Blood consists not only of a liquid part (plasma) - it also contains a large number of different cells. Some of them are white blood cells, which are responsible for the formation and maintenance of strong immunity, protecting the body from germs, viruses and tumors. Leukocytes are divided into 5 main subtypes, the most numerous of which are represented by neutrophil cells.
Not a single clinical blood test is complete without determining their quantity. This is one of the simplest and most informative examinations that can be carried out by any laboratory in the Russian Federation, even an ORP point in a small town. Why does this study deserve so much attention? The answer is simple - it quite accurately reflects the work of one of the human systems, without which life would be impossible. Immune system.
Functions and types of cells
Neutrophils are a type of leukocyte - white blood cells that are vital to the immune system. These cells are heterogeneous; in total there are 4 types of neutrophils, which differ in their narrow purpose:
- myelocytes are preneutrophils, maximally immature cells without differentiation, which can eventually turn not only into a neutrophil, but into any blood element: from a platelet to an eosinophil;
- young neutrophils are an immature version of neutrophils, a conditional reserve of cells that begin to work in conditions of the body’s increased need for immune cells; in critical situations, a minimum number of such cells can be recorded in the bloodstream (no more than 1%);
- band neutrophils - make up no more than 5% of the total number of neutrophils, this is already a partially specialized cell of the immune system, it works in the bloodstream if the remaining neutrophils cannot cope with their functions;
- segmented neutrophils are the basis of neutrophil cells; up to 70% of the total number of structures constantly work in the bloodstream; they manifest themselves to the maximum during the infectious and inflammatory process in the body.
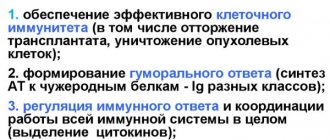
Thus, there are only two types of active, that is, capable of acting, neutrophils: segmented and band. They solve the main tasks that the body sets for neutrophils:
- lyse the cell membrane of the pathogen, killing viruses, bacteria, fungi, and other pathogenic microflora;
- enter into an antigen-antibody reaction with microbes, binding pathogenic flora, accelerating the relief of inflammation;
- absorb microbes and digest them (phagocytosis): one cell can destroy up to 30 “strangers”;
- inactivate viruses, reducing the rate of replication of pathogens, helping to stop inflammation of a viral nature.
What types of neutrophils are there?
Before full maturation, neutrophils go through 6 stages, based on which, cells are classified into:
- myeloblasts,
- Promyelocytes,
- Myelocytes,
- Metamyelocytes,
- Band,
- Segmented.
Stages of neutrophil development
All cell forms, except segmented ones, are considered functionally immature neutrophils.
Norms of neutrophils in the blood in adults and children
Neutrophils are abbreviated Neut and are counted as a percentage or absolute neutrophil count in units per liter of blood. The choice depends on the laboratory in which the analysis is performed. The norms of neutrophils in men, women, and children are presented in the tables.
In women, the variability of indicators is quite high, correlates with age, depends on hormonal fluctuations: puberty (especially delayed), menstruation, pregnancy. The data may decrease slightly depending on the patient’s condition when the test is taken, but never increase.
On average, the norm of neutrophils in the blood of women is up to 60%. This is slightly higher than that of men, which is explained by the physiological and immune characteristics of the female body.
| Woman's age | Norm in % (according to segmented form) |
| Up to 18 and from 45 to 60 | 50-55 |
| Until 21 | 51,5-56,5 |
| Before 35 and after 60 | 52-60 |
| Up to 45 | 50-58,5 |
In men, normal levels of neutrophils in the bloodstream are not significantly lower: up to 57%, and are correlated with the age and condition of the patient when the test was taken.
| Man's age | Norm in % (according to segmented form) |
| Up to 18 and from 35 to 45 | 50-54 |
| Under 21 and over 60 | 50-56 |
| Up to 35 | 51,5-57 |
| 45-60 | 49-53 |
In children, the calculation of the norm of neutrophils in the blood is carried out by day, month, year, since fluctuations are the most variable. A sharp increase in the first days of life is associated with the active formation of immunity and adaptation to the external environment.
| Child's age | Norm in % (according to segmented form) |
| Newborn | 59-60 |
| 12 hours | 65,1-68,1 |
| 1st day | 60,1-61,1 |
| 7 days | 39,9-42,9 |
| 14 days | 39,1-40,5 |
| 30 days | 35,5-38,2 |
| 6 months | 30,1-32,1 |
| 1 year | 30,5-31,5 |
| 2 years | 30,3-33,5 |
| 4 years | 40,1-42,5 |
| 6 years | 49,1-51,1 |
| 8 years | 50,5-53,1 |
| 10 years | 50,1-54,1 |
| 11-18 years old | 52,5-55,5 |
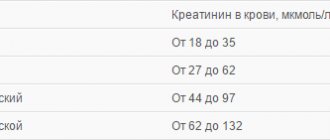
Degrees of neutropenia
To assess how dangerous neutrophil deficiency is in humans, 4 degrees of severity of this condition were distinguished. The main classification criterion is the absolute number of cells in the patient’s blood. The indicators differ fundamentally between the two population groups. The first category includes all adults and children over 12 months of age. For a younger child, the classification by degree is somewhat different (to a lesser extent).
| Patient group Degrees | Adults and children over one year of age, cells/µl | Children, under 12 months, cells/µl |
| Norm | More than 1500 | More than 1000 |
| I (light) | 1500-1000 | 999-500 |
| II (medium) | 999-500 | 499-100 |
| III (severe) | 499-100 | Less than 100 |
What do low neutrophils less than 100 cells/µl indicate? This condition is quite dangerous for a person, since his body is practically defenseless against any bacterial or fungal infection. Determining such changes in the examination results is a reason to immediately contact a hematologist and begin therapy.
Pathological causes of growth
The norm of neutrophils in the blood changes in most cases due to pathological reasons, the main of which are:
- inflammation of infectious or autoimmune origin;
- endocrine pathologies;
- tumor growth, metastasis;
- physician error during surgery (iatrogenic factor).
There is an exception to the rule: neutrophils can remain normal against the background of a manifest pathological process, which indicates depletion of the immune system and requires immediate adequate treatment.
When is the analysis performed?
A blood test for neutrophils is usually taken when a patient has strange and, at first glance, inexplicable symptoms. There are quite a lot of signs that belong to this group, so only the most common ones will be listed:
What are basophils responsible for in the blood?
- Suspicion of poisoning by poisons or heavy metals.
- The presence of any type of anemia.
- Aching pain localized in muscles, bones and joints.
- General weakness.
- Tendency to faint.
- Loss of balance.
- Prolonged depression combined with inexplicable aggressiveness.
- Regular increases in body temperature.
- Rash on the surface of the skin.
- The appearance of hematomas not associated with mechanical damage.
- Dramatic weight loss.
- Swelling of the lymph nodes.
- Cardiopalmus.
- Suspicious shade of urine.
- Drowsiness.
- Dizziness.
- Difficulty swallowing functions.
- Intense thirst that cannot be quenched.
If the attending physician suspects that the patient has tissue necrosis or inflammatory diseases, he will immediately issue a referral for a blood test, which should be taken as soon as possible. Prolonged healing of scratches and small cuts is a good reason to conduct a hematological study for neutrophils.
For people who have undergone surgery, a blood test is required to constantly monitor their condition.
Reasons for the downgrade
A decrease in the number of neutrophils in the blood compared to the norm is called a shift in the leukocyte formula to the left. There are several reasons for this condition:
- HIV;
- aplastic anemia;
- severe infections;
- the period after a serious illness, prolonged fasting, cachexia;
- alcoholism;
- hepatitis;
- sepsis;
- radiation sickness;
- intoxication of various etiologies, taking medications (antibiotics, antiviral anti-inflammatory drugs, drugs for the treatment of hyperthyroidism, for chemotherapy);
- deficiency of minerals, B vitamins;
- bone marrow damage;
- enlarged spleen;
- metastasis of cancer of any location to the bone marrow or myeloproliferative processes;
- genetic predisposition;
- hyperglycemia;
- idiosyncrasy, when the reason for the decrease in the concentration of neutrophils in the bloodstream is unclear.
How to donate blood correctly
Most laboratories advise not to eat for 12 hours before the test, not to smoke at least 30 minutes before the test, and to avoid physical and emotional stress 30 minutes before the test. Alcohol should be avoided at least a day before donating blood, the same goes for taking medications (in consultation with your doctor).
02 November, 15:24
Reasons for the increase in some cells and the decrease in others
An increase or decrease in neutrophil levels in the blood can be correlated with many factors of natural and pathological origin. There are many uniform elements that are called upon to fight “strangers” in this case. There are two options:
- if neutrophils are elevated, and lymphocytes, on the contrary, this is the first phase of the immune reaction, when central immunity is not yet active enough, and there is no need for it: fluctuations are insignificant;
- if neutrophils are reduced, and lymphocytes, on the contrary, this is the second phase of the immune response, when central cells work more actively, and local-level structures reduce their intensity for a short time.
The general rule is one: when neutrophils increase, lymphocytes decrease and vice versa. This is the norm. There is no simultaneous increase or decrease observed.
Treatment
Correction is determined by the specific cause of the pathological process. The goal is not to raise neutrophils in the blood using artificial methods; it is necessary to eliminate the source of the problem. Drug therapy is practiced.
In case of infectious genesis of the disorder, the following means are used:
- Antibiotics. Different types.
- Stimulators of leukocyte synthesis. Leukogen and others. Carefully.
- Local antiseptic drugs.
If we are talking about autoimmune reactions:
- Suppressors. To suppress the activity of protective forces.
- Glucocorticoids. Prednisolone and similar.
- Others may be used. According to the needs and prescription of the treating specialist.
The number of neutrophils in the blood also shows the effectiveness of therapy, therefore it is possible to study the quality of the correction carried out according to this criterion.
Otherwise, the techniques depend on the clinical situation. Diabetes mellitus requires glucose control, malignant tumors require surgical treatment, etc.
Special cases of decreased neutrophils
We are talking about genetically determined neutropenia, which is quite rare, but affects the result of a blood test. This:
- benign chronic neutropenia is asymptomatic, there is no danger to life, but when interpreting the analysis, this point is always taken into account;
- cyclic neutropenia occurs in one person per million, does not affect the quality of life, manifests itself in a periodic causeless decrease and then restoration of neutrophils to normal;
- Kostmann's syndrome is a condition when neutrophils are deprived of the opportunity to mature, as a result a person is deprived of natural protection and constantly suffers from all possible infections. Today, provided that the pathology is detected in a timely manner, patients are given courses of drug correction.
After two crossings the norms are equalized
The leukocyte formula of children (especially small ones) is noticeably different from that of adults. All this is explained by a change in the ratio of lymphocytes and neutrophils from birth to 14-15 years of age.
Many have heard that children have certain crossovers (if you draw a graph) and this is what it all means:
- In a newborn child who has just been born, the number of neutrophil granulocytes is somewhere in the range of 50-72% , and lymphocytes - about 15-34%, however, the number of neutrophils continues to increase in the first hours of life. Then (not even a day passes) the population of neutrophil leukocytes sharply changes direction in the opposite direction and begins to decrease, while lymphocytes move towards it, that is, they increase. At some point, usually between days 3 and 5 of life, the numbers of these cells equalize and the curves on the graph intersect - this is the first cross
. After the crossover, lymphocytes will continue to increase for some time, and neutrophils will decrease (approximately until the end of the second week of life), only to turn in the opposite direction again. - After half a month, the situation changes again: the level of lymphocytes decreases, the content of neutrophils increases, only this process no longer occurs at such a fast pace. The crossing points of these cells will be reached when the child is going to first grade - this is the time of the second crossing
.
Table: norms of neutrophils and other leukocytes in children by age
The value of the indicator for diagnostics
When monitoring a patient's health status, the content of band cells during antibacterial therapy, inflammatory diseases, and also in the postoperative period is of particular importance to the doctor. An increase in the indicator indicates the development of a purulent process and the insensitivity of the pathogen to antibiotics.
One of the most common examples of such problems is an increase in neutrophils with the flu or a severe cough during or after a cold. This symptom indicates the addition of a bacterial infection and the need for antimicrobial therapy.
PN cells, when measuring the quantitative composition of blood, are considered one of the markers that answers the question about the improvement or deterioration of the patient’s health, the possibility of stopping conservative treatment, or the quality of preparation for surgery.
If the analysis shows values higher than normal after an infectious disease, then there is a possibility of complications or, conversely, a lot of neutrophils indicate restoration of immune function. Therefore, you should not refuse a blood test, even if your health has improved.