- immunodeficiency is present;
- A woman’s diet lacks some microelements and vitamins.
The phenomenon is quite rare. On average, the pathology is detected in 1 pregnant woman out of a thousand. However, the indicator is quite relative.
As mentioned earlier, the exact causes of the disease have not been established. Therefore, there is no specific prevention of hydatidiform mole. However, experts have identified a number of measures that can reduce the risk of pathology. The list includes:
- timely consultation with a doctor in case of pregnancy. You must register before 12 weeks;
- a woman must completely stop taking drugs, alcohol, and smoking;
- It is necessary to regularly visit an obstetrician-gynecologist. During the 1st trimester of pregnancy, she should be seen by a doctor once a month. In the second trimester, the number of visits increases to 1 time every 2-3 weeks. In the third trimester, you need to visit a specialist once every 7-10 days;
- pregnancy must be planned consciously. It is recommended that you first undergo all necessary examinations;
- It is recommended to take folic acid for 3 months before planned pregnancy and during the 1st trimester.
Hydatidiform mole is a disease characterized by the proliferation of the outer layer of embryonic cells (trophoblast), filling the entire uterine cavity. According to the degree of damage to the fetal membrane, hydatidiform mole is classified into complete and incomplete.
Content:
1. What is hydatidiform mole? 2. Forms 3. Complete hydatidiform mole 4. Partial hydatidiform mole 5. Incomplete form 6. Symptoms 7. Classification 8. Causes 9. Signs 10. Treatment 11. Diagnosis 12. Ultrasound 13. Consequences 14. Chemotherapy treatment 15. Pregnancy after hydatidiform mole skidding 16. Solving the problem 17. Prevention
What is this
Hydatidiform mole is one of the rare complications of pregnancy. It occurs as a result of abnormalities during the fertilization process that lead to abnormal development of the cells that form the placenta. Hydatidiform mole belongs to a group of diseases collectively called “trophoblastic tumors.” These tumors are usually benign (noncancerous). And although they can spread outside the uterus, they are treatable.
In a normal pregnancy, a fertilized egg contains 23 paternal and 23 maternal chromosomes. In the complete form of hydatidiform mole, the fertilized egg contains no maternal chromosomes at all, while the chromosomes of the paternal sperm are duplicated, so that the result is that the egg contains two sets of paternal chromosomes and none of the maternal ones. In this case, during the subsequent development of pregnancy, the embryo does not form, the amniotic sac and normal placental tissue are absent. Instead, the placenta forms as a mass of cysts that resemble a bunch of grapes. These cysts are clearly visible on the ultrasound screen.
In most cases of incomplete hydatidiform mole, the fertilized egg has a normal set of maternal chromosomes (23 chromosomes), but also contains a double set of paternal chromosomes. Thus, a fertilized egg has 69 chromosomes instead of the normal 46. (This can happen when sperm chromosomes are duplicated, or when two sperm fertilize the same egg.) In this case, some normal placental tissue forms along with cystic placental structures. Of course, pregnancy loss under such circumstances is a serious moral injury. However, with proper treatment and medical supervision, it is unlikely that any associated pathologies will develop in the future.
Forms
Types of hydatidiform mole:
- complete hydatidiform mole (simple) - pathological changes occur throughout the chorion;
- partial hydatidiform mole - these changes involve only part of the chorion;
- destructive hydatidiform mole - altered villi grow into the wall of the uterus. The most severe form of manifestation of mole, since the development of dangerous intra-abdominal and external bleeding is possible, and the tumor itself acquires a malignant course.
Full
A complete hydatidiform mole is special in that it occurs at the beginning of pregnancy, during the first three months. During normal conception, the egg contains 23 paternal and 23 maternal chromosomes. A fertilized egg with a complete hydatidiform mole contains only paternal chromosomes and no maternal ones. Because the paternal chromosomes are duplicated, the egg produces two sets of only the paternal chromosomes. Subsequently, the embryo does not form, the fertilized sac and natural placental tissue are absent. Hydatidiform mole is clearly visible on ultrasound, since the placenta forms in the form of a mass of cysts and in appearance they resemble a bunch of grapes.
Partial
With partial hydatidiform mole, as a rule, triplodia is observed, i.e. cells carry 69 chromosomes. The extra set of chromosomes is of paternal origin. A fetus with a partial hydatidiform mole also has signs of triplodia: intrauterine retention and numerous malformations, for example, syndactyly and hydrocephalus.
The clinical picture of partial hydatidiform mole is less pronounced. In most cases, it resembles that of an incomplete or failed abortion. Partial hydatidiform mole is often diagnosed only after histological examination of material obtained from the uterine cavity.
Incomplete form
Incomplete hydatidiform mole occurs when the fertilized egg contains the maternal set of chromosomes (23 chromosomes) and double the paternal set of chromosomes.
In this case, instead of 46 chromosomes, the fertilized egg contains 69. The main cause of partial hydatidiform mole occurs when the paternal chromosomes are duplicated, or when the egg is inseminated by two sperm. Because of this, a cystic placental structure and natural placental tissue is formed. Partial hydatidiform mole develops in a woman after the first trimester.
Losing a pregnancy under these circumstances is a serious moral injury. Once the correct treatment is prescribed and the doctor carries out observation, the development of any pathologies associated with trophoblastic disease is unlikely. An ultrasound can determine the size of the uterus if a hydatidiform mole is suspected.
Invasive hydatidiform mole develops at full and incomplete degrees. The bubbles penetrate deep into the falling membrane, but retain the placental structure of the villi.
Symptoms
Diagnosing this disease does not cause any difficulties, because the signs of hydatidiform mole are quite classic.
To detect a disease such as hydatidiform mole, diagnostics must be done. It is done when, during a gynecological examination, a woman has a large uterus, which is abnormal for this period. So, with this pathology, a three-month pregnancy period corresponds in size to five months. The thickness of the uterus is tight-elastic. The gynecologist does not see the exact signs of conception, such as fetal movements and heart sounds.
A diagnostic sign of hydatidiform mole is a woman’s complaints of uterine bleeding. Bleeding begins in the early stages and continues until the due date, or until surgery to remove the egg. Discharge during a hydatidiform mole is dark-colored bleeding that has a liquid consistency. Egg vesicles are released along with the blood. Bleeding is not profuse, but if it is regular, it can lead to the formation of iron deficiency anemia.
Characteristic signs of hydatidiform mole are:
- bloody discharge caused by detachment of the placenta from the decidua,
- an increase in the size of the uterus caused by the accumulation of blood and the growth of the chorion,
- preeclampsia (rarely eclampsia), accompanied by an increase in the size of the uterus,
- vomiting in pregnant women caused by severe disturbances of water and electrolyte balance,
- thyrotoxicosis (in less than 10% of pregnant women), accompanied by tremor, tachycardia, increased temperature and humidity of the skin,
- embolism of the branches of the pulmonary artery,
- theca lutein cysts of the ovaries, caused by an increase in the level of ovarian stimulating hormones and disappearing on their own after a few months.
In most cases, hydatidiform mole is detected during abortion or suspected miscarriage (due to bleeding). In some cases, symptoms are mild. A more distinct clinical picture is observed with complete hydatidiform mole.
Classification
Hydatidiform mole can be complete or incomplete (classical or partial). They differ in the degree of damage to the fetal membrane: with a complete hydatidiform mole, changes occur in the entire fetal membrane, and with incomplete mole, changes occur only in its area. A separate category includes destructive hydatidiform mole, which is considered a malignant pathology.
Most often, a complete hydatidiform mole occurs between 11 and 25 weeks of pregnancy and is characterized by the absence of any signs of embryonic or embryonic development. The first clinical symptom of this type of disease is an enlarged uterus that does not correspond to the gestational age. You can visually verify the presence of vesicles and edematous chorionic villi.
For incomplete hydatidiform moles, the characteristic time of detection is gestational age 9–34 weeks. The main symptom is the size of the uterus, which is smaller than that corresponding to the current stage of pregnancy. It is also possible to visually identify fragments of the fetus, placenta and edematous chorionic villi. In some cases, the transition of an incomplete hydatidiform mole to a malignant formation is possible.
Simultaneously with a simple hydatidiform mole, the development of an invasive type of hydatidiform mole is possible. At the same time, this diagnosis can be confirmed only by removing the uterus or the area with metastases (signs of invasion are observed in the villi of the myometrium and other tissues). With this type of hydatidiform mole, there is swelling on the chorionic villi, the absence of embryonic vessels and the invasion of the myometrium by proliferating syncytio- and cytotrophoblast elements. The lesion quickly extends deep into the myometrium and can cause severe intraperitoneal bleeding.
Causes
The main factors that increase the risk of developing hydatidiform mole are:
- insufficient level of carotene in food,
- lack of vitamin A,
- a note in the medical history of luteal cysts,
- age over 40 years.
The likelihood of the formation of this pathology increases significantly in the presence of several risk factors. Another cause of hydatidiform mole is uniparental disomy, which occurs when the maternal genomes are lost and the paternal genome is duplicated.
In some cases, this pathology develops in full form as a result of fertilization of an anucleated egg by two sperm. Incomplete hydatidiform mole can occur when an egg is fertilized by two sperm, characterized by a single set of maternal and double set of paternal chromosomes. In both of these cases, the fetus dies.
Signs
The main signs of hydatidiform mole are bleeding that occurs in the 1st trimester of pregnancy and an enlarged uterus. The woman is also tortured:
- nausea,
- vomit,
- gestosis in the 1st trimester of pregnancy,
- stomach ache.
There are also no signs of pregnancy such as parts, heartbeat and movements of the fetus, and with ultrasound, the absence of the fetus and the presence of small cystic tissue are observed in the uterus. Hydatidiform mole in a malignant form is characterized by the penetration of its tissues into the structure of the uterine wall and further spread with blood into the vagina and lungs. Its signs are bloody discharge from the uterus and pain in the abdomen, lower back and sacrum that continues even after removal of the hydatidiform mole. There is also no uterine contraction.
Treatment
Treatment of a benign form of the disease leads to the removal of the egg using vacuum aspiration. During this process, the contents of the uterus are sucked out with a metal narrow-cylindrical tip and an electric vacuum pump.
HCG during hydatidiform mole exceeds the norm. After egg removal, it is recommended to check your hCG levels every week. It should drop to 100 mIU/ml. After hCG has decreased to this norm, its determination continues every month for 6 months.
Chemotherapy for hydatidiform mole is also used. The dose of drugs is prescribed by the doctor strictly individually. After treatment, you should protect yourself from pregnancy for one year. In case of severe hydatidiform mole, it is necessary to first treat complications, such as:
- water and electrolyte disturbances,
- thyrotoxicosis,
- anemia,
- preeclampsia.
Only after the normal state of the pregnant woman is restored, the uterus is emptied. With a complete hydatidiform mole, treatment depends on the woman’s desire to have children in the future. If you plan to have a baby in the future, then vacuum aspiration should be used, regardless of the size of the uterus. It is done as follows:
- Before anesthesia, oxytocin is administered, which improves uterine contractions,
- rapid expansion of the cervical canal occurs, as it causes heavy bleeding,
- rapid vacuum aspiration is performed,
- The uterine cavity is scraped, ensuring complete removal of the blisters.
If patients have Rh-negative blood, they are given anti-Rh(D) immunoglobulin during surgery. In less than 10% of cases of hydatidiform mole removal, there is a need for chemotherapy. The probability of developing malignant tumors after the elimination of complete or partial hydatidiform mole is 8% or 0.5%, respectively. After treatment for hydatidiform mole is completed, pregnancy and childbirth proceed normally, and the risk of re-development of hydatidiform mole does not exceed 1%. For women who fall into this 1%, the following is produced:
- once a trimester ultrasound of the pelvis,
- depending on the characteristics of the pregnancy, examination of the ovum or placenta,
- within 6 weeks after completion of pregnancy, determination of hCG levels.
Heavy bleeding and an enlarged uterus larger than the size corresponding to the 20th week of pregnancy may be an indication for laparotomy with removal of the uterus (if the woman does not want to have children). The ovaries are not removed.
Diagnostics
When diagnosing a hydatidiform mole, the patient's complaints are taken into account. For example, they indirectly indicate this pathology:
- bloody issues,
- purulent or serous leucorrhoea,
- pain in the abdomen, chest, lumbar region,
- headaches leading to vomiting, blurred vision, development of paresis, etc.,
- neurological symptoms.
Anamnesis analysis is also very important. Characteristic pathologies accompanying hydatidiform mole are:
- preeclampsia registered in early pregnancy,
- incessant vomiting in a pregnant woman,
- thyrotoxicosis,
- embolism of the branches of the pulmonary artery.
An important diagnostic tool is ultrasound. In this case, hydatidiform mole may be indicated by:
- enlarged uterus,
- absence of fetus,
- lack of fetal heartbeat,
- missing parts of the fetus
- observation of a homogeneous small cystic substance,
- observation of thecalutein ovarian cysts.
Other methods for diagnosing hydatidiform mole are:
- clinical examinations (blood test for platelets, erythrocytes, leukocytes, etc.),
- biochemical studies (coagulogram, determination of creatinine level, liver function test, etc.),
- gynecological examinations (determining the shape, hardness and size of the uterus, examining areas of cyanosis of the cervix and vaginal mucosa, etc.),
- endoscopic methods (laparoscopy, hysteroscopy),
- radiological methods (chest x-ray, hysterosalpingography),
- determination of karyotype,
- radioimmunological and biological techniques,
- CT scan,
- NMRI.
Ultrasound
The size of the uterus during a hydatidiform mole is larger than the size characteristic of the expected period of pregnancy (50% of cases). Ultrasound visualizes many liquid bubbles of various diameters (a picture of a snow storm), which appeared as a result of proliferation of the chorion epithelium with a change in its shape, location and the formation of liquid vacuoles; the fertilized egg turns into a cluster-like conglomerate of heterogeneous ultrasonic density. In half of the cases, cysts can be detected in the ovaries. The doctor must rule out partial hydatidiform mole - a combination of local hydatidiform mole and pregnancy.
Ultrasound is the most accurate method for diagnosing hydatidiform mole. In this case, the diagnosis is based on the detection of multiple echo signals in the uterine cavity, creating a picture of a “snow storm”. The longer the pregnancy, the more accurate the diagnosis, which is associated with an increase in the size of the vesicles (the picture becomes more clear).
Ultrasound diagnosis of partial hydatidiform mole during pregnancy of more than 12 weeks is also not difficult, if the fetus is developing normally. With minor changes in the chorion and/or severe fetal degeneration, identifying this pathology is often difficult.
Differential diagnosis of hydatidiform mole should be carried out with uterine fibroids with secondary changes in the myomatous nodes (edema, necrosis). There may be difficulties in differentiating a hydatidiform mole from a non-developing pregnancy with significant regressive changes.
Consequences
The main complication of the disease is the development of chorionic carcinoma. This is a trophoblastic disease of a malignant form, which is characterized by the proliferation of pathological tissues in the uterus, liver, lungs and brain. And this already leads to death.
There are several stages of gestational tumors:
- the hydatidiform mole itself,
- characterized by the presence of malignancy within the uterus;
- the so-called placenta bed - localization of the tumor in the muscles of the organ and at the placenta attachment;
- non-metastatic tumor - germination of similar tissues into the uterus after abortion, childbirth or hydatidiform mole; metastatic tumors with a good prognosis - the malignant tumor does not leave the uterine cavity (a positive outcome of the disease is possible if the last pregnancy was less than 4 months ago, there are no metastases in the brain and liver, the patient has not had chemotherapy, the level of beta-hCG does not exceed the norm) ;
- metastatic tumors with a poor prognosis - cancer spreads beyond the uterus to other organs.
In addition to this pathology, hydatidiform mole has several other negative consequences. For example:
- Inability to develop subsequent pregnancies (infertility). This consequence is observed in 30% of women who have had the disease.
- Amenorrhea is the complete or partial absence of menstruation. This pathology develops in almost 12% of patients.
- Septic diseases.
- Thrombosis.
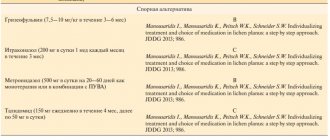
Chemotherapy treatment
Previously, there was a practice of mandatory chemotherapy for all patients who had a hydatidiform mole. Currently, this procedure is recommended only for women with an increased risk of developing chorionepithelioma. This danger is detected in women without a certain decrease in chorionic gonadotropin titers after getting rid of hydatidiform mole. If there is no progress within a month, chemotherapy is vital. In addition to high hCG levels, indications for chemotherapy are diagnosed choriocarcinoma and detection of metastases. Treatment of trophoblastic tumors is carried out in clinics prepared for this, and you should choose a clinic with good statistics on the treatment of such diseases. The treatment process begins a course of chemotherapy, depending on the research of the tumor. Chemotherapy is also carried out during bleeding that has not stopped; in this case, the chemotherapy procedure is combined with hemostatic therapy.
Hydatidiform mole is characterized by gynecologists as a serious disease that requires particularly close monitoring. Identifying the causes and undergoing a course of treatment for such a disease is mandatory. Recurrence of hydatidiform mole occurs in almost 20% of cases, but if you strictly follow all the doctor’s recommendations, it is quite possible to avoid a relapse, and the pregnancy will be completely full.
In any case, the patient who has suffered a mole is under the supervision of an oncology gynecologist for a certain time. After the illness, hCG levels are analyzed monthly for 1.5 years. During such a period, a woman needs to protect herself from pregnancy, preferably hormonal contraceptives - they will help restore normal ovarian function.
If the rehabilitation period proceeds normally, after two years the woman receives approval for a new pregnancy. At the same time, monitoring of a pregnant patient who has suffered a hydatidiform mole in the past, for obvious reasons, should be more closely in order to avoid the risk of relapse, severe pregnancy and bleeding.
Modern medicine allows 70% of women who are faced with the problem of hydatidiform mole to avoid dangerous consequences and fully carry and give birth to a child during the next pregnancy. Therefore, the happiness of motherhood with such a complication does not become impossible; it is only slightly delayed.
Pregnancy
When the hydatidiform mole is removed, the woman is registered for another 1-1.5 years. During this control period, you need to carefully monitor to ensure that pregnancy does not occur. The best method of planning pregnancy is hormonal contraceptives, which it is advisable to discuss with your gynecologist. Thanks to the hormonal effect on the body, this method will positively regulate the functioning of the ovaries, which could have been disrupted during the operation and complications in general.
The next pregnancy should be under strict control both from the woman and from the medical team. personnel. This is necessary because the likelihood of complicated childbirth and pathologies in the development of pregnancy has now increased.
Conceiving after chemotherapy or surgery should be planned no earlier than a year later!
Solution
After the diagnosis of “hydatidiform mole”, the treatment of which is aimed at removing the tumor from the uterine cavity, is confirmed, the woman is sent to the hospital. If the disease has no complications and the gestational age does not exceed 12 weeks, then a curettage procedure is performed. To do this, the cervix is stretched, which provides better access to its cavity, and all uterine contents are removed using a curette (special instrument).
Vacuum aspiration is used even in cases where the uterus is of a size corresponding to 20 weeks of pregnancy. This procedure involves suctioning out the contents of the cavity using special equipment. It is often performed together with curettage.
When the volume of the uterus increases to a size that corresponds to 24 weeks of pregnancy, a hysterectomy (removal of the uterus) is performed. Also, indications for surgery include thinning of its walls, perforation by hydatidiform mole, and the presence of metastases in the lungs or vagina. In this case, the ovaries are not removed.
After removing the hydatidiform mole from the uterine cavity, its tissue is sent for histological examination to exclude chorionepithelioma. If this procedure shows the malignancy of the formation, the level of hCG after a hydatidiform mole tends to increase, and foci of metastatic origin are found in the lungs, then the patient is prescribed chemotherapy.
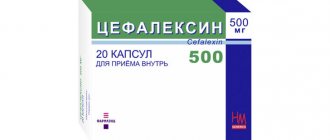
To treat the pathology, the drugs “Methotrexate” and “Dactinomycin” or a drug combining these two drugs – “Leucovorin” - are used. The main direction of action of these medications is to destroy cancer cells. These medications are prescribed until the level of hCG and the menstrual cycle are normalized, and pathological foci in the lungs and uterus disappear. After getting rid of these symptoms, the patient is prescribed several more preventive courses of chemotherapy with the same drugs.
In some cases, radiation therapy in the form of X-rays and other types of radiation may be necessary. It is carried out both externally, using devices, and from the inside. In the latter case, so-called radioisotopes are used, which produce radiation into the area where the malignant cells are located using thin plastic tubes.
Prevention
There is no specific prevention of hydatidiform mole, since the true causes of this disease have not been established.
Indirect measures to prevent hydatidiform mole can be considered:
- conscious planning of pregnancy, undergoing all recommended examinations in advance;
- complete cessation of smoking, drinking alcohol and drugs;
- taking folic acid for 3 months before planning pregnancy and during the first trimester of pregnancy;
- regular visits to an obstetrician-gynecologist (once a month in the 1st trimester, once every 2-3 weeks in the 2nd trimester and once every 7-10 days in the 3rd trimester);
- timely registration of a pregnant woman at the antenatal clinic (up to 12 weeks of pregnancy).
Tweet Pin It
Treatment of signs of hydatidiform mole
Treatment of hydatidiform mole during pregnancy depends on the individual characteristics of the course of the pathology, the period of gestation of the child, as well as the type of disease. In some cases, the fetus can be saved. However, the disease often leads to miscarriage or the need to remove the fertilized egg. If an accurate diagnosis is made, the woman is often offered to undergo minor surgery. During this procedure, curettage of the uterus is performed. The action is carried out in order to remove remnants of pathological tissue. Follow-up is then required for 8 weeks after surgery. The woman will have to undergo regular tests and ultrasound examinations every two weeks.
After the hydatidiform mole has been removed from the uterus through surgery, the level of hCG in the blood is monitored. The value of the indicator should gradually fall. This will be the main sign that the pathological processes in the uterus have stopped. If a negative hCG value is obtained, the test must be taken again. Actions are performed to ensure that the disease is truly cured. Additionally, the woman must undergo examination by a gynecologist-oncologist.
If an ultrasound shows that hydatidiform mole activity is observed, and an X-ray examination of the lungs indicates metastatic lesions, chemotherapy is administered. After remission is achieved and laboratory parameters return to normal, 2-3 additional courses are administered. The action is performed for prevention.
A patient experiencing a hydatidiform mole should be monitored by an oncologist for another year. The level of hCG in the blood is monitored monthly. It is not recommended to plan pregnancy during this period. The best means of preventing its onset are hormonal contraceptives. They allow you to normalize ovarian function after completing a course of chemotherapy and getting rid of the disease. Treatment is applied until the menstrual cycle returns completely to normal.
If there is no need for chemotherapy, and treatment was carried out in other ways, doctors recommend abstaining from pregnancy for a period of time. In other situations, the period is extended to 12 months. If conception occurs during this period, the level of hCG will certainly increase. This will lead to the fact that doctors will not be able to reliably determine the cause of the incident. It must be taken into account that hydatidiform mole can recur. The probability of this is 1-2%. However, reoccurrence of the pathology is still possible. In the vast majority of cases, the pathology does not in any way affect the ability to have a child in the future. A mother who has had the disease can give birth to a healthy child. The chance of premature birth also does not increase.
Laboratory research
To confirm the diagnosis, a woman submits:
- blood for hCG, the level of which is significantly increased in PZ;
- analysis of thyroid hormones, the function of which is disrupted when pregnancy has developed;
- blood chemistry. With this disease, the functioning of the liver and kidneys is disrupted, the level of creatinine, residual nitrogen, proteins, urea, bilirubin, transaminases, and alkaline phosphatase changes.
A transvaginal ultrasound of the uterus is required.