A general blood test showed “leukocytes - 10 thousand in 1 μl of blood”, what should I do? This condition in which the number of leukocytes in the blood exceeds the established 9.0 thousand in one microliter of blood is called leukocytosis.
Normally, 1 μl of human blood contains from 4 to 9 thousand leukocytes, depending on gender and age category. Leukocytosis or increased white blood cells in the blood is a relative concept; for example, for plasma donors, stricter limits of leukocytes are established, beyond which the donor is not allowed.
General information
Leukocytes - what are they?
The answer to the question “what are leukocytes?” is not as clear as it seems at first glance. To put it simply, leukocytes are white blood cells that are involved in protecting the body from bacteria, viruses and other harmful agents. This concept also includes a heterogeneous group of blood cells of different morphology and significance, united by the presence of a nucleus and the absence of color.
What are leukocytes responsible for?
The main function of white blood cells is specific and nonspecific protection against all types of pathogenic agents and participation in the implementation of certain pathological processes, that is, they are responsible for the “protection” of the body.
Blood structure
All types of leukocytes can actively move and penetrate through the capillary wall into the intercellular space, where they capture and digest foreign agents. If a lot of such agents penetrate the tissue, then the leukocytes, absorbing them, greatly increase and are destroyed. This releases substances that provoke the development of a local inflammatory reaction, which is manifested by swelling, increased temperature and hyperemia of the inflamed focus.
Where are leukocytes formed in humans and how long do they live?
Carrying out the function of protecting the body, a large number of leukocytes die. To maintain a constant quantity, they are continuously produced in the spleen, bone marrow, lymph nodes and tonsils. Leukocytes usually live up to 12 days.
Where are leukocytes destroyed?
Substances that are released when white blood cells are destroyed attract other leukocytes to the area where foreign agents are introduced. By destroying the latter, as well as damaged cells of the body, white blood cells die en masse. The pus that is present in inflamed tissues is an accumulation of destroyed white blood cells.
What are white blood cells also called?
There are 3 main synonyms for the described cells in the literature: white blood cells, white blood cells and leukocytes. They are classically divided into granulocytes and agranulocytes . The former include eosinophils , neutrophils and basophils , the latter – lymphocytes and monocytes .
Classification and characteristics of white blood cells
Approximately half a century ago, the lower limit of normal leukocytes fluctuated between 5.5-6.0 G/l; currently this level has dropped to 4.0 G/l, or even less . This is due to widespread urbanization, increased radioactive background, and the use of a large number of medications, sometimes unjustified. However, leukocytosis has not disappeared anywhere and, under certain circumstances, makes itself felt as a symptom of some disease, since it is not an independent nosological unit.
The following types of leukocytosis are distinguished:
- Physiological ( redistribution
or, as they used to call it,
relative
), due to the redistribution of an increased number of white blood cells between the vessels of various organs; - Pathological
(
reactive
or
absolute
), associated with a violation of leukopoiesis in the pathology of the hematopoietic organs or arising as a response of the body to infectious, purulent-inflammatory, septic and allergic processes.
The classification of leukocytes and leukocytosis is based on the types of white blood cells, their functions and behavior. White blood cells, depending on the presence or absence of specific granules in the cytoplasm, are divided into two series: granulocytic
and
agranulocytic
.
What kind of cells are these - leukocytes? Why do they behave this way and why do they care? What do the terms “ neutrophilic and eosinophilic leukocytosis”
” that doctors often mention? Why is leukocytosis dangerous or is it not dangerous at all?
And you can understand this if you know the basic properties of leukocytes.
Basic properties of leukocytes, their tasks and functions
The size of leukocytes, depending on the type, ranges from 7.5 to 20 microns; they contain many enzymes (peptidases, lipases, diastases, proteases), which in a quiet state are isolated (in lysosomes) and are called lysosomal enzymes. Leukocytes perform their functions outside the vessels, and they use the vascular bed only as a road. They are characterized by an amoeboid movement, with the help of which they penetrate the endothelium of the capillaries ( diapedesis
) and are directed to the lesion (
positive chemotaxis
).
The reverse movement of leukocytes from the source of irritation is called negative chemotaxis
.
If we talk about the norm of leukocytes, then the range of variation here is quite wide (4.0-9.0 G/l) , moreover, blood taken from a finger contains information about only a sixth of white cells, because their main habitat is fabrics. And in order to understand where the norm is and where the pathology is, of course, you need to know what the population of leukocytes is, what tasks it performs, what they are needed for and whether you should worry at all if suddenly a high content of white cells is detected in a general blood test.
The lifespan of leukocytes depends on the type and ranges from several days to 20 years or more. Those leukocytes that have turned into “memory cells” are destined to live long, since even after a long period of time they are obliged to recognize the “foreign” that they met many years ago. Having “remembered” it, they must immediately “inform interested” species. They, in turn, must “give the command” to destroy the stranger.
The main tasks of white blood cells can be represented as follows:
- Leukocytes take part in the formation of cellular and humoral immunity, which constitutes their protective
function; - They enter the gastrointestinal tract, capture nutrients and transport them into the blood, which is especially important for newborns who, while breastfed, receive ready-made, unchanged maternal immunoglobulins along with milk, which can protect a small person from many infections. That is why a child under one year old is not afraid of, for example, the flu. Nature has thought of everything, endowing leukocytes with a metabolic
function; - They dissolve (lyse - lysis) damaged tissues and carry out the histolytic
task; - They destroy various bookmarks that are not needed at all, even in the embryonic period - a morphogenetic
function.
A detailed blood test involves counting not only the total number of leukocytes, but also the percentage of all types of white blood cells in the smear. By the way, the percentage must be converted into absolute values ( leukocyte profile
), then the information content of the analysis will increase significantly.
Granulocyte series
The progenitors of leukocytes (myeloblasts), belonging to the granulocytic series, originate in the bone marrow, where they pass through several stages and do not enter the bloodstream until the end of maturation. In the peripheral blood, under some pathological conditions (or purely by chance - 1 cell), metamyelocytes can be found. These are young (juvenile) cells, they are also the precursors of granulocytes. However, if for some reason young ones appear in the blood, and at the same time they can not only be seen, but counted in a smear, then we can judge a shift to the left
(for leukemia, infectious and inflammatory diseases).
An increase in the stroke of older forms indicates a shift of the formula to the right
.
formation of blood cells from stem cells in the bone marrow
Cells of the granulocyte series are endowed with pronounced enzymatic and metabolic functions, therefore their characteristic neutrophilic, eosinophilic and basophilic granularity is closely related to the activity of the cell and is strictly specific
, i.e., cannot transform from one type to another.
Representatives of granulocytes
Mature granulocytes include:
I. Neutrophils
Neutrophils
represent the largest group of white cells and make up 50-70% of the entire population. The granules located in their cytoplasm have high bactericidal activity (myeloperoxidase, lysozyme, cationic proteins, collagenase, lactoferrin, etc.). In addition, neutrophils have receptors for immunoglobulins (IgG), cytokines and complement proteins. Only 1% of these cells are normally found in the blood, the rest are concentrated in tissues.
Neutrophils are the first to rush to foci of inflammation, phagocytose (capture) and destroy harmful agents; they are the body's main defenders from microbes and toxins. With various infections, their number can increase 5-10 times (neutrophilic leukocytosis), and then not only mature, but also young cells, up to myelocytes, begin to enter the peripheral blood. In such cases, they speak of a leukocyte formula with a shift to the left.
II. Eosinophils
Eosinophils
make up 1-5% of all leukocytes. They got their name because they lend themselves well to staining with eosin dye. They remain in the bloodstream for several hours, and then are sent to the tissues, where they are destroyed. Eosinophils perform phagocytic and detoxification functions (neutralize toxins), destroy foreign proteins, neutralize antigen-antibody reaction products by capturing histamine and other substances, produce histaminase, participate in the formation of plasminogen, that is, they are a part of fibrinolysis. In addition to the listed advantages, eosinophils contain:
- Antiparasitic alkaline protein;
- Prostaglandins;
- Leukotrienes;
- Histaminase;
- Inhibitors of mast cell and basophil degranulation;
- They have receptors for IgE, IgG, IgM.
Given such a wide composition of leukocytes of this type, eosinophilic leukocytosis is a significant diagnostic indicator for helminthic infestations and allergic reactions, when the number of eosinophils increases, and an encouraging sign for ARVI and some other infections. Elevated levels of eosinophils in such cases indicate impending recovery.
III. Basophils
Basophils are literally rare in a smear, only 0-1%. Their task is to produce histamine, which dilates capillary vessels and promotes wound healing, and heparin, which is a natural anticoagulant (anti-clotting system of the blood). They, along with mast cells, are also called heparinocytes. Basophils contain platelet activating factor (PAF), prostaglandins, and leukotrienes. They are equipped with IgE receptors, which play an important role in the release of histamine and the manifestation of allergic reactions (urticaria, anaphylactic shock, bronchial asthma).
Granulocytes are also interesting because they replenish energy reserves through anaerobic glycolysis and thrive in oxygen-poor tissues, which is why they rush to areas of inflammation that are poorly supplied with blood. The neutrophils themselves, when they die, release lysosomal enzymes, which soften the tissue and form a purulent focus (abscess), so the pus consists of destroyed neutrophils and their fragments.
Non-granular agranulocytes
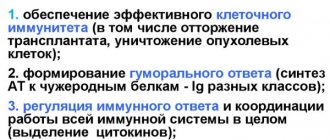
The importance and significance of agranulocytes in all immunological reactions can hardly be overestimated, since they play a leading role in ensuring cellular and humoral immunity. Certain types of leukocytes-agranulocytes are designed to perform the following tasks:
Monocytes
Monocytes
make up 2-10% of the entire leukocyte community (macrophages).
They arrive at the scene of the incident (damage zone) immediately behind the neutrophils, have powerful bactericidal properties (especially in an acidic environment), phagocytize microorganisms, destroyed leukocytes and dead tissue cells, freeing the inflammation zone, for which they are called “ the body’s wipers
”;
Lymphocytes
Lymphocytes - (20-40% of all Le) cells that have left the blood vessel, following their specialization, do not return back. In addition, they live for a long time - tens of years, especially “memory cells”.
Lymphocytes
– are the central link of the immune system (immunocompetent cells), they take care of maintaining the constancy of the internal environment of the body and are able to recognize “theirs” and “theirs”. In addition, the activity of lymphocytes is not limited to these tasks:
- They synthesize antibodies ( B lymphocytes
); - Lyse foreign cells. This function belongs to natural killers (N-killers), which are called zero, since they do not belong to either the B or T lymphocyte
communities; - Provide immunological reactions “graft versus host” and “host versus graft”;
- Destroy their own mutant cells;
- They bring the body into a state of sensitization when foreign proteins enter.
Lymphocytes are formed from a common stem cell. Some are sent to the thymus gland (thymus), where they undergo “training” and become T-lymphocytes of various “professions”:
- T-helpers or assistants (they know everything and give commands);
- T-suppressors (suppress the immunological reaction when it is no longer needed);
- T-killers (they themselves kill at the level of cellular immunity);
- T-amplifiers (effectors, accelerators of immune processes);
- Immunological memory cells that carry information about past diseases (why many people get an infection once in their life).
B cell differentiation occurs in the red bone marrow and lymphoid organs. Their main function is active antibody formation and providing all stages of humoral immunity.
Only a small portion of lymphocytes circulate in the peripheral blood; the rest constantly migrate through the lymph nodes, spleen and bone marrow.
Norm of leukocytes in the blood
How many leukocytes should a healthy person have?
The normal number of white blood cells in the blood is measured in units (that is, cells) per liter of blood. It is also worth understanding that the content of leukocytes is not constant, but changes depending on the state of the body and the time of day. For example, the concentration of leukocytes usually increases slightly after meals, in the evening, after physical and mental stress.
The normal level of leukocytes in the blood of an adult over 16 years of age is 4-9·109/l. Considering the amount of blood in the adult human body, we can say that there are from 20 to 45 billion white blood cells circulating there.
What is the norm of leukocytes in the blood of men?
The above value is taken as the normal level of leukocytes in men (more precisely, leukocytes 4.4-10). In the body of males, the number of leukocytes is subject to much weaker fluctuations than in other groups of patients.
What is the normal number of leukocytes in women?
In women, this indicator is more variable and leukocytes of 3.3-10·109/l are taken as the standard. The figures for this indicator may fluctuate depending on the phase of the menstrual cycle and the state of hormonal levels.
Normal white blood cell count in pregnant women
It is known that many blood parameters in pregnant women are altered, therefore, values that are overestimated for ordinary patients are considered to be the norm for leukocytes. Thus, according to various authors, an increase in the number of leukocytes to 12-15·109/l should not cause concern and is physiological for this condition.
The norm of leukocytes in the blood of a child
The norm of the indicator described in this section in children directly depends on age.
| Age | Normal value (unit 109/l) |
| 11 – 16 years | 4,5 — 13 |
| 6 – 10 years | 4,5 — 13,5 |
| 4 – 6 years | 5 — 14,5 |
| 34 years | 5,5 — 15,5 |
| 6 – 24 months | 6,6 — 11,2 |
| 1-6 months | 7,7 — 12 |
| 8-14 days | 8,5 — 14 |
| 1-7 days | 9 — 15 |
| newborns | 10 — 30 |
Leukocyte formula
The blood test also calculates the percentage of different types of leukocytes. Absolute cell values are additionally designated by the abbreviation “abs.”
Classification of leukocytes by groups
In a healthy person, the leukocyte formula looks like this:
- band neutrophils – 1-6%;
- segmented neutrophils – 47-72%;
- eosinophils – 0.5-5%;
- basophils – 0.1%;
- lymphocytes – 20-37%;
- monocytes – 3-11%.
In children, during the development process, 2 so-called “crossovers” of the leukocyte formula occur:
- the first at the age of 5 days, when the lymphocyte/neutrophil goes from 20%/60% to 60%/20%;
- the second at the age of 4-5 years, when the reverse crossover occurs to the lymphocyte/neutrophil of 20%/60%, after which the content and proportions of this ratio should correspond to those of an adult.
Leukocytosis - what is it?
“What is leukocytosis” and “leukocytosis - what is it?” are the most frequent queries on hematology topics on the World Wide Web. So, leukocytosis is a condition characterized by an increase in the absolute number of leukocytes per liter of blood more than an established physiological indicator. It should be understood that an increase in leukocytes in the blood is a relative phenomenon. When interpreting a general blood test, one should take into account gender, age, living conditions, diet and many other indicators. In adult patients, a leukocyte count exceeding 9·109/l is considered leukocytosis.
Elevated leukocytes in the blood - what does this mean?
In simple terms, leukocytosis indicates the presence of an inflammatory process in the body. The reasons why leukocytes in the blood are elevated are physiological and pathological in nature, respectively, and leukocytosis is physiological and pathological.
Physiological (which means that does not require treatment) increased levels of leukocytes in the blood can occur for the following reasons:
- hard physical labor;
- food intake (can “spoil” a blood test, causing an increased number of leukocytes after a meal to reach 12·109/l);
- dietary characteristics (food leukocytosis can also occur if the diet is dominated by meat products, some components of which the body perceives as foreign antibodies - this means that leukocytes in the blood will be increased due to the development of an immune response);
- pregnancy and childbirth;
- taking cold and hot baths;
- after vaccination;
- premenstrual period.
An increased level of leukocytes in the blood of a pathological nature requires examination or, at a minimum, re-analysis after 3-5 days to exclude counting errors. If leukocytes in the blood are elevated and physiological causes have been excluded, then an increase in the number indicates the presence of one or more of the following conditions:
- infectious disorders ( meningitis , sepsis , pneumonia , pyelonephritis and others);
- infectious disorders affecting immune cells (infectious lymphocytosis or mononucleosis );
- various inflammatory diseases caused by microorganisms ( phlegmon , peritonitis , abscess , boil , appendicitis , infected wounds - these are the most common causes of an increase in the described indicator in the blood);
- inflammatory disorders of non-infectious origin ( systemic lupus erythematosus , rheumatoid arthritis and others);
- myocardial infarction , lung and other organs;
- extensive burns;
- malignant neoplasms (in the presence metastases in the bone marrow, leukopenia );
- large blood loss;
- proliferative diseases of hematopoiesis (for example, leukemia , when white blood cells are increased to 100·109/l or more);
- splenectomy;
- diabetic coma, uremia.
In addition, when there are a lot of leukocytes in the blood, this means that in rare cases one can suspect poisoning with aniline or nitrobenzene . Many leukocytes in the blood appear in the initial stage of radiation sickness .
There are a number of insufficiently studied conditions of the human body, in which leukocytes and ESR and body temperature rises slightly. After a short period of time, these indicators return to normal. These abnormal conditions do not have any noticeable manifestations.
Causes of elevated leukocytes in the blood of women
In women, as stated earlier, there are many more physiological reasons for the level of leukocytes to be higher than normal. What does it mean? The fact is that hematological parameters in women are much more dynamic and subject to change. Most often, a physiological increase in the indicator is observed during the premenstrual period and during pregnancy, but after childbirth it decreases to normal values. Otherwise, the causes of leukocytosis in women are identical to those described above.
Elevated white blood cells during pregnancy
The norm during pregnancy for the described indicator is, according to various authors, up to 15 and even 18·109/l. Leukocytosis during pregnancy is a fairly common phenomenon, reflecting the reaction of the mother's immune system to the presence of the fetus. If white blood cells are elevated during pregnancy, the patient's condition should be closely monitored due to the increased risk of premature birth. Also, we should not forget about the “traditional” causes of leukocytosis: inflammation, infections, somatic diseases. White blood cells that are elevated after childbirth usually return to normal within 2-4 weeks.
High white blood cells in a child
In general, in pediatrics it is believed that if a blood test shows leukocytes 14·109/l in a healthy patient, then you should be wary, order a repeat test and draw up an examination plan. The reasons for elevated leukocytes in a child’s blood can be varied, so patients in this category always need to have a repeat test.
The most common reason why a child’s white blood cell count is elevated is the presence of childhood infections (including elementary ARI , when blood counts are changed within a few days after recovery), mainly of a bacterial nature.
They are also high in children with other diseases (which are more common in children than in adults), for example, leukemia (colloquially “blood cancer”) and juvenile rheumatoid arthritis . The reasons for the described phenomenon in a newborn are described below.
High white blood cells in a newborn
If leukocytes are elevated in a newborn, this is not always a sign of disease (as, for example, increased bilirubin ). Their normal level in the blood immediately after birth can reach 30·109/l. However, it should decrease quickly during the first week. The issues of increasing leukocytes in a newborn (infant) should be dealt with by an experienced neonatologist.
Symptoms of leukocytosis
Leukocytosis in children and adults, leukocytosis in newborns and pregnant women never causes characteristic signs of changes in well-being and cannot be detected during instrumental examination. Moderate leukocytosis in itself is a symptom and without collecting an anamnesis, examination by specialists, or ordering tests, it does not have any special clinical significance.
How to lower and how to raise leukocytes in the blood
Patients are often interested in how to quickly lower or how to quickly increase leukocytes in the blood. At the same time, on the Internet you can find a lot of useless and sometimes dangerous methods for raising or lowering the level of leukocytes using folk remedies.
It is important to understand: an elevated or increased level of leukocytes does not require urgent reduction to normal; a comprehensive, thorough examination of the patient and a search for the cause of this phenomenon are needed. And when the cause is eliminated (cured), the leukocyte count will return to normal.
Diagnostics
Leukocytosis is detected during a clinical blood test. Since there are many reasons for an increase in white blood cell levels, you should first consult a general practitioner. The doctor collects a detailed medical history, conducts a physical examination of the patient, including measuring body temperature, examining the skin and mucous membranes, etc. Based on the data obtained, in order to confirm the disease that caused leukocytosis, the following studies are prescribed:
- Blood tests
. Markers of inflammation are determined in the blood - high ESR and CRP, autoantibodies (rheumatoid factor, ACCP, antibodies to the cytoplasm of neutrophils). The leukocyte formula (percentage of leukocyte forms) must be calculated. A blood smear is examined for the presence of toxic granularity of neutrophils, atypical mononuclear cells, and Botkin-Gumprecht shadows. If a septic condition is suspected, presepsin is measured. - Pathogen detection
. To identify the infectious pathogen as the cause of leukocytosis, bacterial culture of blood, sputum, and urine is performed. The enzyme immunoassay method detects antibodies (class and immunoglobulins) to bacteria, viruses, helminths, and their DNA is detected using the polymerase chain reaction. - Allergy diagnostics
. In order to confirm the allergic nature of the disease, the level of immunoglobulin E (IgE) is measured using the ELISA method. To identify the causative allergen, basophil tests and various allergological tests are performed - skin (scarification, patch, prick tests), provocative (nasal, inhalation, conjunctival). - Radiography
. In case of pneumonia, chest x-rays show infiltrates in the lungs, foci of darkening; x-rays of joints in patients with arthritis show narrowing of the joint space, osteoporosis, and bone erosion. With osteomyelitis, x-rays of bones reveal thickening of the periosteum and sequestration foci (areas of bone necrosis). - Ultrasound
. With pyelonephritis, an ultrasound examination of the kidney reveals an increase in the size of the kidneys, expansion and thickening of the pyelocaliceal system. Infectious mononucleosis is characterized by hepatosplenomegaly. Echocardiography may show vegetations on the valves and effusion into the pericardial cavity. - Histological studies
. If leukemia is suspected, a trephine biopsy or sternal puncture is performed, the material of which reveals hyperplasia of the granulocytic lineage and a large number of blast cells. To diagnose lymphomas, an aspiration biopsy of an enlarged lymph node is performed; the biopsy specimen reveals lymphocytic hypercellularity, collagen proliferation, and Berezovsky-Sternberg giant cells.
The leukocyte formula allows you to determine the percentage of different types of leukocytes
Low leukocytes in the blood - what does this mean?
If there are few leukocytes in the blood, this means that there has been a decrease in the number of white blood cells below 4000 per 1 mm3 (including both granulocytes and agranulocytes ), called leukopenia .
Indicator of the number of leukocytes in the blood
It doesn’t matter whether white blood cells are low in women or men, the reasons for this phenomenon do not differ by gender. So, the following possible reasons for the low level of this indicator:
- damage to bone marrow cells by a variety of chemicals , including drugs;
- hypoplasia or bone marrow aplasia ;
- lack of certain vitamins and microelements ( iron , folic acid , vitamin B12 and B1 copper );
- radiation exposure and radiation sickness ;
- acute leukemia;
- myelofibrosis;
- hypersplenism;
- plasmacytoma;
- myelodysplastic syndromes;
- pernicious anemia;
- metastases to the bone marrow;
- typhus and paratyphoid fever ;
- sepsis;
- carriage of herpes virus types 7 and 6 ;
- anaphylactic shock;
- collagenoses;
- taking medications ( sulfonamides , a number of antibiotics , thyreostatics , NSAIDs , cytostatics , antiepileptic and oral antispasmodic drugs ).
Also, when leukocytes are below normal, this means that the patient should exclude thyroid disease.
If white blood cells are low in a child's blood, this may be a symptom of influenza , malaria , typhoid fever, measles , brucellosis , rubella or viral hepatitis . In any case, leukopenia is a serious phenomenon that requires urgent analysis of its causes.
Elevated leukocytes in a smear in women, causes
Leukocytes normally in a smear from the urethra do not exceed 10 units in the field of view, from the cervix - do not exceed 30 units, from the vagina - do not exceed 15 units.
An increased content of leukocytes in a smear may indicate bacterial infections ( gonorrhea , mycoplasmosis , syphilis , genital tuberculosis chlamydia and others), trichomoniasis , HIV , herpes , papillomavirus , cytomegalovirus , candidiasis , dysbacteriosis , allergies , genital irritation and basic non-compliance hygiene rules before collecting material.
Leukocytes in urine are increased, reasons
The normal content of leukocytes in the urine of men is 5-7 units per field of view, in women - 7-10 units per field of view. leukocyturia in medicine . Its cause can be both failure to comply with personal hygiene rules and serious illnesses (inflammatory diseases of the genitourinary tract, urolithiasis , tuberculosis , carbuncle , systemic lupus erythematosus and others).
Neutrophils are increased
Neutrophils
The normal number of neutrophils in a blood test is:
- for rods 1-6% (or 50-300·106/l in absolute values);
- for segmented ones 47-72% (or 2000-5500·106/l in absolute values).
Neutrophilia - what is it?
A condition in which there is an increase in the number of neutrophils in the blood is called neutrophilia . It can occur during inflammatory purulent processes, infectious acute diseases, insect bites, myocardial infarction , after severe blood loss, and with physiological leukocytosis .
Neutrophils are elevated in adults and children
In general, the reasons for the development of the described condition are similar in people of all ages. It is also known that pronounced neutrophilia is characteristic, as a rule, of bacterial infection . So, if elevated neutrophils in the blood, this means that:
- elevated band neutrophils in an adult or child indicate mild infection or inflammation;
- band neutrophilia with the detection of metamyelocytes against the background of general leukocytosis is observed in purulent-septic complications ;
- neutrophilia with the detection of young leukocytes (promyelocytes, myelocytes, myeloblasts) and the absence of eosinophils indicates a severe course of purulent-septic and infectious diseases and can worsen the patient’s prognosis;
- the causes of increased band neutrophils with the appearance of a large number of destroyed segmented forms indicates suppression of bone marrow activity caused by severe infectious disorders, endogenous intoxication or other reasons;
- the appearance of hypersegmented neutrophils can be caused not only by radiation sickness or pernicious anemia , but in rare cases it is observed in practically healthy patients;
- an increase in segmented forms against the background of eosinophilia (neutrophilic surge) is characteristic of chronic inflammatory processes, myeloproliferative diseases and acute infections.
Increased neutrophils in the blood during pregnancy
The condition when neutrophils are abs. moderately increased, that is, up to 10,000·106/l in a pregnant woman can be interpreted (subject to the exclusion of pathological conditions) as a variant of the norm, called neutrophilia of pregnant women . It occurs due to the response of the immune system to the process of fetal growth and is characterized by an increased content of band granulocytes . In case of neutrophilia in pregnant women, it is necessary to monitor and regularly do a general blood test, since these changes can also signal the risk of premature birth.
Other reasons
- Massive tissue breakdown
: myocardial infarction, ischemic stroke, pancreatic necrosis, extensive burns. - Toxic effects on the bone marrow
: poisoning with lead, organic hydrocarbon compounds, ionizing radiation. - Endocrine disorders
: chronic adrenal insufficiency, autoimmune polyglandular syndromes, congenital dysfunction of the adrenal cortex. - Primary immunodeficiencies
: Wiskott-Aldrich syndrome, Jobe syndrome (hyper-IgE syndrome). - Malignant neoplasms
: small cell lung cancer, breast cancer, colon adenocarcinoma. - Lung diseases
: pulmonary eosinophilia (eosinophilic pneumonia), Langerhans cell histiocytosis, allergic bronchopulmonary aspergillosis. - Dermatological diseases
: eczema, Dühring's dermatitis herpetiformis, scabies. - Condition after removal of the spleen (splenectomy)
: as a component of post-splenectomy syndrome.
Neutrophils are reduced
Neutropenia is a condition when neutrophils in the blood are reduced to 1500·106/l or less. Occurs more often with viral infections. Neutropenia is usually associated with roseola , hepatitis , mumps , adenovirus infection , rubella , influenza viruses , Epstein-Barr , Coxsackie , infection with rickettsia and fungi . The described condition also occurs with radiation sickness , treatment with cytostatics , aplastic and B12-deficiency anemia , and agranulocytosis .
Basophils are increased
The normal number of basophils in a blood test is 0.1% (0-65·106/l in absolute values). These cells take an active part in the allergy and the development of the inflammation process, neutralize poisons from insect bites and other animals, and regulate blood clotting.
Basophils are higher than normal - what does this mean?
Basophilia is an increase in the number of basophils above normal. The reasons for the increase in basophils in an adult and the reasons for the increase in basophils in a child have no fundamental differences and differ only in the frequency of occurrence in different age groups of patients.
So, an increase in the number of basophils occurs in the following diseases:
- blood diseases ( polycythemia vera, chronic myeloid leukemia, acute leukemia, lymphogranulomatosis );
- ulcerative colitis , chronic inflammatory diseases of the digestive tract;
- chronic sinusitis;
- myxedema;
- hemolytic anemia;
- allergic reactions;
- Hodgkin's disease;
- taking antithyroid drugs, estrogens .
Symptoms
Most often, at the initial stage, the disease is not accompanied by specific symptoms and is diagnosed after a blood test.
The main symptoms of leukocytosis are the following:
- weakness of the body;
- increased fatigue;
- general malaise;
- acute periodic headaches;
- increased sweating;
- tingling sensation in the limbs and stomach;
- increased liver size;
- spleen extending beyond the edge;
- enlarged lymph nodes;
- sudden fainting;
- bleeding in the mucous membranes;
- difficulty breathing;
- streaks of blood in various parts of the body;
- increased body temperature;
- lack of weight;
- lack of appetite;
- visual impairment, etc.
As is known, leukocytosis is not an isolated disease. As a rule, such a pathology is considered a signal of the presence of serious diseases of the body (most often blood diseases).
Monocytosis
Monocytosis is a condition when an adult or child has an increased number of monocytes . Elevated monocytes in an adult (the norm is 90-600·106/l or 3-11% in the leukocyte formula ) or a child can be detected with the following pathologies:
- sarcoidosis , brucellosis , syphilis , tuberculosis , ulcerative colitis ;
- infections and the recovery period after acute infections;
- acute leukemia of the monocytic and myelomonocytic type, multiple myeloma, myeloproliferative diseases, lymphogranulomatosis;
- endocarditis , rheumatoid arthritis , systemic lupus erythematosus , periarteritis nodosa ;
- intoxication with tetrachloroethane or phosphorus .
Neutrophilia, eosinophilia, basophilia and other types of leukocytosis, the causes that cause them
- Physiological. It has been proven that after physical activity, the level of white blood cells can increase sharply. In addition, the jump can also be caused by the intake of food, certain liquids and medications (this is more of an autoimmune reaction).
- Pathological-symptomatic leukocytosis is a characteristic feature of some infectious diseases.
- Leukocytosis can also be “short-term”, as a result of stress. It is episodic in nature, appears suddenly and disappears just as quickly. Sometimes, a similar phenomenon accompanies typhus, scarlet fever, diphtheria and some other diseases. This group can be combined with the previous one, but since leukocytosis is short-term, it was decided to separate it into a separate type.
- Neutrophilic surge. Accompanies myeloproliferative diseases, chronic inflammation and acute infections. The number of white blood cells increases sharply due to an increase in the level of neutrophils.
- Increased levels of eosinophils in the blood. Eosinophilia clearly occurs during allergic reactions of various etiologies and malaria.
- Basophilic leukocytosis – accompanies myxedema, ulcerative colitis and pregnancy.
- An increase in the number of leukocytes occurs in all viral infections (ARVI, influenza, herpetic infection, chickenpox, rubella, infectious mononucleosis, etc.) and some severe bacterial ones - brucellosis, syphilis and tuberculosis.
- And finally, a large number of monocytes indicates that a person suffers from a cancerous tumor and a narrow number of bacterial infections.
Changes in blood eosinophil levels
These cells play an important role in the development and suppression of allergic reactions : from elementary nasal congestion ( allergic rhinitis ) to anaphylactic shock . An increase in the number of eosinophils in a blood test is called eosinophilia , and a decrease in their number is called eosinopenia.
Level of eosinophils in the blood
Eosinophilia occurs in a fairly extensive list of diseases, including:
- allergies and bronchial asthma ;
- tumors;
- infestation with parasites;
- lymphogranulomatosis;
- chronic myeloid leukemia;
- scarlet fever;
- treatment with antibiotics , sulfonamides or PAS .
In the vast majority of cases, a decrease in the number of eosinophils below the normal level is associated with increased adrenocorticoid activity, leading to retention of eosinophils in bone marrow tissue. The presence of eosinopenia in the postoperative period indicates how severe the patient's status is.
Allergy
This is the main cause of eosinophilic leukocytosis. Entry of an allergen into the body causes IgE-mediated degranulation of mast cells with the release of mediators of allergic inflammation - leukotrienes, histamine, etc. One of the main functions of eosinophils is to suppress the production of inflammatory mediators, therefore any allergic reaction is accompanied by an increase in the level of eosinophils.
The maximum level of eosinophilia is achieved at the time of exacerbation of the allergic reaction, then it gradually decreases as symptoms regress and returns to normal levels during the remission stage. In most allergic diseases (bronchial asthma, rhinoconjunctivitis), moderate leukocytosis is observed. Only with the development of systemic reactions (Stevens-Jones syndrome, DRESS syndrome) can high leukocytosis occur.
Changes in the level of lymphocytes in the blood
An increase in the content of lymphocytes (lymphocytosis) is observed when:
- bronchial asthma;
- chronic radiation sickness;
- whooping cough, tuberculosis;
- thyrotoxicosis;
- drug addiction;
- after splenectomy ;
- chronic lymphocytic leukemia.
Lymphopenia is observed in the following cases:
- malformations of the organs of the lymphoid system;
- slowing down lymphopoiesis ;
- acceleration of lymphocyte ;
- agammaglobulinemia;
- thymoma;
- leukemia;
- aplastic anemia;
- carcinoma , lymphosarcoma ;
- Cushing's disease;
- systemic lupus erythematosus;
- treatment with corticosteroids;
- AIDS;
- tuberculosis and other diseases.