Causes of yersiniosis
Yersiniosis is a disease caused by Yersinia enterocolitica, characterized by a fecal-oral transmission mechanism, polymorphism of clinical symptoms (intoxication, damage to the gastrointestinal tract and joints, exanthema).
The causative agent of intestinal yersiniosis was isolated in 1939 in the USA by R. Gilbert. The first human diseases caused by Y. enterocolitica were registered in 1962-1966. in France, Belgium, Sweden, Czechoslovakia. Yersiniosis is registered everywhere. The disease is more common in Northern and Western Europe, Great Britain, Japan, USA, Canada and Russia. In the USA and Western Europe, intestinal yersiniosis ranks seventh in the structure of acute intestinal infections, and third or fourth among the bacterial pathogens that cause them. In Ukraine, sporadic cases and even epidemic outbreaks of intestinal yersiniosis are recorded. Y. enterocolitica belongs to the family Enterobacteriaceae, genus Yersinia, which includes several species of bacteria, of which only Y. enterocolitica, Y. pseudotuberculosis, Y. pestis are common in human pathology.
Y. enterocolitica is a gram-negative, motile, rod-shaped bacterium, has a capsule, grows on ordinary nutrient media, and produces endotoxin. Yersinia is resistant to the environment and is capable of reproduction in a fairly wide temperature range (from 2 to 40 ° C). The optimal temperature for growth is 2-5 °C, so they actively reproduce at the temperature of household refrigerators and winter vegetable stores, which contributes to the contamination of various products, especially vegetables, by Yersinia during their storage. Bacteria are killed by boiling, drying, exposure to sunlight and disinfectants. Pasteurization does not always inactivate Yersinia.
Antigenic differences make it possible to distinguish 6 biotypes and 76 serotypes of the pathogen. Y. enterocolitica is characterized by significant pathogenicity due to various factors:
- adhesion,
- colonization on the surface of the intestinal epithelium,
- enterotoxigenicity,
- invasiveness and cytotoxicity, which are expressed to varying degrees in different serotypes and strains of the pathogen, explain the diversity of clinical forms of intestinal yersiniosis.
Yersinia enterocolitis shares common antigens with other enterobacteria, which may contribute to the formation of corresponding antibodies and complicate serological diagnosis. Pathogenic enterocolitic Yersinia have heterogeneous antigens, related antigens of various organs and tissues, which leads to the formation of autoantibodies and multiple organ lesions.
Intestinal yersiniosis refers to saprozoonotic infections, in which the existence of the pathogen as a species requires a parasitic phase in the body of animals, and the possibility of independent life in the environment contributes to the long-term persistence of yersinia outside the macroorganism.
The main reservoir of Y. enterocolitica in nature is soil. There is an opinion that in the soil ecosystem, pathogenic Yersinia have their own hosts, which ensure the continuity of the epizootic process. Various aquatic organisms can be hosts of Y. enterocolitica, and temperature, humidity, and soil chemical composition affect the life span of Yersinia, their virulence and biochemical activity.
Secondary reservoirs of infection are rodents, agricultural (pigs, cattle, rabbits, etc.) and animals (cats, dogs), poultry. The main source of infection for people is farm and domestic animals, and less commonly, rodents. This type of yersiniosis in animals occurs in the form of carriage and manifest forms (diarrhea, mastitis, generalized infection). The mechanism of infection of intestinal yersiniosis is fecal-oral. Routes of transmission: food, water and household. Typically, humans become infected by consuming animal products contaminated with Y. enterocolitica (milk, dairy products, meat, chicken carcasses, eggs), as well as vegetables and fruits. Waterborne infection is less common; it is observed when drinking contaminated water from wells, open reservoirs, natural sources, and in some cases, tap water. Occasionally, the source of infection can be a sick person or a bacteria carrier, and then under certain conditions (hospital, children's group, sanatorium, family) household transmission of Y. enterocolitica is possible.
Since the pathogen enters the human body orally, the pathogenesis of yersiniosis is determined by the following successive stages:
- Infection is the penetration of a pathogen; Most Yersinia overcome the protective barrier of the stomach, where catarrhal-erosive gastroduodenitis develops.
- Entry of Yersinia into the intestines, their reproduction, local inflammatory reaction, penetration of the pathogen into the lymph nodes; subsequently, Yersinia accumulates in the intestine, where adhesion to the epithelial cells of the ileum and cecum occurs, Y. enterocolitica penetrates the epithelial cells, cytotoxic damage to the cytoplasm and bacterial proliferation on the surface of the epithelium are observed. Enterotoxigenic strains of Y. enterocolitica secrete a heat-stable enterotoxin, which activates adenylate piclase of enterocytes with the accumulation of intracellular concentrations of biologically active substances (cAMP, cGMP), which leads to disruption of water-electrolyte balance and absorption. The accumulation of Yersinia in the intestine causes the formation of an inflammatory focus with the formation of erosions, purulent-necrotic plaques, and microabscesses. Terminal ileitis and sometimes appendicitis develop. Penetration of Yersinia into regional lymph nodes causes mesadenitis, as well as the occurrence of microabscesses. In the appendix, the inflammatory process is often catarrhal in nature, but the development of destructive forms of the disease with subsequent development of peritonitis is possible. At this stage, the infectious process may be completed, in which case localized forms of the disease are observed. But in the presence of highly virulent strains of Y. enterocolitica, with a decrease in the body’s reactivity and the failure of local protective factors, a generalization of the process can develop, unfolding in an invasive or non-invasive way.
- Bacteremia - with the invasive route of generalization of infection, mesadenitis is followed by bacteremia, toxinemia, bacterial-toxic damage to many organs and systems, primarily the liver, spleen, lymph nodes, kidneys, joints, heart, lungs, and nervous system.
- Repeated generalization, formation of new foci of inflammation, autoimmune and allergic reactions. The presence of specific granulomas leads to secondary bacteremia with the formation of secondary foci of inflammation, which leads to relapses of the disease, secondary focal forms (pyelonephritis, arthritis, meningitis, myocarditis, erythema nodosum, etc.), protracted and chronic course. In some cases, Y. enterocolitica can play the role of a “trigger” in stimulating immunopathological processes with the development of systemic diseases (Reuther’s disease, Crohn’s, Gunnar-Sjögren’s disease, rheumatoid arthritis, autoimmune thyroiditis and hepatitis, endo- and myocarditis, pericarditis).
- Freedom from infection. The final phase of pathogenesis—elimination of the pathogen from the body, which leads to recovery—occurs as a result of an increase in the phagocytic activity of leukocytes and the formation of specific antibodies (cellular-humoral immunity). Immunity after yersiniosis is unstable, recurrent diseases have been described.
Manifestations of yersiniosis are characterized by polymorphism. Diseases of varying degrees are characterized by an acute onset, intoxication, catarrhal syndrome, damage to the digestive canal and joints, exanthema, enlargement of the liver and lymph nodes. The incubation period lasts from 15 hours to 7 days (on average 2-3 days). Gastrointestinal forms are registered more often. The disease begins acutely with the following symptoms:
- abdominal pain (moderate or intense, constant or cramping), which is localized in the middle part of the abdomen, epigastric region or right iliac region,
- sometimes with nausea and vomiting,
- stool is loose and foul-smelling, from 4-5 to 20 times a day, in severe cases contains moderate admixtures of mucus and blood.
Dehydration is possible, which, however, is very rarely accompanied by the development of significant hemodynamic changes. Along with gastrointestinal manifestations, symptoms of intoxication are observed:
- chills,
- increase in body temperature to 38-39 °C,
- headache,
- general weakness, body aches, myalgia.
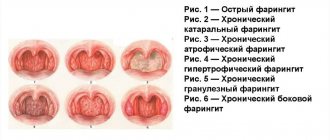
Some patients are bothered by a slight sore throat, moderate runny nose; They exhibit hyperemia of the oral part of the throat, similar to granulosa pharyngitis, and occasionally enanthema or erosion on the palate. The tongue is covered with a white coating, often with hypertrophied papillae. Also, signs of the disease may include pain in the joints, pain when urinating, scleral injection, lymphadenopathy, and skin hyperemia.
In 25% of patients, on the 1st-2nd day of illness, a small-spotted, roseolous, maculopapular or urticarial-papular rash appears on the trunk and limbs, which quickly disappears.
In a third of patients, the liver becomes enlarged.
An erased form without intoxication is possible, with minor symptoms of damage to the digestive canal. The duration of the disease is from 4-5 to 14 days, exacerbations and relapses are observed.
The abdominal form, which includes such variants as mesadenitis, terminal ileitis, anendipitis, develops in 10% of patients with yersiniosis. The leading symptom is abdominal pain, constant or transient, initially without a specific localization, which after a few hours - 1-2 days is concentrated in the abdominal or right iliac region. When palpating the abdomen, local pain is detected in the ileocecal (ileococcal) region, often peritoneal signs. Sometimes, with severe mesadenitis, dullness of percussion sound in the right iliac region is determined (positive Padalka's sign). In the case of laparotomy for suspected appendicitis, mesadenitis or terminal ileitis, or appendicitis (catarrhal, less often destructive) is discovered. Often there is a slight serous or serous-hemorrhagic effusion in the abdominal cavity. The abdominal form is usually accompanied by moderate intoxication and gastroenteritis syndrome; in some cases, a rash and minor catarrhal symptoms appear. Terminal ileitis is characterized by inflammation of the distal ileum with mesenteric adenitis, often has a recurrent, protracted, and sometimes complicated course (necrosis of the mucous membrane, ulcerative ileitis, peritonitis, stenosis of the distal ileum, adhesive disease).
Yersinia mesadenitis tends to recur and become chronic. With a favorable course, the abdominal form ends with recovery after 3-6 weeks.
The generalized form of intestinal yersiniosis develops after the localized ones, but a primary generalized form often occurs, caused by highly virulent strains of the pathogen. Characteristic signs are the acute onset of the disease:
- increase in body temperature to 38-40 ° C,
- severe intoxication (headache, dizziness, general weakness, myalgia),
- combination of dyspeptic and catarrhal syndromes,
- rash on the skin and mucous membrane of the mouth and throat,
- arthralgia and arthritis.
In 25% of patients with this form, lymphadenopathy, enlargement of the liver and spleen, and slight jaundice of the sclera and skin are observed; hepatitis develops. The rash (maculopapular, less often small-spotted) most often appears on the 2-3rd day of illness and is localized on the torso, face, limbs, and around large joints. Other types of rash are also possible: roseolous, hemorrhagic, papular, erythematous (ring-shaped, macular, exudative erythema). The rash persists for 1-10 days.
Deafness of heart sounds, lability of pulse and blood pressure are observed. Palpation of the abdomen reveals pain and rumbling. Toxic nephritis may develop. The course of the mixed variant of the generalized form is usually favorable, but a third of patients experience exacerbation and relapses. In a certain proportion of patients, yersiniosis becomes protracted or chronic, as a result of which systemic diseases can develop.
Septic and septicopyemic variants of generalized intestinal yersiniosis develop in patients with severe concomitant diseases and immunodeficiency conditions. The disease begins acutely and is accompanied by:
- high and prolonged fever (from several months to 1 year),
- chills,
- sweating,
- severe intoxication,
- hepatosplenomegaly,
- icteric syndrome,
- recurrent (often hemorrhagic) rash,
- polyarthritis,
- myocarditis,
- pneumonia,
- damage to the central nervous system.
The fulminant form of sepsis is characterized by a rapid course, the development of infectious-toxic shock (ITSH), DIC syndrome.
The secondary focal form can develop against the background or after any of the above clinical forms of intestinal yersiniosis, while the first manifestations of the disease (for example, gastroenteritis) and focal lesions that appear subsequently are characterized by a long-term perspective (from 4-6 weeks to several months).
The arthritic variant of this form is manifested by damage to large and small joints. Tenosynovitis and tendoperiostitis may develop. Arthritis is reactive, bone tissue destruction is usually absent. The course of yersinia arthritis is benign, recovery occurs in 2-4 weeks, less often - 4-6 months, but a longer course is possible (up to 2 years); Residual arthralgias are also observed.
With yersiniosis meningitis, the meningeal symptom complex is combined with some manifestations of yersiniosis (rash, catarrhal and articular syndromes, ileitis, liver enlargement, lymphadenopathy). Erythema nodosum is more often observed in women. The rash looks like painful, 2-4 cm or more in size subcutaneous nodules of a purplish-bluish color, located symmetrically on the limbs, and to a lesser extent on the torso and face. Appears 2-3 weeks after gastrointestinal or abdominal forms of yersiniosis, often occurring subclinically. A nodular rash is accompanied by intoxication and polyarthritis.
Etiology
Yersinia
The causative agent of yersiniosis is the microorganism Yersinia, which belongs to the Enterobacteriaceae family. This motile polymorphic bacterial rod stains negatively for Gram and survives in facultative anaerobic conditions - oxygen-free. Yersinia have peritrichial flagella that provide motility and do not form spores.
The microbe tolerates low temperatures well: it grows and multiplies in food products at 4-6 °C. Thanks to this characteristic of bacteria, yersiniosis is popularly called “refrigerator disease.” The favorite habitats of microbes are confectionery and bakery products, milk and butter. Yersinia actively reproduces in vegetable salads at an ideal temperature of 25 – 29°C.
Yersinia is resistant to environmental factors: it survives freezing and thawing, and retains its pathogenic properties in water and soil for a long time. Direct sunlight, boiling, ultraviolet irradiation, oxidizing agents and chemical disinfectants have a bactericidal effect on Yersinia.
Due to pathogenicity factors, microbes cause the development of pathology. During their life, bacteria release three types of toxins - enterotoxin, cytotoxin and endotoxin. Enterotoxin activates adenylate cyclase of enterocytes, increases the permeability of their membranes to water and electrolytes, causes diarrhea and dehydration.
Yersinia pathogenicity factors:
- A negative Gram stain indicates the presence of a capsule.
- Flagella, which determine the active movement of the microbe after introduction into the human body.
- The ability of the pathogen to adhere and colonize the intestinal mucosa.
- Adhesins causing arthropathy.
- A protease that destroys IgA and facilitates penetration through the mucous membrane of internal organs.
- Outer membrane proteins that ensure unhindered penetration of microbes into deep-lying tissues.
- Cell wall lipopolysaccharides cause the toxicity of Yersinia.
The complex antigenic structure of bacteria explains the unique pathogenesis of the disease, the variety of clinical manifestations, the wide range of severity of toxicosis and the polymorphism of organ lesions.
How to treat yersiniosis?
Treatment of yersiniosis involves complex therapy taking into account the clinical form, severity and period of the disease. Etiotropic therapy at the present stage, according to WHO recommendations, involves the administration of fluoroquinolones to adults, among which preference is given to ciprofloxacin, the course duration of which ranges from 7 days to 1 month, depending on the clinical course.
In the presence of meningitis, pefloxacin is prescribed parenterally, it penetrates the BBB.
For nonseptic yersiniosis, sulfamethoxazole-trimethoprim (trimoxazole) is also recommended for 3-7 days.
In case of a generalized course, it is possible to use 3rd generation pephalosporins, among which preference is given to ceftriaxone, the duration of administration of which depends on the clinical situation. In some cases, gentamicin or doxycycline can be prescribed.
The most important principle of antibiotic therapy for generalized forms is the continuity and duration of the course of antibiotic therapy (up to the 7-10th day of normal body temperature).
In septic forms of the disease, it is advisable to administer 2-3 antibiotics of various groups parenterally.
Pathogenetic therapy includes the use of detoxification, desensitizing, vitamin, metabolic, and antioxidant drugs.
Treatment of patients with a secondary focal form of yersiniosis is complex and is carried out according to an individual scheme. In case of recurrent, protracted course of yersinia polyarthritis, development of Reiter's syndrome, erythema nodosum, glucocorticosteroids are prescribed for a short course.
For articular syndrome, it is advisable to use non-steroidal anti-inflammatory drugs. Immunocorrective therapy is prescribed (after a preliminary examination) against the background of an immunodeficiency state, a protracted course, secondary focal forms without autoimmune disorders.
Diagnostics
Since yersiniosis has various symptoms, similar to other diseases, for differentiation the following diagnostics are carried out:
- general blood analysis;
- blood biochemistry;
- immunological analysis;
- bacterial culture is the most informative method, but this is a rather long analysis. To carry it out, such biomaterial is used as: feces, urine, sputum, washing from the back wall of the pharynx;
- instrumental methods: X-ray, ECG, abdominal ultrasound, CT, laparoscopy.
What diseases can it be associated with?
During its development, yersiniosis provokes many functional disorders:
- terminal ileitis, sometimes appendicitis;
- penetration of Yersinia into regional lymph nodes causes mesadenitis;
- in the appendix, the inflammatory process is often catarrhal in nature with the subsequent development of peritonitis;
- secondary bacteremia with the formation of secondary foci of inflammation leads to the emergence of secondary focal forms (pyelonephritis, arthritis, meningitis, myocarditis, erythema nodosum, etc.);
- if Y. enterocolitica acts as a trigger in the stimulation of immunopathological processes, systemic diseases develop - Reiter's disease, Crohn's, Gunnar-Sjögren's disease, rheumatoid arthritis, autoimmune thyroiditis and hepatitis, endo- and myocarditis, pericarditis;
- The abdominal form of yersiniosis is usually represented by terminal ileitis, the protracted course of which can be complicated by necrosis of the mucous membrane, ulcerative ileitis, peritonitis, stenosis of the distal ileum, and adhesive disease.
In general, complications develop in the case of severe disease, late hospitalization of patients, the presence of chronic diseases and immunodeficiency conditions, and untimely initiation of etiotropic therapy. The most severe complications leading to death in generalized forms are infectious-toxic shock and disseminated intravascular coagulation syndrome. Diffuse ileitis can be complicated by necrosis of the mucous membrane, intestinal perforation and the development of peritonitis, stenosis of the distal ileum, and adhesive disease.
As a result of yersiniosis, the development of chronic forms of ileitis, arthritis, thyroiditis, uveitis, glomerulonephritis, connective tissue diseases, etc. is possible. Septic and septicopyemic variants of generalized yersiniosis are characterized by high mortality - 30-60%.
Epidemiology
Bacteria live in the soil and enter the human body through carriers - various animals: pigs, cats, dogs, cattle, birds, rabbits. Infection from a sick person is possible, but is extremely rare and has no epidemiological significance. Rodents become the source of infection during outbreaks in cities, and clusters of them form the epicenter. Sick rats and mice live in cellars and vegetable stores. Their feces end up on vegetables and in water tanks.
The transmission mechanism is fecal-oral, carried out through the alimentary and waterways.
- Infection occurs when eating food that has undergone inadequate heat treatment: poorly cooked meat, unboiled milk, as well as raw water contaminated with Yersinia.
- There is a contact and household route of transmission of infection among people with poor hygiene standards.
- Cases of yersiniosis after transfusion of infected blood have been described.
Animals become infected by consuming food or water contaminated with soil infected with Yersinia. The contact route of transmission of the pathogen is due to keeping animals in unsanitary conditions.
People have a low susceptibility to yersiniosis. Individuals with a healthy immune system practically do not suffer from clinical forms of infection. Children, elderly people and people with weakened defenses are difficult to tolerate the disease. Bacteria, penetrating the body, attach to the epithelium of the intestinal mucosa and destroy it. Such processes lead to the formation of a detailed clinical picture of the disease. The risk group includes people working in livestock farming, poultry farming and food processing units.
What drugs are used to treat yersiniosis?
- Ciprofloxacin - 0.5 g 2 times a day orally or 0.4 g 2 times a day parenterally for a duration of 7 days to 1 month, depending on the clinical course.
- Pefloxacin - in the presence of meningitis, 0.4 g 2 times a day parenterally.
- Trimoxazole - for nonseptic yersiniosis, 0.8 g of sulfamethoxazole (active ingredient) 2 times a day for 3-7 days.
- Ceftriaxone - for generalized course at a dose of 1.0 g 2 times a day parenterally; The duration of drug administration depends on the clinical situation.
Symptoms
Yersinia parasitizes the upper parts of the large intestine, with an incubation period of about a week.
The disease usually begins with an increase in temperature from 38 to 40 degrees, accompanied by the following symptoms:
- nausea;
- vomiting;
- abdominal pain;
- diarrhea;
- inflammation of the lymph nodes;
- rash;
- puffiness of the face and neck.
This photo shows the presence of a rash on the upper extremities due to yersiniosis
All these are signs of uncomplicated yersiniosis. The initial symptoms may pass quickly enough, but the disease is insidious in that, without manifesting itself for a long time, it affects the internal organs.
Treatment of yersiniosis with traditional methods
Treatment of yersiniosis with folk remedies is perceived by medical professionals with a certain degree of skepticism. It is not recommended to start treatment with folk remedies at the first symptoms of yersiniosis; it is advisable to seek professional help. Therapy for this infection usually requires the use of several strong antibiotics, which cannot be equivalent to herbal medicine. If in the later stages of treatment or during the recovery period the doctor deems it acceptable to use herbal infusions or other herbal medicine, this will be discussed individually.
Classification
Morphological forms of the disease:
Gastrointestinal - inflammation of the stomach and small intestine with the development of gastritis, enteritis or gastroenteritis;- Abdominal - inflammation of the large intestine, appendix, mesenteric lymph nodes;
- Generalized - intoxication, dyspepsia, signs of inflammation of the lungs, meninges, liver, kidneys;
- Mixed - intestinal infection with simultaneous inflammation of several internal organs,
- Secondary focal - occurs as an autoimmune inflammation of the joints, myocardium, intestines against the background of an existing yersinia infection;
- Erased - often not detected; proceeds like a banal intestinal infection; It is tolerated by patients much easier than the manifest forms of the disease.
Yersiniosis can acquire an acute, chronic and recurrent course with periods of attenuation and exacerbation.
Gastrointestinal and abdominal forms develop if the Yersinia strain has a low invasive ability, and the human immune system reliably protects the body from the infectious process. Pathology is formed at the gastrointestinal tract level without further spread of infection.
Highly virulent Yersinia strains are causative agents of a generalized form of infection in individuals with severe immunodeficiency. Microbes enter the blood through the intestinal wall, spread throughout the body and reach internal organs, which become inflamed and cease to function normally. During the treatment process, the immune system defeats the infection and the patient makes a full recovery. If this does not happen, the generalized form becomes secondary focal, proceeding like an autoimmune disease - vasculitis, Crohn's disease, rheumatoid arthritis, thyroiditis.
Treatment of yersiniosis during pregnancy
A complex infectious disease that provokes systemic and multiple organ disorders in the body, which turns out to be yersiniosis, negatively affects the course of pregnancy and requires the use of potent antibacterial drugs for treatment.
As part of prevention, the following is carried out:
- sanitary control of water supply;
- sanitary and hygienic measures at food facilities;
- compliance with the rules of transportation, storage, preparation and sale of products and ready meals;
- protection of food warehouses, vegetable stores from rodents, deratization measures;
- veterinary control of animals;
- sanitary educational work among the population.
No specific vaccination has been developed.
Prevention
To prevent infection with yersiniosis, a number of preventive measures are necessary.
The first and most important thing that is required is the fight against rodents, as they pose the greatest danger. You should also follow all food storage measures to avoid infection.
It is very important to check the sanitary standards for preparing dishes from raw products, as well as checking the quality of water.
If one person becomes ill, disinfection is carried out in any group.
It is very important to maintain personal hygiene and keep the refrigerator and food storage areas clean.
Treatment of other diseases starting with the letter - and
| Treatment of ileus |
| Treatment of impetigo |
| Internet addiction treatment |
| Treatment of interstitial nephritis |
| Treatment of intra-abdominal abscesses |
| Treatment of heart attack |
| Treatment of pulmonary infarction |
| Treatment of splenic infarction |
| Treatment of erythema infectiosum |
| Treatment of hysteria |
| Treatment of ichthyosis |
| Treatment of ischemic stroke |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.
Diagnostic measures
Diagnosis of yersiniosis begins with listening to complaints, collecting anamnesis and external examination of the patient. Specialists collect information about the symptoms and the time of their appearance, the course of the disease and the circumstances under which the infection occurred - contact with sick animals, consumption of raw water and poorly cooked food.
- Laboratory diagnostics consists of conducting a blood test and drawing up an immunogram. The hemogram shows anemia, leukocytosis, lymphopenia, eosinophilia, increased ESR; in the immunogram - antigens and antibodies to the causative agent of yersiniosis.
- The main method for diagnosing yersiniosis is bacteriological. The pathogen is isolated from the feces, blood, bile and liquor of sick people. The laboratory examines sputum or rinsing from the mucous membrane of the throat. The biomaterial taken from the patient is inoculated on special nutrient media on which the infectious agent grows and multiplies freely. First, inoculate in liquid accumulation media and place the tubes in the refrigerator. On the 3rd or 5th day, the culture is reseeded onto Endo and Ploskirev plate selective media, and the dishes are placed in a thermostat. After incubation under special conditions, bacterial colonies are assessed. Then a pure culture is isolated and the microbe is identified to genus and species by sowing in a variegated His row to study its biochemical properties. Final typing is carried out using diagnostic agglutinating sera. Yersinia is also isolated from environmental objects and food products. Bacteriological diagnostics give good and accurate results, but take a lot of time.
- Serodiagnosis allows you to get results in a shorter time. Pathogen antigens are determined in the blood using ELISA, RIF, RAL and RNIF. Serological diagnosis of yersiniosis includes a detailed Widal agglutination reaction with the appropriate diagnosticums and a passive hemagglutination reaction with an antigenic erythrocyte diagnosticum.
- Genetic analysis is the detection of pathogen DNA in the material under study by performing PCR.
- All patients require consultation with specialists in the field of gastroenterology, cardiology, nephrology, and neurology.
- To identify existing complications, an ECG, echocardiography, ultrasound of internal organs, CT, MRI, and radiography are performed.
Features of the pathology
Most people with yersiniosis suffer from children from 2 to 14 years of age. The disease is rare in adults. The causative agent is Yersinia enterocolitica, a bacterium belonging to the Enterobacteriaceae family. It also includes Yersinia pseudotuberculosis, the causative agent of pseudotuberculosis, a pathology with similar manifestations.
Causes of yersiniosis in children - infection with the bacterium Yersinia enterocolitica
The causative agent of yersiniosis is very resistant to low temperatures. It survives even at -20 degrees. Yersinia is not afraid of either the cellar or the refrigerator. However, it dies in boiled water and is easily killed by disinfectants. The bacterium cannot survive in an environment with very low humidity.
In Russia, a surge in Yersinia infections usually occurs during the cold season: late autumn, winter, early spring.
Special risk groups
You can get yersiniosis:
- children suffering from pathologies that weaken the immune system: HIV, cancer, chronic malnutrition caused by pancreatitis, Crohn's disease and other severe chronic diseases of the digestive system;
- Chemotherapy also contributes to the occurrence of yersiniosis;
- in isolated cases, newborn children whose mothers had an acute form of yersiniosis are also infected.
In patients with similar immune problems, intestinal yersiniosis occurs in a more severe form and more often leads to complications.
Difference from pseudotuberculosis
One of the forms of the disease is pseudotuberculosis, also caused by Yersinia, but by another species - Yersinia pseudotuberculosis. The incubation period lasts up to 21 days, while the pathogenesis of the disease is the same.
A typical symptom is the so-called “glove or stocking syndrome.” At the same time, the skin on the palms or soles peels off and comes off in layers. Another typical symptom is the presence of a rash. This rash will appear in the area:
- ankle joints;
- knee;
- wrist;
- elbows.
The disease was called pseudotuberculosis because foci in the form of a capsule with cheesy contents are found in the lymph nodes and parenchymal organs. But unlike tuberculosis, there are no epithelial cells in them.