Currently, the accelerated pace of life, lack of time, constant employment of young and middle-aged people increasingly lead to the fact that a person does not pay due attention to his health, even if something bothers him. However, it should be remembered that many dangerous diseases, causing only slight discomfort at the beginning, can lead to a disastrous outcome as complications develop. This is especially true for abdominal aortic aneurysm.
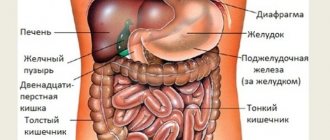
The aorta is the largest and most important vessel in the human body. This artery carries blood from the heart to other organs and is located along the spine in the chest and abdominal cavities. Its diameter in the abdominal cavity ranges from 15 to 32 mm, and it is in this section that an aneurysm most often (in 80% of cases) develops. An aneurysm is a protrusion or bulging of the vessel wall caused by atherosclerotic, inflammatory or traumatic damage.
The following types of abdominal aortic aneurysms are distinguished:
- by localization of the lesion: suprarenal, infrarenal (above and below the place of separation of the renal arteries from the aorta, respectively), total (along its entire length).
- by diameter: small (3 – 5 cm in diameter), medium (5 – 7 cm), large (more than 7 cm), giant (several times larger than the normal diameter of the vessel).
- by nature: uncomplicated and complicated (rupture, dissection, formation of blood clots on the aortic wall).
- Shape: saccular and spindle-shaped. Their differences are that a saccular bulge covers less than half the diameter, if you imagine the aorta in cross section, and a fusiform aneurysm is a bulge of the wall over almost the entire diameter.
- according to the structure of the protrusion wall: true, false and stratifying. A true aneurysm is formed by all the membranes of the vascular wall (inner, middle and outer), while a false aneurysm is represented by scar tissue replacing the normal aortic wall in this area. A dissecting aneurysm is a divergence of the membranes of the vessel wall and the flow of blood between them.
Abdominal aortic aneurysm occurs in 5% of men over 60 years of age. The danger of an aneurysm is that the thinned wall at the site of the protrusion may not withstand the blood pressure and rupture, which will lead to death. The mortality rate for this complication is high and amounts to 75%.
What can lead to an abdominal aortic aneurysm?
Causes of aneurysm formation:
- Atherosclerosis is the most common cause of aneurysm. In 73–90%, protrusion of the wall of the abdominal aorta is caused by the deposition of atherosclerotic plaques with damage to the internal lining of the vessel.
- Inflammatory lesions of the aorta in tuberculosis, syphilis, mycoplasmosis, nonspecific aortoarteritis, bacterial endocarditis, rheumatism.
- Genetic disorders that cause weakness of the vascular wall (connective tissue dysplasia, Marfan syndrome).
- Traumatic injuries to the vascular wall can occur after closed injuries to the abdomen, chest or spine.
- Postoperative false aneurysms from anastomoses can extremely rarely form after operations on the aorta.
- Fungal (mycotic) lesions of the aorta in persons with immunodeficiency (HIV - infection, drug addiction) or due to the entry of a fungal pathogen into the blood (sepsis).
Structure at the microscopic level
The aorta is a complex structure formed by a combination of various tissues and components such as nerves, extracellular matrix, endothelial cells, intimal cells and smooth muscle.
The walls of this “pipeline” consist of 3 layers:
- Inner lining or endothelium , consisting of 1 layer of epithelial cells and in contact with blood. It provides a soft lining surface for blood flow.
- Middle shell. Consists of 5-7 layers of smooth muscle surrounding the lumen of the aorta and elastic tissue. This special composition provides the flexibility of the vessel, which is necessary for its contraction or expansion with each heartbeat. The tissue layer also promotes proper distribution of blood.
- The outer layer or adventitia is the outer layer of the vessel, formed mainly by collagen. The substance is necessary to ensure that the artery remains attached to surrounding tissues and organs.
Risk factors for aortic atherosclerosis and aneurysm formation:
- male gender - men are affected more often than women, although aneurysms also occur in women.
- age over 50 - 60 years - as the body ages, the elasticity of blood vessels is impaired, which makes the aortic wall susceptible to damaging factors.
- complicated heredity - the presence of an aneurysm in close relatives, connective tissue dysplasia, which has a genetic predisposition.
- Smoking negatively affects the cardiovascular system as a whole, since substances contained in cigarettes damage the inner lining of blood vessels and affect blood pressure levels, increasing the risk of developing hypertension.
- Alcohol abuse also has a toxic effect on blood vessels.
- diabetes mellitus - glucose, which cannot be absorbed by cells from the blood, damages the inner lining of blood vessels and the aorta, promoting deposition
- overweight
- arterial hypertension (see drugs to lower blood pressure).
- elevated cholesterol levels
Conditions that provoke aneurysm rupture
- hypertensive crisis
- excessive physical activity
- injury, for example as a result of a road accident
What function does it serve?
The task of the abdominal aorta is to supply blood to the lower abdomen. It delivers oxygen and nutrients along with the blood:
- into the abdominal cavity;
- to your feet.
Thanks to the abdominal aorta, the functioning of:
- genitourinary system;
- digestive system.
This vessel also maintains normal blood pressure due to the elasticity of its walls. When the heart contracts, the walls of the aorta are stretched by a large volume of blood, and when it relaxes, the wall returns to its original position. Due to this mechanism, a large difference between systolic and diastolic blood pressure is prevented.
Systolic pressure evaluates the tension and filling of the arteries with blood at the moment of maximum contractile activity of the heart. Diastolic shows the minimum tension at the moment of myocardial relaxation.
How does an aortic aneurysm manifest in the abdominal cavity?
An uncomplicated small aneurysm may not manifest itself clinically for several years, and is detected by chance during examination for other diseases. Formation of more significant sizes is manifested by the following signs:
- the most common symptom of an aneurysm is dull pain in the abdomen of a pulling, bursting nature
- discomfort and feeling of heaviness in the left umbilical region
- feeling of pulsation in the abdomen
- digestive disorders - nausea, belching, unstable stools, lack of appetite
- lower back pain, numbness and coldness of the lower extremities
If the patient notices these signs, you should consult a doctor for examination, as they may be symptoms of an abdominal aortic aneurysm.
Branches of the large unpaired arterial vessel
The abdominal part of the aorta and all the main arterial branches are very elastic. During systole, the walls of the aorta and arteries dilate to accommodate the increased blood flow. During diastole, adjacent vessels contract, and elastin fibers help move blood through the arterial vessels.
Overview of the branches of the aorta:
| Parts of the aorta | Branches | What organs supply blood |
| Ascending department: coronary arteries | Left | Left atrium, left ventricle |
| Right | Right atrium, right ventricle | |
| Aortic arch | Brachiocephalic trunk | The right half of the head, neck and brain, right arm |
| Carotid artery | Brain, organ of vision, neck | |
| Left subclavian artery | Parts of the neck and chest | |
| Descending | Intercostal | Intercostal space |
| Subcostal arteries | hypochondrium | |
| Superior artery (diaphragm) | Diaphragm | |
| Bronchial | Connective tissue and lymph nodes of the lungs, bronchial mucosa | |
| Esophageal | Esophagus | |
| Pericardial | Posterior part of the pericardium | |
| Mediastinal | Lymph nodes of the posterior mediastinum, connective tissue | |
| Abdominal | Lower diaphragm (pair) | Aperture |
| Celiac trunk | Pancreas, duodenum, spleen and adjacent mesentery, stomach, liver | |
| Superior mesenteric | The small intestine below the duodenum, as well as parts of the cecum and colon | |
| Adrenal | Adrenal glands | |
| Renal | Adrenal glands | |
| Ovarian (female), testicular (male) | Ovary and epididymis | |
| Inferior mesenteric | Distal third of the transverse colon, descending colon, sigmoid colon and upper rectum | |
| Lumbar | Lumbar spine, spinal canal, parts of the lumbar muscles of the back and lateral walls of the trunk | |
| Common iliac | Pelvic area and lower limb | |
| Sacral median (caudal) | Sacral spine |
The supply of blood to each organ or tissue is precisely regulated by the body. The brain receives about 13%, and sometimes more, sometimes less blood is delivered to other organs, depending on how “active” they are. After eating, for example, quite a lot of blood enters the gastrointestinal tract, about 24%. When performing physical work, more blood enters the skeletal muscles than at rest.
Examination for suspected aneurysm
In the absence of symptoms, the diagnosis can be made by chance, for example, during an ultrasound scan for diseases of the stomach, intestines, or kidneys.
If there are clinical signs of an aneurysm, the doctor who suspects this disease examines the patient and prescribes additional research methods. Upon examination, pulsation of the anterior abdominal wall is determined in the supine position; upon auscultation of the abdominal cavity, a systolic murmur is heard in the projection of the aneurysm; upon palpation of the abdomen, a volumetric pulsating formation similar to a tumor is palpated.
The following instrumental methods are prescribed:
- Ultrasound and duplex scanning of the abdominal aorta - allows you to visualize a protrusion in the aortic wall, determine the location and extent of the aneurysm, assess the speed and nature of blood flow in this area, identify atherosclerotic lesions of the wall and the presence of wall thrombi.
- CT or MRI of the abdominal cavity may be prescribed to clarify the location of the formation and assess the spread of the aneurysm to the outgoing arteries.
- Angiography is prescribed in case of unclear diagnosis based on the results of a previous examination. It consists of injecting a radiopaque substance into a peripheral artery and taking an X-ray after the substance enters the aorta.
- X-ray of the abdominal cavity can be informative if calcium salts are deposited in the walls of the aneurysm and their decalcification has occurred. Then the contours and extent of the protrusion can be traced on the x-ray, since the abdominal part of the normal aorta is not normally visible.
In addition, mandatory studies are carried out - a general blood test and biochemical blood tests, a study of cholesterol levels, a blood test for glucose, rheumatological tests, etc.
Parietal or parietal branches
All branches of medicine are divided into two groups. The first includes parietal branches, which have the second name parietal. The second includes visceral or visceral branches. The parietal branches include several arterial pathways:
- inferior phrenic artery. Its beginning is at the level of the twelfth thoracic ridge. Its direction lies towards the lower surface of the diaphragm. This artery is also divided into thin suprarenal arterial tracts, the number of which is from 1 to 24 pieces. Their direction lies downwards towards the adrenal gland;
- lumbar There are 4 pairs of these vessels. It falls on the level of the first to fourth lumbar ridges. The arteries enter the muscle fibers of the posterior wall of the peritoneum, then the path lies forward, they lie between the internal oblique abdominal muscle and the transverse muscle. This ensures blood supply to the abdominal walls. Each lumbar artery branches off into a dorsal branch, which in turn provides branches for the blood supply to the muscle fibers and skin of the back. The branch also goes into the vertebral canal, where it supplies the spinal cord, as well as its membranes and the roots of the spinal nerves, with arterial blood;
- median sacral. It is a very thin arterial vessel that begins its branch at the level of the fifth lumbar ridge from the posterior surface of the aorta. This place falls on the area where the artery divides into the common iliac vessels. Passes to the middle part of the surface of the sacrum to the coccyx. Thus, it supplies the sacrum and coccyx with arterial blood.
Treatment of abdominal aortic aneurysm
There are no medications that can eliminate an aneurysm. But the patient should still take the medications prescribed by the doctor to prevent high blood pressure, which can cause the aneurysm to rupture, and to prevent further damage to the vascular wall. The following groups of drugs are prescribed:
- cardiotropic drugs - Prestarium, Recardium, verapamil, Noliprel, etc.
- anticoagulants and antiplatelet agents (drugs that prevent the formation of blood clots) - cardiomagnyl, thromboAss, aspicor, warfarin, clopidogrel. They should be prescribed with caution, as rupture of the aneurysm contributes to further bleeding.
- lipid-lowering drugs (atorvastatin, rosuvastatin, etc., see statins - harm or benefit) normalize cholesterol levels in the blood, preventing its deposition on the walls of blood vessels (
- antibiotics and antifungals for inflammatory processes in the aorta.
- anti-inflammatory drugs (NSAIDs - diclofenac, corticosteroids - prednisolone) for rheumatic damage to the heart and aorta.
- medications aimed at correcting glucose levels in diabetes mellitus, etc.
Effective treatment of the disease is carried out only by surgery. The operation can be performed on a planned or emergency basis.
The indication for elective surgical intervention is an uncomplicated aneurysm larger than 5 cm. Emergency surgery is performed for aortic dissection or rupture.
In both cases, the operation is performed under general anesthesia with the connection of a heart-lung machine. An incision is made in the anterior abdominal wall with access to the abdominal aorta. After this, the surgeon applies clamps above and below the protrusion, excises the walls of the aneurysm and sutures an artificial prosthesis to the intact areas of the aorta above and below the aneurysm.
The prosthesis is a synthetic tube that takes root well in the body and does not require replacement throughout a person’s life. Sometimes a prosthesis, bifurcated at the end, is used to replace the aorta below the site of its bifurcation in case of damage to the iliac arteries. The operation lasts about 2 – 4 hours.
After suturing the surgical wound, the patient is transferred to the intensive care unit, where he is under observation for up to 5–7 days. After this, another two to three weeks or longer, depending on the course of the postoperative period, remains in the specialized department, and is discharged home under the supervision of a cardiologist and cardiac surgeon at the clinic at the place of residence.
Contraindications for elective surgery
- acute myocardial infarction
- acute stroke (no earlier than 6 weeks after its occurrence)
- chronic heart failure in late stages
- severe liver and kidney failure
- acute infectious diseases
- decompensation of concomitant diseases (diabetes mellitus, bronchial asthma, etc.)
- acute surgical pathology (pancreatitis, appendicitis, cholecystitis, etc.).
Due to the fact that when preparing for a planned intervention, the patient and the doctor have time, unlike a complicated aneurysm, the patient can be carefully examined taking into account possible contraindications and an assessment of the body’s compensatory capabilities.
There are no contraindications for emergency surgery, since the surgical risk is several times less than the mortality rate from complications of the aneurysm, therefore any patient with suspected aneurysm rupture should be taken to the operating table.
In the 90s of the last century, Argentine scientists tested a device for aortic replacement called a stent graft. This is an aortic prosthesis, which consists of a trunk and two legs, guided by a catheter under X-ray television control through the femoral artery to the aneurysm and self-reinforced in the walls of the aorta with special hooks.
- The operation is endovascular and is performed without an incision in the anterior abdominal wall under local or general anesthesia. Duration 1 – 3 hours.
- The advantages of aortic endoprosthetics are low trauma compared to open surgery and faster recovery of the body.
- Disadvantages - due to the fact that the aneurysm itself is not excised, but the prosthesis is inserted as if inside the protrusion, the aneurysm continues to exist. Gradually, the protrusion of the aortic wall spreads above the stent attachment site, which leads to the development of new blood flow paths, the formation of blood clots, dissection of the vessel wall, and, as a result, increases the risk of complications. Often these processes require a conventional operation, therefore, despite good results in the early period after endoprosthetics, it is performed less frequently than open surgery.
The mass distribution of endoprosthetics is limited by the considerable costs of the clinic for the purchase of graft stents (the cost of one prosthesis abroad is about 500 thousand rubles, the cost of the operation itself is 20 - 40 thousand rubles), especially since the stent must be made individually for a specific patient. In Russia, this operation is considered a high-tech type of care, and in some clinics it is carried out according to quotas from the Ministry of Health of the Russian Federation. Open operations, especially in an emergency, are performed free of charge.
Description
An aortic aneurysm is usually called a lumen formed in it that is twice (or more) the normal diameter of the vessels. A defect appears as a result of the destruction of the elastic fibers (filaments) of the central shell, as a result of which the remaining fibrous tissue elongates, thereby expanding the diameter of the vessels and leading to tension in their walls. As the disease progresses and the size of the lumen subsequently increases, there is a possibility of rupture of the aortic aneurysm.
Classification of aortic aneurysm
In surgery, several classifications of aortic aneurysm are considered: depending on the origin, localization of segments, the nature of the clinical course, the structure of the aneurysmal sac and shape.
Based on location, the following types of thoracic aortic aneurysm are distinguished:
- aneurysm of the ascending aorta;
- sinus of Valsalva;
- arc areas;
- descending part;
- abdominal and thoracic regions.
It should be noted that the diameter of the ascending aorta should normally be about 3 cm, and the descending aorta should be 2.5 cm. The abdominal aorta, in turn, should be no more than 2 cm. The dimensions of the aortic aneurysm are considered critical if they exceed normal values by almost 2 times.
Based on the location of the abdominal aortic aneurysm, there are:
- suprarental aneurysms (belong to the upper part of the abdominal aorta with outgoing branches);
- infrarenal aortic aneurysm (without dividing the aorta into common iliac arteries);
- total.
Depending on the origin, the following are considered:
- acquired aneurysms (non-inflammatory, inflammatory, idiopathic);
- congenital.
Classification of aneurysm by shape:
- saccular – presented in the form of a limited bulging of the wall (does not occupy even half of the aortic diameter);
- are divided into iliac, lateral, spreading and descending arteries into the pelvic region;
- fusiform aortic aneurysm - occurs as a result of stretching of the aortic wall along the entire circumference or part of its segment;
The structure of the aneurysm sac differs:
- false aortic aneurysm, or pseudoaneurysm (the wall consists of scar tissue).
- true (the structure of such an aneurysm resembles the structure of the wall itself).
Depending on the clinical course, the following are considered:
- dissecting aortic aneurysm;
- aneurysm is asymptomatic;
- complicated;
- typical.
The term “complicated aneurysm” means rupture of the sac, which, as a rule, is accompanied by heavy internal bleeding and subsequent formation of hematomas. In this situation, thrombosis of the aneurysm, which is characterized by a slowdown or complete cessation of blood flow, cannot be excluded.
One of the most dangerous phenomena is a dissecting arterial aneurysm. In this case, blood passes through the lumen in the inner membrane, which penetrates between the layers of the aortic walls and spreads through the vessels under the influence of pressure. As a result of this process, dissection of the aortic aneurysm occurs.
What you need to know about aortic aneurysms?
As mentioned earlier, all aneurysms are divided into congenital and acquired. The development of the former is characterized by diseases of the aortic walls of a hereditary nature (fibrous dysplasia, Marfan syndrome, Ehlers-Danlos syndrome, congenital elastin deficiencies and Erdheim syndrome).
Acquired aneurysms arise as a result of ongoing inflammatory processes associated with specific (syphilis, tuberculosis) and nonspecific aortitis (streptococcal infection and rheumatic fever), as well as as a result of fungal infections and infections that arise after surgery.
As for non-inflammatory aneurysm, the main reasons for its occurrence are the presence of atherosclerosis, previous prosthetics and defects formed after suturing.
There is also a possibility of mechanical damage to the aorta. In this case, aneurysms of a traumatic nature occur.
You should not ignore the person’s age, the presence of arterial hypertension, alcohol abuse, and smoking. In this case, the likelihood of developing a vascular aneurysm is also high.
Description of abdominal aortic aneurysm
Abdominal aortic aneurysm is most often observed in men over 60 years of age. In particular, the risk of developing the disease increases with regular increases in blood pressure and smoking.
An abdominal aortic aneurysm manifests itself in the form of dull, aching and gradually increasing pain in the abdomen. Unpleasant sensations, as a rule, occur to the left of the navel and radiate to the back, sacrum and lower back. If such symptoms are detected, you should consult a doctor, otherwise the abdominal aortic aneurysm may rupture.
Indirect symptoms include:
- sudden weight loss;
- belching;
- constipation lasting up to 3 days;
- urinary disturbance;
- attacks of renal colic;
- motor disorders in the limbs.
Also, with an abdominal aneurysm, problems with gait may occur due to poor circulation.
Aneurysm of the thoracic aorta. Description of the disease
With an aneurysm of the ascending aorta, patients complain of severe pain in the chest and in the heart. If the lumen has increased significantly, then there is a possibility of compression of the superior vena cava, which may result in swelling in the face, arms, neck, as well as migraine.
An aortic arch aneurysm has slightly different symptoms. The pain is localized in the area of the shoulder blades and behind the sternum. Aneurysm of the thoracic aorta is directly related to compression of nearby organs.
Wherein:
- there is strong pressure on the esophagus, which disrupts the swallowing process and causes bleeding;
- the patient feels shortness of breath;
- there is profuse salivation and bradycardia;
- compression of the recurrent nerve is characterized by a dry cough and the appearance of hoarseness in the voice.
When the cardiac part of the stomach is compressed, pain appears in the duodenum, nausea, profuse vomiting, discomfort in the stomach, and belching.
Aneurysm of the descending aorta is accompanied by severe pain in the chest, shortness of breath, anemia and cough.
Where to go and how to identify the disease?
Aortic aneurysm is diagnosed using several methods. One of the most used is radiography. The procedure is carried out in 3 stages. The main thing when performing radiography is a complete display of the lumen of the esophagus. In the image, the aneurysm of the descending artery protrudes into the left lung.
It should be noted that in most patients a slight displacement of the esophagus is detected. In the rest, calcification is observed - a local accumulation of calcium in the form of salts in the aneurysmal sac.
As for the abdominal aneurysm, in this case, radiography shows the presence of calcification and Schmorl's hernia.
Ultrasound of the aorta of the heart is also important when diagnosing an aneurysm. The study allows us to identify the size of the ascending lumen, descending lumen, as well as the aortic arch and abdominal capillaries. An ultrasound can show the condition of the blood vessels leaving the aorta, as well as changes in the wall area.
A CT scan can also determine the size of the aneurysm that has formed and identify the causes of an abdominal artery aneurysm.
Why is an aneurysm dangerous? What can the doctor recommend?
The likelihood of rupture of an aortic aneurysm with a size of less than 5 cm is minimal. Typically, in this case, the disease is treated with medications that are used to treat high blood pressure. These include beta blockers. Such drugs reduce the force of heart contractions, reduce pain and normalize blood pressure.
Your doctor may also prescribe medications to treat high cholesterol. They have been proven to reduce the risk of death and stroke.
If the aneurysm has reached a size exceeding 5 cm, the doctor will most likely prescribe surgery, since there is a possibility of its rupture and the formation of thrombosis. Surgical intervention consists of removing the aneurysm and further prosthetics of the area where it is located.
Aortic aneurysm. Recommendations
If a doctor discovers an aortic aneurysm, then most likely he will recommend radically changing your usual lifestyle. First, you should give up bad habits, in particular: smoking and drinking alcohol.
Prevention of aortic aneurysm involves eating heart-healthy foods (kiwi, sauerkraut, citrus fruits) and doing physical exercises that will increase your heart rate.
Complications after surgery
- Mortality after planned surgery is 0–0.34% per year in the long-term period.
- Mortality after operated rupture of an aneurysm in the first two months is 90%.
- Operative mortality varies greatly: for elective operations it is 7–10%;
- during operations for aneurysm rupture - 40 - 50%;
- for endoprosthetics – 1%.
The statistics presented and the experience of surgeons show that a planned operation is much preferable for the patient, since delay in the presence of indications for surgery is fraught with a threat to life. But even with careful preparation of the patient and assessment of surgical risks, the development of complications after surgery cannot be ruled out. They develop rarely and account for less than 4%.
Complications in the early postoperative period
- pulmonary edema
- cerebral edema
- renal failure
- dehiscence and inflammation of the surgical wound
- blood clotting disorders and bleeding in internal organs
- in endoprosthetics – endoleaks, or leakage of the installed prosthesis
- thromboembolic complications - separation and entry of blood clots into the arteries of the intestine, lower extremities, brain, and pulmonary artery.
Prevention of complications includes careful selection of a prosthesis, intensive monitoring of the patient in the postoperative period, taking antibiotics, and prescribing heparin according to a standard surgical regimen.
In the long term there are
- prosthesis infection (0.3 – 6%)
- prosthetic intestinal fistula (less than 1%)
- prosthesis thrombosis (3% within 10 years after surgery)
- sexual dysfunction (less than 10% in the first year after surgery)
- postoperative hernia.
Prevention of long-term complications - prescribing antibiotics for any invasive examinations, dental, gynecological and urological procedures, if they are accompanied by penetration into body tissues; lifelong use of statins, antiplatelet agents, beta blockers and ACE inhibitors. Impotence can be prevented by carefully isolating the iliac arteries and aorta at the time of surgery so as not to damage nearby nerves.
Features and norms
Human anatomy is considered a complex but very interesting science. Knowing what each department and organ is responsible for, how our body works, it becomes easier to monitor our health and respond to any changes in a timely manner. We can be affected by many diseases, which only qualified specialists can help us cope with. Often we are faced with diseases of organs and blood vessels directly related to them. One of them is the abdominal aorta (AA). Normally, the cross-section of this artery is 2–3 centimeters in diameter. The length does not exceed 13 cm. The BA is located in the region of the 7th thoracic spine. From there it originates and nourishes the nearby abdominal organs. It ends in the area of the 4th lumbar vertebra, after which it branches into 2 directions.
Each person may have their own characteristics and structure, which is why BA sometimes ends in the area of the 3rd or 5th lumbar vertebra. The structure allows the aorta to be protected from all kinds of damage, since it is located on the inside of the human spine. You can find it a little to the left of the medial line. The top is covered with fiber and lymphatic vessels, which guarantees protection from damage. The aorta, located in a straight line, gradually changes at an early age, acquiring a curved shape.
Next to BA, a person has:
- vein of the left kidney;
- inferior vena cava;
- pancreas;
- splenic vein;
- intermesenteric plexus;
- lumbar sections of the left sympathetic trunks;
- upper roots of the mesentery of the intestine (small).
This aorta is directly involved in the digestive process, since it provides nutrients to most of the organs that are responsible for digestion. In its normal state, it is characterized by a regular cylindrical shape, and when cut, the diameter is 2–3 centimeters. Any expansion, change and deviation from the norm is an impetus for examination and comprehensive diagnosis. Violation of the correct form leads to the development of pathologies. The detection of an altered abdominal aorta indicates the development of potentially dangerous diseases of internal organs and systems. It is necessary to consider the most common diseases caused by disturbances in the structure of the abdominal aorta.
What is the danger of an abdominal aortic aneurysm without surgery?
This disease is fraught with the development of life-threatening complications, such as dissection, rupture or thrombosis of the aorta.
Dissecting aneurysm of the abdominal aorta
It is caused by the gradual thinning of the walls of the aorta and the penetration of blood into the wall of the vessel, stratifying its membranes. This hematoma spreads further and further until the wall bursts under the influence of blood pressure and the aorta ruptures.
- symptoms: sharp pain in the abdomen or back, severe weakness, pallor, decreased blood pressure, cold profuse sweat, loss of consciousness, collapse, shock and death. Sometimes the patient may not even have time to get to the hospital.
- diagnostics: emergency ultrasound of the abdominal cavity, if indicated - CT or MRI.
- Treatment: emergency surgery.
Aortic rupture
There is a breakthrough of blood from the aorta into the abdominal cavity or retroperitoneal space. Symptoms, diagnosis, and treatment are similar to those of dissecting aortic aneurysm. Shock and death are caused by massive blood loss and cardiac dysfunction.
Aneurysm thrombosis
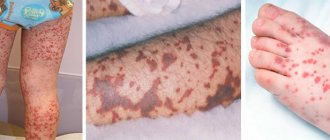
Rarely, complete blockage of the entire lumen by thrombotic masses develops; mainly, the formation of parietal thrombi occurs, which, with the blood flow, can be transferred to smaller arteries and cause blockage of their lumen (renal, iliac arteries, arteries of the lower extremities).
- signs: with renal artery thrombosis - sudden severe pain in the lower back, lack of urination, general poor health, nausea, vomiting; with thrombosis of the iliac and femoral arteries - sudden coldness of the lower extremities (one or both), intense pain, rapid bluish skin of the legs, impaired motor function.
- diagnostics: ultrasound and duplex scanning
- Treatment: anticoagulant therapy, surgical removal of the blood clot.
Diagnostics
Photo: organserdce.com
How to identify an aortic aneurysm if in some cases it develops asymptomatically and is discovered by chance during some examination or autopsy, but is not the cause of death? Some cases have specific signs of aortic aneurysm and lead to all sorts of life-threatening complications. This disease is most often observed in older people. This is caused by age-related pathologies of the vascular walls, the presence of hypertension or metabolic disorders.
There are two types of aneurysm, differing in location in the human body:
- Thoracic aortic aneurysm – located in the thoracic region;
- Abdominal aortic aneurysm is located in the abdominal cavity.
These aneurysms are distinguished by shape, parameters and complications. Signs of an aortic aneurysm determine the course of the disease and the surgical procedure. A complication in the form of internal bleeding in 2 out of 5 cases leads to death.
Establishing diagnosis
Diagnosis of dissecting aortic aneurysm is quite difficult due to several reasons:
- Signs of an aortic aneurysm are not monitored;
- Symptoms correspond to other diseases (for example, cough and discomfort in the thoracic region are observed with pulmonary diseases); Pathology is rarely encountered in medical practice.
If there are signs of the disease, you should consult a therapist or cardiologist. They will conduct an initial examination, based on the results of which examinations are prescribed. After testing, the diagnosis of aortic aneurysm is often confirmed.
How to diagnose an aortic aneurysm?
Diagnosis of dissecting aortic aneurysm is performed using certain instrumental research methods:
- A physical examination serves to collect initial data (complaints) without the use of complex examination methods. Diagnosis of an aortic aneurysm consists of external examination, percussion (tapping), palpation (palpation), auscultation (listening with a stethoscope) and pressure measurement. After detecting characteristic signs, further diagnosis of dissecting aortic aneurysm is prescribed;
- X-ray shows the internal organs of the chest and abdomen. The image clearly shows the protrusion of the aortic arch or its enlargement. To identify the parameters of the aneurysm, a contrast agent is injected into the vessel. Due to the danger and traumatic nature, such diagnosis of dissecting aortic aneurysm is prescribed for special indications;
- Electrocardiography is used to determine the activity of the heart muscle. An ECG of an aortic aneurysm will help distinguish this disease from coronary heart disease. With atherosclerosis, which causes the formation of an aneurysm, the coronary vessels suffer, which can cause a heart attack. How to detect an aortic aneurysm? On the cardiogram, you can track specific signs of an aortic aneurysm corresponding to this pathology of the cardiovascular system;
- Magnetic resonance and computed tomography make it possible to determine all the required parameters of the aneurysm - its location, size, shape and thickness of the vessel walls. The pathognomonic CT sign of a dissecting aortic aneurysm shows wall thickening and a sharp dilation of the lumen of the vessel. Based on these data, possible treatment is determined;
- Ultrasound examination – ultrasound of an abdominal aortic aneurysm is one of the most common diagnostic methods. It helps to determine the speed of blood flow and the existing turbulence that separates the walls of the vessel;
- Laboratory tests include general and biochemical blood tests, as well as urine tests. How to diagnose an aortic aneurysm using tests? They reveal the following signs of an aortic aneurysm: A decrease or increase in the number of leukocytes, characteristic of acute or chronic forms of infectious diseases that precede the formation of an aortic aneurysm. An increase in the number of unsegmented neutrophils is also observed. Increased blood clotting manifests itself in the form of an increase in platelet levels, changes in coagulation factors and indicates the probable formation of blood clots in the aneurysm cavity. High cholesterol levels indicate the presence of atherosclerotic plaques in the vessel. A urine test may show a small amount of blood.
The listed signs of aortic aneurysm are not characteristic symptoms of this disease and are not found in all patients.
What lifestyle should a patient with an abdominal aortic aneurysm lead?
Before surgery. If the aneurysm is small (up to 5 cm), and elective surgery is not planned, doctors take a wait-and-see approach and monitor the patient. The patient should visit the doctor every six months for examination; if the aneurysm grows rapidly (more than 0.5 cm per six months), he will be scheduled for surgery.
After surgery, the patient visits the doctor monthly in the first year, then every six months in the second year and then once a year.
Both before and after surgery, the patient must take medications prescribed by the doctor. It is recommended to follow the following simple steps to maintain a healthy lifestyle to prevent aneurysm growth and complications:
- Proper nutrition and excess weight loss. Fatty, fried, spicy, salty foods are excluded. Animal fats and confectionery products are limited. Fresh vegetables and fruits, cereals, dairy products, low-fat poultry, meat and fish, juices, compotes, fruit drinks are recommended. Eating 4 – 6 times a day, in small portions. It is better to cook products in steamed, boiled, pureed form.
- Reducing cholesterol levels - taking statins as prescribed by a doctor, limiting the intake of cholesterol from food.
- Controlling blood pressure levels - eliminating psycho-emotional stress, heavy physical labor, regularly taking medications that normalize blood pressure, limiting sodium in food.
- Complete cessation of smoking and alcohol. It has been proven that smoking provokes the growth of an aneurysm, and alcohol increases blood pressure, which can provoke a vascular accident.
- Elimination of significant physical activity (in the early postoperative period, complete bed rest with gradual restoration of motor activity). Sports activities are contraindicated. Walking for short distances is acceptable.
- Correction of concomitant diseases - diabetes mellitus, heart disease, liver disease, kidney disease, etc.
Development mechanism, dangers
The development of the pathological process is based on a violation of the anatomical properties of the aortic wall. Normally, it has sufficient elasticity to adapt to dynamic loads. The level of tension is constantly different, depending on blood pressure.
The trigger mechanism for deviation is atherosclerosis or an inflammatory process. Any factors that can lead to degeneration of the vascular wall, its weakening, thinning.
As a result, load resistance decreases. If, in addition, there is an increase in blood pressure, the mechanical effect on the aorta increases.
The result is stretching of the walls at the site of weakening and degeneration. Further, aneurysmal expansion is possible on one side or symmetrical on both sides (spindle-shaped, around the entire circumference).
Then the process continues to grow. The blood flow in the sac-like structure becomes turbulent, and the pressure in the aneurysm increases. Gradually, the formation begins to stratify.
The main consequence and also the danger is a rupture of the structure. The mortality rate of an emergency condition is close to 100%.
There are isolated cases of survival, but this is purely an accident. Death occurs in a matter of seconds due to massive bleeding.
Disease prognosis
The prognosis without treatment is unfavorable, since the natural course of the disease leads to complications and death.
- The mortality rate with small aneurysms (up to 4–5 cm) is less than 5% per year, and with sizes 5–9 cm or more – 75% per year.
- The mortality rate after the discovery of a medium and large aneurysm in the first two years is high and amounts to 50–60%.
- The prognosis after aortic rupture is extremely unfavorable, since 100% of patients without treatment die immediately, and 90% die in the first two months after surgery.
- The prognosis after planned treatment is favorable, 5-year survival after surgery is high 65-70%.
Author:
Selezneva Valentina Anatolyevna physician-therapist
AAA screening
Because many aneurysms do not cause symptoms, a person usually does not see a doctor. Many ABAs are discovered when a doctor diagnoses another condition. To check for the presence of AAA, imaging methods are used:
- Ultrasound
: This procedure uses high-frequency sound waves to measure the size of the abdominal aorta. - CT scan
: In this scan, X-rays create a detailed picture of the AAA. - Angiography
: This test involves X-rays - A CT or MRI scan
with contrast to detect abnormalities in the blood vessels.
Doctors recommend that men ages 65 to 75 who have ever smoked get an ultrasound to check for AAA, even if they don't have any symptoms.
Specialist actions
The condition of the vessel is assessed in grey-scale image mode (B-mode) using color Doppler. This allows you to diagnose disorders - plaques, aneurysms, stenoses, occlusions.
Blood flow is examined using a pulse-wave device. At the level of origin of the visceral branches. The result of measuring hemodynamic velocity in the BA is compared with peak systolic velocities (PSVs). The indicator is calculated at the level of the orifices and visible segments of the celiac trunk, SMA and BA. In practical diagnostics, the survey window is moved from the BA to the ostia and proximal sections of each artery, where PSS is recorded.
Study protocol
Longitudinal section: the aorta is examined in the area from the diaphragm to the bifurcation. Color Doppler imaging is used to detect intimal detachment due to aneurysm, changes associated with stenosis or occlusion. The size and severity of the violation is determined.
Transverse section: the maximum diameter of the aorta is recorded in the area of the diaphragm and at the bifurcation site, the SMA. The anteroposterior and transverse diameters between the outer walls are measured.
Coronal section: The size of the aortic aneurysm between the outer walls is calculated.
Video 1:
How the research is carried out
Diagnosis includes assessment of the condition of the proximal abdominal aorta, orifice and celiac trunk, SMA and IA. Distal areas cannot be visualized.
Before the ultrasound, the doctor does not give any medications. The subject is placed on the couch in a supine position. The specialist installs the device sensor under the xiphoid process. This position allows you to visualize the main artery with the celiac trunk. The doctor takes all necessary measurements.
The patient has to roll over on his side or at an angle. This allows a clear view of the aorta, celiac trunk, and SMA through the liver. To obtain an adequate spectrum during the diagnostic process, the doctor asks the patient to hold his breath.
Doppler examination is necessarily performed with modern ultrasound equipment. A color, energy and pulse-wave device of high sensitivity is used. In most cases, the procedure is performed with low frequency sensors (2–5 MHz). The specialist should focus on the orifice of the celiac trunk, SMA and NBA. These are typical sites for the development of atherosclerotic lesions.
Picture 3:
determining the condition of the main bloodstream
What influences the success of the procedure?
In addition to the quality of the equipment and the professionalism of the specialist who conducts the study, there are several other important factors that can affect the possibility of high-quality visualization.
First of all, this concerns a person’s body weight. Flatulence and shortness of breath may also affect the results. Therefore, it is extremely important to properly prepare for this study.
More fresh and relevant information about health on our Telegram channel. Subscribe: https://t.me/foodandhealthru
We will be grateful if you use the buttons:
Hemodynamics of the aorta
The cardiac cycle affects the average speed of blood flow in the aorta. The velocity rises to a peak during systole but falls during diastole. This pattern is repeated with each cardiac compression. In the area of the ascending aorta and arch, blood flows in a spiral, which reduces blood stagnation and increases oxygen transport.
As blood moves into the descending aorta, the rotation of the flow decreases. In the case of an aneurysm, physiological disturbances occur in the form of high-velocity and spiral flows in places where they are not normally present. Such abnormal high blood flow rate events place greater stress on the vessel wall.
Causes
Development factors are different. The points are similar in one thing: degeneration of the aortic structures and excessive load are observed.
Atherosclerosis of stenotic type
The essence of the pathological process is the narrowing of the lumen of a large vessel. This is usually the result of prolonged smoking, drinking alcohol, or taking drugs.
Also a characteristic deviation in the condition of hypertensive patients, diabetics, and individuals with excessive production of thyroid hormones.
Stenosis is observed on an ongoing basis. Or the narrowing occurs regularly. As a result of such a “swing,” the muscles of the aorta relax and the density of the wall decreases. In the medium term, changes lead to bulging.
Atherosclerosis of occlusive type
Blockage of a vessel with cholesterol plaque. The pathological process is observed in patients with diabetes mellitus, persons with impaired fat metabolism (outwardly manifested by excess body weight), and other people.
Treatment is relatively simple in the early stages. Statins are used to dissolve formations. There is another option, blockage with a blood clot.
If the lumen of the vessel is sufficient for the passage of blood, death does not occur.
Arterial hypertension
Isolated abdominal aortic aneurysm rarely causes. A combination of a group of factors is required, including atherosclerosis.
Excess pressure leads to excessive stress on the walls of the aorta.
With their dystrophy and impaired elasticity, the mechanical factor is sufficient for the development of an aneurysm. No one can say for sure when this will happen.
Aortitis
Inflammatory process. Has a specific character. Develops as a result of tuberculosis, syphilis, and herpetic lesions. It is a complication.
Treatment is urgent, in a hospital setting. The likelihood of developing an aneurysm varies between 10-30%.
Vasculitis
About the same thing, only the lesion is nonspecific. Autoimmune development factors are several times more common. Infections are also possible.
As a result of the pathological process, the elasticity of the walls decreases along the entire diameter, which is why point sac-like aneurysms are less common. There are no guarantees that a deviation will develop, but the risks are high.
Injuries suffered
Especially the abdominal cavity. Unlike the chest, it is covered only by powerful abdominal muscles. However, this is not enough.
Persons who have been involved in a car accident or have survived a fall from a great height are especially often injured.
Aortic ruptures result in instant death. Tissue bruises can lead to the formation of a hematoma, compression of a large vessel and gradual disruption of the cellular structure.
Postponed surgeries
Regarding a pre-existing aneurysm, anomalies of anatomical development. The probability of such an outcome is small, but it exists.
Therefore, after surgery, regular screening for late complications (developing over 12 months or more) is recommended.
Abdominal tumors
Including surrounding organs and systems. They cause compression of the aorta, disruption of the vessel, and a possible increase in pressure in the affected area.
Preparation for the procedure
Content:
- Indications
- Preparation for the procedure
- How does duplex scanning work?
- Advantages and disadvantages
- What does this procedure reveal?
- Criteria for damage to the branches of the aorta
- What influences the success of the procedure?
Duplex examination must be performed on an empty stomach, so you should refrain from eating 4-6 hours before the procedure. No other special preparatory rules are required, except in cases of increased gas formation in the patient. With flatulence, it is almost impossible to see the organs on the monitor, so the person may be sent for bowel cleansing. Before the procedure itself and before prescribing it, the attending doctor must tell the patient about all the nuances of the procedure. During this conversation, a person can ask any questions that concern him.
Forecast
Presented with many options. The overall mortality rate of abdominal aortic aneurysm is 30-40%. Without surgery the number is higher. After radical treatment, it is twice or three times lower.
The outcome depends on many factors:
- Age. Young patients tolerate surgical therapy more easily. Therefore, the chances of a favorable outcome are greater.
- Presence of somatic pathologies. Hypertension, diabetes mellitus, and cardiac problems create the risk of postoperative complications. Including, not every surgeon will take on such a person due to the high threat of death.
- Family history. If there are patients with an aneurysm in your family, the risks increase. You need to look at the outcome of the family member. Because the peculiarities of the circulatory system and metabolic phenomena are also transmitted.
- The degree of progression of the pathology. If persistent negative dynamics are observed, the formation grows every six months, surgery cannot be avoided.
- Localization of the violation. If there is damage at the level of the renal arteries, the mortality rate, even with timely treatment, is several times higher. Such cases are not trivial, so it makes sense to look for surgeons in the capital or abroad.
After treatment, survival rate is 85%. Other situations are more difficult.