We study leukocytes in the blood, the norm is given by age and gender. Leukocytes is a collective term that unites different in size and functional activity cells in the body of humans and animals. Common characteristic features are the presence of a nucleus and the white color of the cells (white bodies). In inflammatory diseases, the number of blood leukocytes increases sharply, since they are the first line of defense of the human body against pathogens. This fact explains the need to measure their level at the first stage of diagnosing any disease.
The role of leukocytes in the blood
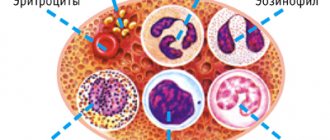
White blood cells have an important mission for the human body - they protect it from viral and bacterial attacks, waste and toxins, and other foreign bodies. The leukocyte series consists of several types, each of which plays its own role:
- Neutrophils - detect bacterial infections and destroy them.
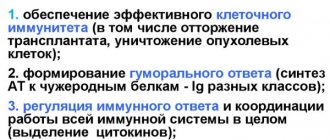
- Lymphocytes are responsible for the immune system and the so-called immune memory.
- Monocytes - destroy foreign elements found in the blood.
- Eosinophils are responsible for human allergic reactions.
- Basophils - play a supporting role in detecting foreign particles and are important in inflammatory and allergic reactions.
The main tasks of leukocytes include:
- Penetration into the gastrointestinal tract in order to capture nutrients and transport them into the blood. This is especially important for infants, who receive immune protection from their mother through breast milk.
- Taking part in building humoral and cellular immunity, i.e. performing a protective function.
- Dissolution of damaged tissues.
If leukocytes in an adult are low, then what does this mean?
An increase in the number of white cells indicates the active work of the immune system aimed at fighting the infectious agent. In turn, the state of leukopenia, which is characterized by a decrease in leukocytes in the blood, indicates the development of a serious pathological process. Possible reasons include:
- lack of necessary substances for normal growth and development of new cells. This condition can be corrected by preparing the right diet;
- destruction of white blood cells is observed during the natural death of leukocytes after the process of phagocytosis;
- insufficient production of leukocytes - as a result of bone marrow dysfunction. This condition is observed in leukemia, chemotherapy, severe poisoning, bone metastasis and autoimmune diseases.
Important: a simultaneous decrease in leukocytes and erythrocytes, as well as the presence of blast cells (precursors of blood cells) in the bloodstream, recorded during a three-fold repeat analysis, is a sufficient reason for a large-scale screening examination for oncology.
Read further: What blood test indicators show oncology (cancer)
Standard indicators: general information
The normal white blood cell count may vary from person to person. Moreover, the main criterion for difference is the age of the subject. So, in children this figure will be higher than in adults. Due to the fact that the norm is estimated in units per liter of blood, diet, body condition and time of day should also be taken into account. So, in the afternoon, after eating, after any stress, physical or mental, the concentration of the indicator will be increased. Gender has virtually no effect on the number of leukocytes. The amendment needs to be made only for a pregnant woman and a woman after 50 years, when due to hormonal changes the concentration of the indicator changes.
For a healthy person, the leukocyte composition of the blood looks like this:
- 55% – neutrophils: 45-72% – segmented neutrophils, 1-6% – band neutrophils;
- 19-37% – lymphocytes;
- 3-11% – monocytes;
- 0.5-5.0% – eosinophils;
- 0.5-1% – basophils.
In a blood test, these data are taken into account in relation to the content of the total number of immune cells.
On the Internet you can find a variety of white blood cell standards that differ greatly from each other. In reality, everything is much simpler - the range from 4 to 9 * 109 is accepted as the norm, with slight adjustments for gender, pregnancy, and age. Children have their own norms, this is due to the passage of a long period of growth and development from newborns to puberty.
Victoria Druzhikina
Neurologist, Therapist
Diagnostics
When conducting a general blood test, the total number of white cells is calculated, cells are counted under a microscope, or the leukocyte formula is compiled using flow cytometry. In this case, the exact quantitative content of each type of white body is determined. This is the first step in establishing the cause of the inflammatory process.
The analysis period does not exceed 1 day.
Additional tests for deviations from the norm include:
- advanced laboratory diagnostics (biochemistry, tests for tumor markers, hormones)
- and laboratory research methods (MRI, ultrasound).
Preparing for a blood test
The preanalytical stage is of maximum importance for the reliability and accuracy of the results obtained. Thus, about 70% of errors are made at this stage. It is extremely important not only to carry out the blood collection procedure correctly, but also for the patient himself to prepare for the test. Recommendations for preparation:
- 6 hours in advance, food intake is excluded; 1 day in advance, fatty, smoked and salty foods are removed from the diet;
- no smoking for 30 minutes;
- It is prohibited to drink alcoholic beverages at least 1 day before the test;
- within 1 hour emotional and physical stress is limited.
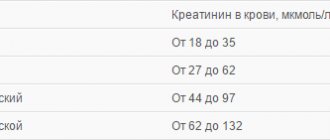
Norm indicators in the table by age for women
The range of standards is indicated in reference books and regulations used by doctors.
For a woman, the normal concentration of white blood cells is 4.0 - 9.0 * 109/l. In this case, the age table will look like this:
Table of normal levels of leukocytes in the blood of women.
| Age | White blood cell count (*109) |
| up to 16 years old | 4,5 — 12,5 |
| up to 20 years | 4,2 — 10,5 |
| from 21 years old | 4 — 9.0 |
The leukocyte norm in women can vary depending on the menstrual phase and hormonal levels. The norm of leukocytes in women after 50 years is somewhat different. This is due to hormonal fluctuations.
Thus, during menopause, the concentration of the indicator increases, replacing the production of certain hormones. After menopause, on the contrary, there is a decline in the activity of a number of hormones and cells, which include white blood cells. In digital terms it will look like this:
- 45-55 years – norm 3.3 – 8.8 units. by 109 cells per liter;
- 55-65 years – norm 3.1 – 7.58 *109/l.
Factors that increase the number of leukocytes
If you have low white blood cell counts, the first thing to do is see your doctor to identify the underlying causes
this condition.
You may also try the additional strategies listed below if you and your doctor determine that they may be appropriate. But neither of these strategies should ever be done in place of what your doctor recommends or prescribes!
Consult your doctor
A low white blood cell count often indicates an underlying health problem that needs to be identified, and your doctor is the best resource for determining appropriate diagnosis and treatment strategies. You and your doctor can discuss medications, dietary supplements, or alternative treatments such as acupuncture or sauna bathing, depending on what is causing the decrease in white blood cells.
Additionally, if you think your immune system is not effective enough, take extra precautions with your hygiene. Make sure you wash your hands and avoid contact with people who may be sick.
Physical training
During and after physical exercise, especially in strength training for men, white blood cell counts increase. This means that the number of cells can increase greatly in response to intense physical training. ()
In the recovery phase after submaximal physical activity, an increase in the number of leukocytes, neutrophils, lymphocytes and monocytes was observed. ()
Be careful with exercise, especially if you have been diagnosed with a low white blood cell count caused by an underlying medical condition. Your doctor can help you determine whether your body can handle this type of stress (exercise).
Healthy eating
A healthy diet rich in fruits and vegetables can help balance your immune system and maintain optimal health. Fruits and vegetables contain vitamins, minerals and polyphenols important for the body.
Certain foods and nutrients can increase white blood cell counts. This was found in animal studies.
- Vitamin B12 helps increase white blood cell counts, but this effect was only observed in protein-deficient rats. Those rats that received normal levels of protein showed unchanged levels of these immune cells. ()
- Garlic – slightly increased the number of leukocytes in rats. ()
- Noni juice increased the number of leukocytes and platelets in the blood of rats. ()
- Fish oil – increased the level of leukocytes in broiler chickens. ()
Taking folic acid
Folate (folic acid) deficiency is associated with a decrease in the number of lymphocytes and granulocytes, two types of white blood cells. ()
In a randomized clinical trial, folic acid supplementation increased white blood cell counts in children receiving the anti-epizootic drug carbamazepine. ()
Taking Shark Liver Oil
Shark liver oil has a lot of alkylglycerols, which are fats that stimulate the production of white blood cells. Supplementation with shark liver oil has been shown in studies to increase the number of these immune cells in humans. ()
Normal for pregnant women
Pregnant women experience changes according to many studies. During the period of bearing a child, the concentration of leukocyte cells up to 12-15*109/l is considered the norm. By trimester it will look like this:
| Trimester | White blood cell count (*109) |
| first | 4 — 9 |
| second | 4 — 10 |
| third | 14 — 12 |
High values are due to increased protective functions of the body, thickening of the blood during pregnancy, and a decrease in the level of lymphocytes. Also during pregnancy you need to know your TSH level.
Also, an increased level of white blood cells is necessary to stimulate uterine contractions.
It is worth noting that each private laboratory has its own standards, slightly different from those prescribed in the document. This is due to the equipment used. Therefore, when donating blood privately, you should pay attention to the standards indicated on the form.
Preparing for a blood test
In order to reliably determine how many leukocytes are in your blood, you must follow the following recommendations:
- Take the test no earlier than 3 hours after eating;
- For 3 hours, avoid drinking caffeine and sugar-containing drinks, alcohol and tobacco;
- Limit physical activity 30-40 minutes before donating blood;
- Before going to the hospital, do not take hot baths, contrast showers or other water procedures at an uncomfortable temperature for the body.
If these rules are not followed, the level of white cells may slightly exceed the norm or be at its upper limit. This change may lead to diagnostic errors and incorrect assessment of health status.
Normal for men
The leukocyte count in men is subject to less fluctuations than in women. The norm for men by age is presented in the table:
| Man's age | White blood cell count (*109) |
| 12-18 years old | 3,5 — 8 |
| 18-25 years old | 4 — 9 |
| 25-40 years | 4 — 8 |
| Over 40 years old | 3 — 9 |
Factors that reduce the number of leukocytes
Work with your doctor to identify and treat any health conditions by increasing your white blood cell levels.
You may try the additional strategies listed below if you and your doctor determine that they may be appropriate. None of these actions should ever be taken instead of your doctor's advice!
Reducing stress
Psychological stress can increase cortisol, adrenaline and prolactin levels, leading to an increase in white blood cell counts. Reducing stress can lower these hormones and help normalize high immune cell counts. (, )
Improving sleep quality
Interrupted, short, and poor-quality sleep can increase inflammation, including white blood cell counts. Make sure you get enough sleep and fall asleep around the same time every night. Normalizing your sleep can help keep inflammation low. (, )
Quit smoking
The white blood cell count in male smokers was significantly higher than in former smokers and non-smokers. In smokers, white blood cell values were associated with the number of cigarettes smoked, the amount of smoke inhaled, and the duration of smoking. ()
Obviously, smoking is not recommended as a means to increase white blood cell counts. If you smoke, we recommend talking to your doctor about ways to quit smoking.
Reduce the amount of carbohydrates in food
A high carbohydrate diet can increase leptin, insulin and IGF-1 levels to a greater extent than fat intake. The high-carbohydrate “Western diet” was also associated with increased white blood cell counts and increased levels of inflammation. Reducing carbohydrates in your diet can help lower white blood cells, reduce inflammation, and possibly help prevent insulin resistance. (, , , )
Reduce caloric intake
Long-term calorie restriction was associated with lower white blood cell counts without harmful effects on the immune system. In a 2-year study of 218 healthy, calorie-restricted adults, those on calorie restriction also showed a 0.6*10/9 L reduction in white blood cell counts. The effect of caloric restriction on people with initially elevated white blood cells is unknown. ()
Normal in children
Children tend to have higher white blood cell counts. The norm for different ages is presented in the table:
| Age | White blood cell count (*109) |
| newborn | 10 — 30 |
| from the fifth day of life | 9 — 15 |
| from the tenth day of life to one month | 8,5 — 14 |
| from month to year | 8 — 12 |
| from one to five years | 7 — 11 |
| from 5 to 15 years | 6 — 10 |
| over 15 years old | 5 — 9 |
The table shows that the norm of leukocyte content in newborn children is very different, for example, from the norm in children 5 years old.
Leukocytes: cognitive and conceptual meaning
Deciphering the results of any medical tests is the immediate task of doctors. Despite this, some basic principles, such as what leukocytes are in a blood test, are of interest to many patients who are responsible for their health. This fact is not surprising based on the importance of blood cells for the body, which will be discussed further in the article. Understanding what these are - leukocytes, which appear on the blood test form under the WBC stamp, often falls on subjects whose indicators deviate from the standards, however, general information about these cells will be useful for healthy people.
Human blood is the main biological fluid of the body, in constant motion, consisting structurally of plasma, or a fluid substrate, and compacted elements, one of which are leukocytes. Leukocytes are the components on which the formation of human immunity is based, and the cells are divided into several subtypes that differ in configuration, size and functionality. The scientific unification of subspecies into one group was based on the morphological characteristics of the cells, consisting in the presence of a nucleus and the absence of color pigmentation, which is characteristic only of leukocytes.
Elevated leukocytes in the blood: causes and treatment
The condition in which white blood cells are elevated is called leukocytosis. It can occur in anyone. Short-term leukocytosis should not cause concern, because it may be associated with the influence of external factors. Thus, a newborn may react with an increased level of leukocytes to new complementary foods. For a man or woman, the norm is a slight increase in the concentration of the indicator as a result of the following situations:
- emotional tension and stress (treated by a psychologist);
- smoking (all the consequences of smoking are described here);
- consumption of certain foods;
- excessive physical activity;
- long stay in the sun or in the bath;
- change of time zones.
To eliminate errors in the analysis, it must be taken in the morning on an empty stomach in a calm state. If, when following all the canons of taking the test, the result still turns out to be above the norm, then we can talk about leukocytosis associated with the presence of some kind of disease.
The reasons why leukocyte cells are elevated may be:
- Any infectious processes.
- Autoimmune pathologies.
- Chronic inflammatory processes.
- Allergies (learn effective allergy remedies from this article).
- Viral infection of the body.
- Severe pain syndrome.
- Oncological processes (examination and therapy are prescribed by an oncologist).
- Burns and frostbite.
- Parasitic contamination of the body.
Causes of increased leukocytes in the blood of women
Women are more likely to have inconsistent test results than men. In addition to the above, the reasons for this may be:
- emotional and mental state;
- changes in climate and weather conditions;
- phase of the menstrual cycle (read what to do with menstrual pain here);
- medications taken;
- inflammatory processes associated with the gynecological area (therapy is prescribed by a gynecologist).
A number of processes occurring in the body of a pregnant woman determine the reasons for the increase in leukocytes in this category of people. In addition to the fact that white blood cells during pregnancy can be elevated due to physiological factors, experts separately identify the following sources:
Doctor's advice
To obtain reliable results, it is important to take a correct blood test. In emergency cases, you can do this after eating; in a planned manner, it is better to go to the treatment room on an empty stomach. It is advisable not to smoke for 2 hours before donating blood. A prerequisite is that if the test is prescribed not to assess the condition during an illness (cold, acute respiratory viral infection, sore throat, etc.), but during a medical examination, then you need to donate blood no less than 2 weeks after recovery in the case of a recent illness. If you perform a blood test a few days after illness, you may find elevated white blood cells that have not yet returned to normal due to the immune response. on the pathogen. Such results will require a second blood donation. Therefore, it is better to wait until 2 weeks have passed and then get examined.
Victoria Druzhikina Neurologist, Therapist
- allergic and inflammatory processes (treated by an allergist) associated with decreased immunity;
- taking medications to maintain pregnancy;
- worsening of chronic pathologies;
- pain in the lumbar region;
- anxiety associated with worries about the child’s development;
- hormonal imbalance (corrected by an endocrinologist), leading to blood thickening.
If a pregnant woman has an increased concentration of leukocyte cells, she will definitely be scheduled for a repeat examination to exclude pathology.
Why leukocytes may be elevated in men: reasons
In men, white blood cells can also be elevated for physiological and pathological reasons. In the first case, there is nothing to worry about: you just need to make sure that the test is taken in compliance with all the standards for passing it. Also, it is necessary to exclude the presence of a man in conditions with high air humidity and temperature immediately before the test. Pathological factors include any deviations in the functioning of the body associated with the occurrence of inflammatory, infectious or bacterial processes. This is due to the fact that it is the man’s immune system that is the first to respond to changes in the steadfastness of the internal environment of his body.
Elevated leukocytes in a child’s blood – what does this mean?
For a child, especially a small one, a condition such as constant mood swings, crying, anxiety, and fear is typical. Also, many parents misinterpret the conditions under which the child is kept. So, a comfortable air temperature for him should be in the range of 18-23 degrees. Adults are used to warmer temperatures. The same applies to baths: often a child is bathed in water that is too hot for him, despite the fact that it is comfortable for an adult. It is overheating and an unstable emotional state that are often the reason why a child’s leukocytes are elevated. Also, the reason for the discrepancy between the indicator and the norm in a child can be vaccination. If the concentration of leukocyte cells is increased significantly even after repeated analysis, then we should talk about pathological phenomena that require research and treatment.
What are leukocytes?
This term refers not to one specific cell, but to about a dozen different microscopic formations. Why were they called in one word? Only because of their similar functions. Each of them ensures the proper functioning of the immune system, being activated when exposed to various harmful factors and the development of inflammation. For a better understanding, leukocytes can be divided into 4 large groups:
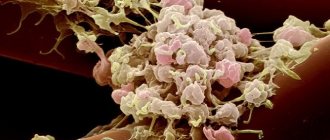
leukocytes under an electron microscope
- Eosinophils . They perform two main functions - they participate in the development of allergies and pathological reactions that occur during the penetration of parasites (Giardia, Ascaris, Opisthorchid, Cysticercus and other organisms). Despite their unpleasant task, these cells are a necessary part of the body's defenses. They are the ones who can “give away” a hidden disease, causing specific symptoms;
- Basophils . The main culprits of any allergic reactions are due to the content of histamine, an amino compound that activates inflammation. When a certain substance (dust particles, animal dander, plant pollen, etc.) penetrates into a susceptible organism, basophils release histamine. The result is the appearance of allergy symptoms (runny nose, dermatitis, anaphylaxis, edema and others);
- Neutrophils (segmented and band-nuclear) . When a harmful bacteria enters the body, these cells will be the first to try to destroy it and prevent the onset of disease. If they fail, neutrophils contain the infection until the body produces specific antibodies against microbes and destroys them. This component of immunity can also be detected in any place where inflammation is actively developing, even if there are no bacteria there. This situation can occur with a heart attack, burn, toxin poisoning and tissue necrosis;
- Lymphocytes . These are the most complex cells, which are the last to take part in protecting the body - on average, after 2 weeks from the penetration of a harmful agent. This time is necessary for lymphocytes to determine the exact type of threat and produce antibodies that act only on a specific harmful factor. Another important function of cells is to provide antitumor immunity, the effectiveness of which is quite low.
Additionally, doctors identify monocytes as a special component of the immune system. However, changes in their number are not very informative and are recorded extremely rarely.
Normally, a blood test for white blood cells should show a certain amount of each of these types of cells. An increase or decrease in their content, in most cases, indicates the presence of a disease or an incorrect diagnostic procedure.
Low leukocytes: causes, treatment
If leukocytes are elevated, this is not always bad. Thus, the body reports some kind of failure and activates protective resources to combat it. A low level of leukocyte cells (leukopenia) is of greater concern. If white blood cells are low, this means that the body cannot fight pathogenic elements. Those. We are talking about the presence of some kind of disease. There are three main factors known for which leukocyte bodies are not produced in the required quantities:
- Lack of necessary substances to build new cells.
- The production of white blood cells with their simultaneous death when fighting foci of infections.
- Imbalance of bone marrow functions.
Leukopenia can be found in both men and women.
The main sign of a prolonged deviation from standard values is an infectious disease, which is manifested by fever and chills and is a consequence of intoxication that is not restrained by leukocytes.
The main factor in combating a low level of leukocyte cells is to prevent the development of infectious diseases, which consists of:
- a well-chosen diet;
- wearing a respiratory mask;
- excluding all contacts with already sick people;
- See a doctor at the slightest increase in temperature;
- treatment with folk remedies.
In severe cases of the disease, drug therapy is carried out. Often the patient is hospitalized to restore immunity.
Substances and ways to reduce the number of leukocytes
There are natural substances and pathways that normally regulate the white blood cells in your body. Talk to your doctor about the most appropriate strategies for treating your medical conditions and managing your white blood cell count.
None of these strategies should be used to replace your doctor's advice!
Zinc
Zinc plays an important role in the body's immune function. Zinc deficiency increased the number of total leukocytes, monocytes and granulocytes (neutrophils, eosinophils and basophils) in mice without changing the number of lymphocytes. ()
Zinc deficiency induces a general stress response, which can lead to an increase in the number of white blood cells. () So, supplementing with zinc (if you don't have enough) can help reduce a high white blood cell count.
Selenium
White blood cell counts decreased in men who ate a diet high in selenium. This decrease may have been caused by changes in the number of granulocytes. ()
The information on this site has not been evaluated by any medical organization. We do not seek to diagnose or treat any disease. The information on the site is provided for educational purposes only. You should consult your physician before acting on information from this site, especially if you are pregnant, nursing, taking medications, or have any medical condition.
Rate this article
Average 4.6 Total votes (10)
Treatment of leukocytosis
Leukocytosis is usually detected only by blood tests. A person does not feel any obvious symptoms indicating a change in the blood. Thus, he may complain of a number of ailments, which are often not associated in any way with a deviation from standard values in the concentration of white blood cells:
- general malaise and fatigue;
- loss of appetite, dizziness (other possible causes of dizziness in women are described here), excessive sweating;
- joint and muscle pain;
- sleep disorder (treated by a somnologist), weakened vision (therapy carried out by an ophthalmologist).
In order to reduce the value of an indicator, the increase of which is associated with physiological reasons, it is recommended:
- avoid hypothermia and overheating;
- Healthy food;
- observe a rest regime;
- be less nervous.
Those. therapy is associated with the elimination of factors causing an increase in the indicator.
If a diagnosis of “leukocytosis” is established, self-medication should not be done under any circumstances. The doctor himself, based on repeated tests and additional examinations, will determine the etymology of the growth of leukocyte cells and prescribe the appropriate treatment.
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1.https://medline.ru/public/art/tom18/art6.html 2. Uncle G.I. et al. Universal reference book for a practicing physician (Section “General blood test”) // Voronezh: Scientific book. - 2021. - 512 p. 3. Kishkun A. A. Clinical laboratory diagnostics. Textbook (Chapter 2. Hematological studies) // M.: GEOTAR-Media. — 2015. — 976 p.
4. Standards for indicators of the composition of blood cells and other indicators are reflected in the ORDER of the Ministry of Health of the Russian Federation dated 09/14/2001 364 (as amended on 06/06/2008), Appendix 3 “NORMS FOR THE COMPOSITION AND BIOCHEMICAL INDICATORS OF PERIPHERAL BLOOD”
Rate how useful it was article
4.8 22 people voted, average rating 4.8
Did you like the article? Save it to your wall so you don’t lose it!
Examination at MedArt
If you want to get a 100% reliable result of a general (clinical) blood test, you will always be welcome at the MedArt diagnostic center. Our specialists are highly qualified and fully competent in the work entrusted to them. High-precision modern medical equipment, high-quality reagents, necessary consumables - we guarantee each of our clients service at the highest level.
With us, you can take a general blood test in a calm and comfortable environment, without distorting the results of your tests due to stress and emotional tension obtained in a long line. You can get accurate and reliable results in just one business day.
What is recommended for patients who have developed this complication?
1) If your body temperature rises, immediately take a blood test. Inform your doctor about the results of the test.
If there is a critically low level of leukocytes and neutrophils, the next administration of chemotherapy will be postponed until complete recovery.
2) Try to stick to a complete diet, exclude raw foods (that is, meat, fish, eggs, fruits and vegetables) - all foods, without exception, must be thermally processed.
3) Follow a work and rest schedule, do not overload yourself, give your body the opportunity to replenish its strength and energy for a speedy recovery.
4) Maintain personal hygiene carefully, because any infection can cause the condition to worsen.
5) Do not visit crowded places unless necessary. Maintain self-isolation. This is relevant not only during the current pandemic, because the risks of infections during febrile neutropenia are enormous - even your household can pose a danger, let alone a large number of strangers, for example, in stores.
6) If you are forced to visit a place with a large number of people, for example, to take a blood test, then be sure to wear a protective mask. Try to keep your distance from others.
The main drugs used in the treatment of febrile netropenia include antibiotics; specialized drugs are also used to stimulate an increase in the level of leukocytes and neutrophils - these are colony-stimulating factors (G-CSF).
These drugs are used to accelerate the formation, maturation and release of neutrophils from the bone marrow into the peripheral blood, where they begin to perform their functions and protect the body.
Why does this state matter to us?
Leukocytes are responsible for immunity and resistance to various unfavorable factors, therefore, when their level in the blood decreases, the body’s “defense” is primarily affected.
In this case, a person becomes more vulnerable to any infection: bacterial, viral or fungal.
In most cases, with the development of infectious complications, specialized antitumor treatment should be postponed. Consequently, in addition to the main danger for humans, which lies precisely in the infectious process, we are also faced with the fact that we have to postpone the treatment of cancer indefinitely until we deal with the infection.
Common and official names for white blood cells
The most popular, literary and popular name for leukocytes is the combination “white blood cells”. For ordinary people, more valuable information is how leukocytes are designated in a blood test, which allows you to interpret the results even before going to specialists. In medical literature and laboratory forms, these cells are encrypted with the abbreviation WBC. Also important is the information that allows you to analyze the ratio of different types of leukocytes in the detailed analysis result:
- The group of granulocytes, consisting of neutrophils, basophils and eosinophils, is collectively designated GRA or GRAN; when each of these cell subtypes is needed, the abbreviations NEUT, BASO, EOS or EOSIN are used, respectively.
- The abbreviation MID is used to identify the percentage composition of basophils, eosinophils, monocytes and immature cells. Some laboratories use the MXD designation for this group of cells.
- The percentage of lymphocytes is abbreviated as LYM or abbreviated as LY.
- The abbreviation MON characterizes the percentage of monocytes in the leukocyte formula.
Anatomy of Human Leukocytes - information:
Leukocytes (from the Greek λευκως - white and κύτος - cell, white blood cells) are a heterogeneous group of human or animal blood cells of different appearance and functions, identified on the basis of the absence of independent coloring and the presence of a nucleus.
The main function of leukocytes is protection. They play a major role in the specific and nonspecific protection of the body from external and internal pathogenic agents, as well as in the implementation of typical pathological processes. All types of leukocytes are capable of active movement and can pass through the capillary wall and penetrate into tissues, where they absorb and digest foreign particles. This process is called phagocytosis, and the cells that carry it out are called phagocytes. If a lot of foreign bodies have entered the body, then the phagocytes, absorbing them, greatly increase in size and are eventually destroyed. This releases substances that cause a local inflammatory reaction, which is accompanied by swelling, fever and redness of the affected area. Substances that cause an inflammatory reaction attract new leukocytes to the site of foreign body penetration. By destroying foreign bodies and damaged cells, leukocytes die in large quantities. Pus, which forms in tissues during inflammation, is an accumulation of dead leukocytes.
White blood cell count
Since the number of leukocytes in the blood reflects the state of the body's defenses, this indicator is of interest to doctors of all specialties. Its definition is included in the minimum of studies that are prescribed to all patients in a hospital or clinic. In a healthy person, the number of leukocytes in the blood is not constant. After heavy physical work, taking a hot bath, in women during pregnancy, during childbirth and before the onset of menstruation, it increases. The same happens after eating. Therefore, in order for the results of the analysis to be objective, it must be taken on an empty stomach, in the morning, without breakfast, you can only drink a glass of water. Normally, the content of leukocytes in 1 liter of blood of an adult ranges from 4.0–9.0 × 109. In children it is higher: at the age of one month – 9.2–13.8×109/l, from 1 to 3 years – 6–17×109/l, at the age of 4 to 10 years – 6.1–11, 4×109/l.
Types of leukocytes
White blood cells vary in origin, function and appearance. Some of the white blood cells are able to capture and digest foreign microorganisms (phagocytosis), while others can produce antibodies. According to morphological characteristics, leukocytes stained according to Romanovsky-Giemsa have been traditionally divided into two groups since the time of Ehrlich: - granular leukocytes, or granulocytes - cells with large segmented nuclei and revealing a specific granularity of the cytoplasm; Depending on the ability to perceive dyes, they are divided into neutrophilic, eosinophilic and basophilic. - non-granular leukocytes, or agranulocytes - cells that do not have a specific granularity and contain a simple non-segmented nucleus, these include lymphocytes and monocytes. The nuclei of mature neutrophil granulocytes have constrictions - segments, which is why they are called segmented. In immature cells, elongated rod-shaped nuclei are detected - these are neutrophilic rod-nucleated granulocytes. Even more “young” neutrophil granulocytes are called “metamyelocytes” (“young”). Most of the blood contains mature segmented neutrophilic granulocytes, fewer are band-nuclear granulocytes; young forms are rare. By the ratio of the number of mature and immature forms, one can judge the intensity of hematopoiesis. When blood is lost, the body begins to produce a large number of cells to replenish it. Since they do not have time to mature in the bone marrow, many immature forms appear in the blood. Similar processes occur in purulent diseases (appendicitis, peritonitis), sepsis, when the body tries to produce more protective cells. With leukemia, white blood cells begin to multiply uncontrollably, so many immature forms also appear in the blood.
The percentage of individual types of leukocytes in peripheral blood is called leukocyte formula . It is calculated per 100 leukocytes. The leukocyte formula allows the doctor to visualize which leukocytes are numerous and which are few. Studying the leukocyte formula helps in determining the severity of an infectious disease and in diagnosing leukemia. An increase in the number of immature neutrophil granulocytes is called a shift in the leukocyte formula to the left. The source of leukocytes is the bone marrow. Irradiation and some drugs (butadione, cytostatics, antiepileptic drugs) damage it. As a result, an insufficient number of leukocytes is produced, and leukopenia appears. An increase in the number of leukocytes is called leukocytosis, a decrease is called leukopenia. Most often, leukocytosis occurs in patients with infections (pneumonia, scarlet fever), purulent diseases (appendicitis, peritonitis, phlegmon), and severe burns. Leukocytosis develops within 1–2 hours after the onset of intense bleeding. An attack of gout may also be accompanied by leukocytosis. In some leukemias, the number of leukocytes increases several tens of times. Although the entry of microbes into the human body usually stimulates the immune system, resulting in an increase in the number of white blood cells in the blood, with some infections the opposite pattern is observed. If the body's defenses are depleted and the immune system is unable to fight, the number of white blood cells decreases. For example, leukopenia in sepsis indicates a serious condition of the patient and an unfavorable prognosis. Some infections (typhoid fever, measles, rubella, chickenpox, malaria, brucellosis, influenza, viral hepatitis) suppress the immune system, so they may be accompanied by leukopenia. A decrease in the number of leukocytes is also possible with systemic lupus erythematosus, some leukemias and metastases of bone tumors.
Neutrophils
The main purpose of neutrophils is to protect the body from infections. They phagocytose bacteria, that is, they “swallow” and “digest” them. In addition, neutrophils can produce special antimicrobial substances. During infections, neutrophils accumulate in large numbers at the site where bacteria enter the body. Pus is nothing more than dead neutrophils. Normally, in the blood of an adult, band neutrophils make up 1–5% of all leukocytes, segmented neutrophils make up 45–65%. An increase in the number of neutrophils, especially immature forms, indicates the presence of infection (abscess, appendicitis, pneumonia, pyelonephritis, tonsillitis, meningitis, sepsis). Similar changes are observed with myocardial infarction, burns, lead poisoning, severe blood loss, and leukemia. With some infections (typhoid fever, malaria, some forms of tuberculosis, hepatitis, influenza, measles, rubella), the number of neutrophils, on the contrary, decreases. A decrease in the number of neutrophils can occur with systemic lupus erythematosus, exposure to radiation and toxic chemicals (aniline, benzene, cytostatics), with some anemia and leukemia.
Eosinophils
Eosinophils remove excess histamine, which appears in allergic diseases. When infected with helminths, eosinophils penetrate into the intestinal lumen and are destroyed there, resulting in the release of substances that are toxic to helminths. Normally, the content of eosinophils in the blood is 1–5% of all leukocytes. The number of eosinophils increases with bronchial asthma, allergic dermatitis, drug allergies, infection with parasites (roundworms, echinococci, opisthorchis, giardia), with some leukemias and tumors, periarteritis nodosa.
Basophils
Not a single allergic reaction occurs without the participation of basophils. They play a role in the development of inflammation. Normally, the content of basophils in the blood is insignificant - up to 0.5% of all leukocytes. An increase in the number of basophils is extremely rare - with allergic reactions, some leukemias, lymphogranulomatosis, decreased thyroid function, and during treatment with estrogens.
Lymphocytes
Lymphocytes are the main patrol agents of the body. They check whether foreign molecules and microbes have penetrated into it, whether the cells of their own body have gotten out of control - whether they have mutated or begun to multiply uncontrollably, turning into a tumor. The main informants of lymphocytes are macrophages. They move throughout the body, “collect samples” that seem suspicious to them, and deliver them to lymphocytes. Normally, the content of lymphocytes in the blood of an adult is 25–35% of all leukocytes. In children under 6 years of age, there are significantly more lymphocytes in the blood than neutrophils, and after 6 years of age, the number of lymphocytes decreases, and neutrophils increase. An increase in the number of lymphocytes is observed in some infections (whooping cough, viral hepatitis, cytomegalovirus infection, tuberculosis, syphilis) and leukemia. With infectious mononucleosis, the content of lymphocytes also increases, but at the same time their shape changes and only in appearance they resemble monocytes. Hence the name of the disease. A decrease in the number of lymphocytes (lymphocytopenia) is typical for severe viral diseases, malignant tumors, immunodeficiencies, and also when prescribed glucocorticoids.
Monocytes
Monocytes are insufficiently mature cells. They begin to perform their main functions when they transform into macrophages - large motile cells that are found in almost all organs and tissues. Macrophages are a kind of orderlies. They “eat” bacteria and dead cells, and can “swallow” particles almost equal in size to them. Macrophages, as already mentioned, help lymphocytes in carrying out immune reactions. Normally, monocytes make up 1–8% of all leukocytes. The number of monocytes increases in some infectious diseases (infectious mononucleosis, malaria, syphilis, brucellosis). In tuberculosis, an increase in the number of monocytes is a sign of disease activity, and the ratio of the number of monocytes to the number of lymphocytes is important: normally it is 0.3–1, and with increased activity of tuberculosis it is more than 1. An increase in the number of monocytes is possible with sarcoidosis, leukemia, lymphogranulomatosis, systemic lupus erythematosus, rheumatoid arthritis and some vasculitis. Sometimes the doctor is not satisfied with one blood test and prescribes a repeat one. Thus, he assesses the dynamics of the disease and the effectiveness of treatment. In some cases, it is sufficient to re-determine only the total number of leukocytes without calculating the leukocyte formula. In other cases, the doctor is interested in more detailed data about the functioning of the immune system.
Leukocytosis
Leukocytosis is an increase in the total number of leukocytes in the blood over 9 G/l (9×109/l).
Classification . Leukocytosis is divided into absolute and relative.
Absolute leukocytosis is an increase in the number of leukocytes in the blood due to increased leukopoiesis of a reactive or tumor nature in the hematopoietic organs or their increased flow from the bone marrow depot into the blood vessels.
Relative leukocytosis is an increase in the number of leukocytes in the blood as a result of the redistribution of leukocytes from the parietal pool to the circulating one or their accumulation in the site of inflammation. In addition, due to the fact that an increase in the total number of leukocytes is usually combined with a predominant increase in the number of certain types of leukocytes, leukocytosis is divided into neutrophilia, eosinophilia, basophilia, lymphocytosis and monocytosis.
Pathogenesis of leukocytosis . The following mechanisms for the occurrence of leukocytosis can be distinguished:
- increased production of leukocytes in the hematopoietic organs (increased leukopoiesis of a reactive nature or with tumor hyperplasia of leukopoietic tissue), when the mitotic, maturing and reserve pool of leukocytes in the bone marrow increases;
- acceleration of the release of leukocytes from the bone marrow into the blood due to increased permeability of the bone marrow barrier under the influence of glycocorticoids, as well as increased proteolysis of the membrane surrounding the islet of granulopoiesis in septic conditions;
- redistribution of leukocytes as a result of their mobilization from the parietal (edge, marginal) pool into the circulating (after the administration of adrenaline, during emotional stress, under the influence of microorganism endotoxins), due to redistribution of blood (with shock, collapse) or increased migration of leukocytes to the site of inflammation (with appendicitis, phlegmon).
Leukocytosis is very often combined with impaired maturation of leukocyte cells in the bone marrow and the production of pathologically altered leukocytes. With leukocytosis resulting from reactive hyperplasia of leukopoietic tissue, as a rule, the functional activity of leukocytes increases, which leads to increased protective reactions of the body. Neutrophilic leukocytosis and monocytosis occur with a parallel increase in the phagocytic activity of leukocytes. Eosinophilic leukocytosis, due to the antihistamine function of eosinophilic granulocytes, plays a compensatory role in allergic reactions. At the same time, leukocytosis in leukemia can be combined with a decrease in the protective properties of leukopoietic cells, which causes immunological hyporeactivity, in which the body suffers from auto- and secondary infections.
Blood picture with leukocytosis . An increase in the total number of leukocytes during leukocytosis is accompanied by a change in the leukocyte formula (the percentage of individual forms of leukocytes, calculated by counting 200 cells in a stained blood smear). The absolute or relative nature of these changes is established by calculating the absolute content of various forms of granulo- and agranulocytes in 1 liter. The calculation is carried out based on knowledge of the total number of leukocytes in 1 liter of blood and the leukocyte formula. Thus, absolute neutrophilic leukocytosis in purulent inflammatory diseases is accompanied by a decrease in the percentage of lymphocytes in the leukocyte formula (relative lymphopenia). However, calculating the absolute number of lymphocytes against the background of high general leukocytosis makes it possible to establish the absence of suppression of the lymphocytic lineage. With leukocytosis, especially neutrophilic, immature cells often appear in the blood (nuclear shift to the left). A large number of degeneratively changed leukocytes during leukocytosis are observed in the blood during sepsis, purulent processes, infectious diseases, and the disintegration of a malignant tumor.
Leukopenia
Leukopenia is a decrease in the total number of leukocytes in the blood below 4 G/l (4 × 106 l).
Classification . Leukopenia, like leukocytosis, can be absolute and relative (redistribution). With a predominant decrease in certain forms of leukocytes, neutro-, eosino-, lympho-, and monocytopenia are distinguished.
The cause of neutropenia may be the action of infectious factors (influenza viruses, measles, typhoid toxin, typhus rickettsia), physical factors (ionizing radiation), drugs (sulfonamides, barbiturates, cytostatics), benzene, deficiency of vitamin B12, folic acid, anaphylactic shock , hypersplenism, as well as a genetic defect in the proliferation and differentiation of neutrophil granulocytes (hereditary neutropenia).
Eosinopenia is observed with increased production of corticosteroids (stress, Cushing's disease), administration of corticotropin and cortisone, and acute infectious diseases.
Lymphopenia develops with hereditary and acquired immunodeficiency conditions and stress. Lymphopenia is characteristic of radiation sickness, miliary tuberculosis, and myxedema.
Monocytopenia is observed in all those syndromes and diseases in which there is depression of the myeloid lineage of bone marrow hematopoiesis (for example, radiation sickness, severe septic conditions, agranulocytosis).
Pathogenesis of leukopenia . The development of leukopenia is based on the following mechanisms:
- decreased production of leukocytes in hematopoietic tissue;
- disruption of the release of mature leukocytes from the bone marrow into the blood;
- destruction of leukocytes in hematopoietic organs and blood;
- redistribution of leukocytes in the vascular bed;
- increased release of leukocytes from the body.
The mechanisms responsible for the inhibition of leukopoiesis are discussed above. A slowdown in the release of granulocytes from the bone marrow into the blood is observed in the syndrome of “lazy leukocytes” due to a sharp decrease in their motor activity caused by a defect in the cell membrane. The destruction of leukocytes in the blood may be associated with the action of the same pathogenic factors that cause lysis of leukopoietic cells in the hematopoietic organs, as well as with changes in the physicochemical properties and membrane permeability of the leukocytes themselves as a consequence of ineffective leukopoiesis, which leads to increased lysis of leukocytes, including in spleen macrophages. The redistribution mechanism of leukopenia is that the ratio between the circulating and parietal pool of leukocytes changes, which happens with blood transfusion shock, inflammatory diseases, etc. In rare cases, leukopenia can be caused by an increased release of leukocytes from the body (with purulent endometritis, cholecystoangiocholitis).
The main consequence of leukopenia is a weakening of the body's reactivity, caused by a decrease in the phagocytic activity of neutrophil granulocytes and the antibody-forming function of lymphocytes, not only as a result of a decrease in their total number, but also a possible combination of leukopenia with the production of functionally inferior leukocytes. This leads to an increase in the frequency of infectious and tumor diseases in such patients, especially with hereditary neutropenia, deficiency of T- and B-lymphocytes. A striking example of severe areactivity is acquired immunodeficiency syndrome of viral (AIDS) and radiation origin, as well as agranulocytosis and nutritional-toxic aleukia.
Agranulocytosis (granulocytopenia) is a sharp decrease in granulocytes in the blood (up to 0.75 g/l or less) against the background of a decrease in the total number of leukocytes (up to 1 g/l or less) of myelotoxic (with damage to the bone marrow) and immune origin (destruction of granulocytic cells a number of anti-leukocyte antibodies). The most common causes of agranulocytosis are medications, ionizing radiation, and some infections.
Aleukia is an aplastic lesion of the bone marrow with a sharp inhibition and even complete shutdown of myeloid hematopoiesis and lymphopoiesis. Alimentary-toxic aleukia develops when feeding on grain that has overwintered in the field and is contaminated with mold fungi that produce toxic substances. In this case, pancytopenia - a sharp drop in the number of leukocytes (alaukia), red blood cells (anemia) and platelets (thrombocytopenia). However, with leukopenia, compensatory reactions may also occur in the form of increased proliferation of some sprouts of the leukocyte lineage while suppressing others. For example, neutropenia may be accompanied by a compensatory increase in the production of monocytes, macrophages, eosinophils, plasma cells, and lymphocytes, which somewhat reduces the severity of clinical manifestations of neutropenia.
History of the study of leukocytes Ilya Mechnikov and Paul Ehrlich made important contributions to the study of the protective properties of leukocytes. Mechnikov discovered and studied the phenomenon of phagocytosis, and subsequently developed the phagocytic theory of immunity. Ehrlich is responsible for the discovery of various types of leukocytes. In 1908, the scientists were jointly awarded the Nobel Prize for their services.
An approximate list of diagnostic measures looks like this:
- Oral interview and history taking. The patient talks about complaints, provides information that could be important. For example, lifestyle, professional activity, past and current pathological processes. There are many options. Based on the results, the specialist or therapist determines the diagnostic vector.
- Ultrasound of the digestive tract. Doctors mainly examine the liver. In some cases this is not enough. Then scintigraphy and/or tomography is prescribed.
- Ultrasound examination of the kidneys. White blood cells are often excreted in the urine. This is quite revealing. Since with almost one hundred percent probability it indicates a focus of inflammation in the excretory tract. Ultrasound can detect pyelonephritis and autoimmune disorders. Also urolithiasis, developmental anomalies of a paired organ.
- X-ray of the lungs. To exclude tuberculosis and cancer processes. The problem is not always solved by routine methods. Like this. In this case…
- MRI is prescribed as needed. To confirm or exclude oncology with one hundred percent probability.
- If a tumor is found, a biopsy will be needed. A sample of the altered tissue is then sent to the laboratory. To understand what kind of neoplasia is occurring. It may well be benign.
- Blood chemistry. The goal is to obtain more information about the state of the body. The technique is used almost always. Examinations are prescribed to clarify the etiology of the disease. Origin of the violation in the laboratory protocol.
Leukocytes are blood cells whose task is to fight pathogens, infections, parasites and keep cancer and other abnormal cells under control. There are many of which are present in the body of a healthy person, but in a dormant state.
Deviations from the norm are possible. In this case, additional diagnostic measures will be needed.
Febrile neutropenia
The combination of an increase in body temperature with a decrease in the number of neutrophils is called febrile neutropenia. This is a life-threatening condition that suddenly and acutely develops in patients against the background of a decrease in the number of neutrophils circulating in the blood below 0.5x10*9/l.
Criteria:
- number of neutrophils in peripheral blood <0.5x109/l;
- a two-fold increase in body temperature >38.00C per day or a single increase in temperature >38.30C when measuring temperature in the mouth. This means that when measuring the temperature in the armpit, you and your doctor should start to worry about a temperature above 37.50C.
The main problem is that it is very difficult for oncologists to control this complication and take the necessary measures in a timely manner, since most patients develop febrile neutropenia during the period when they are no longer in the hospital.
Therefore, the patient must also be attentive to his condition and take timely measures: contact the doctor, donate blood as soon as possible and strictly follow what the attending physician recommends.
If your body temperature rises above 38.00C, you must take a clinical blood test as soon as possible. It is important! Without its result, it is impossible to say for sure whether the patient has febrile neutropenia or whether any urgent measures are needed.
Remember that this complication can turn into a big disaster if it is not recognized and treated in time.
If a combination of both criteria occurs (the number of neutrophils in the peripheral blood <0.5x10*9/l in combination with an increase in body temperature to 380-38.30C), you must contact your doctor as soon as possible or go to the oncological institution at your place of residence.
In the absence of timely treatment within 48 hours after the development of febrile neutropenia, death occurs in 50% of cases! Even with antibacterial therapy, the risk of death remains in 10% of cases.
This suggests that this is a very dangerous complication and should not be taken lightly.
About 80% of febrile episodes against the background of a reduced level of neutrophils in the blood are associated with the development of infection, which occurs in the absence of classical symptoms (pain, flushing, swelling, fever), and the main criterion of the infectious process is high body temperature.
Until recently, fever occurring in a patient with neutropenia was the basis for mandatory hospitalization and treatment in a hospital. However, as a result of clinical studies, a system for assessing complications in patients with febrile neutropenia was created. The doctor counts the points according to this scale and can assess whether there are risks when carrying out treatment on an outpatient basis.
Area of production and period of cell activity
All leukocyte cells, regardless of type, are predominantly produced in the bone marrow and lymph nodes; to a lesser extent, their “production” is developed in the spleen and tonsils. The lifespan of leukocytes varies, depending on the subtype of cells. The shortest period of life of monocytes is, which varies within a few hours. Granulocytes, which include basophils, neutrophils and eosinophils, live on average from ten to twelve days. Lymphocytes are distinguished by the longest period of vital activity; with normal functionality of the body, they live for several decades, accumulating information throughout their existence, guaranteeing a person immune protection from specific harmful agents that he had previously encountered. The presence of cumulative memory, with the ability to recognize infectious sources, allows you to identify harmful components in a timely manner, send a signal to protective cells, which prevents the likelihood of developing clinical indicators of the disease, through intensive control and destruction of pathogens at the initial stage of their pathogenic activity.