Description
Shock is a symptom complex of disorders of the vital functions of the body that arise as a result of a discrepancy between tissue blood flow and the metabolic needs of tissues.
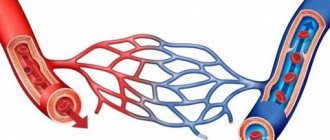
During the development of shock, the body's main task is to maintain adequate blood flow to vital organs (heart and brain). Therefore, initially, vasoconstriction occurs in other organs and tissues, thus achieving centralization of blood circulation. Such prolonged narrowing of blood vessels over time leads to the development of ischemia - a decrease in blood supply to an organ or tissue that occurs due to a weakening or cessation of arterial blood flow. This leads to the production of biologically active substances that increase vascular permeability, which ultimately leads to vasodilation. As a result, the body’s protective adaptive mechanism—centralization of blood circulation—is disrupted, which entails serious consequences.
According to pathogenesis, the following types of shock are distinguished:
- hypovolemic;
- traumatic;
- cardiogenic;
- infectious-toxic;
- anaphylactic;
- septic;
- neurogenic;
- combined (contains all the pathogenetic elements of various shocks).
The consequences of shock depend on the cause that led to the development of this condition. For example, shock can lead to complications such as failure of a number of internal organs, swelling of the lungs and brain. Such dire consequences can lead to death, so shock requires increased attention.
Anaphylactic
Now let's talk about what anaphylactic shock is. This is a severe allergic reaction caused by repeated exposure to an allergen. The amount of the latter may be very small. But the higher the dose, the longer the shock. An anaphylactic reaction of the body can occur in several types.
- Skin and mucous membranes are affected. Itching, redness, and Quincke's edema appear.
- Disruption of the nervous system. In this case, the symptoms are as follows: headaches, nausea, loss of consciousness, sensory disturbance.
- Deviation in the functioning of the respiratory system. Choking, asphyxia, and swelling of the small bronchi and larynx appear.
- Damage to the heart muscle provokes myocardial infarction.
In order to more thoroughly study what anaphylactic shock is, you need to know its classification by severity and symptoms.
- Mild degrees last from a few minutes to two hours and are characterized by: itching and sneezing; discharge from the sinuses; redness of the skin; sore throat and dizziness; tachycardia and decreased blood pressure.
- Average. Signs of the appearance of this degree of severity are as follows: conjunctivitis, stomatitis; weakness and dizziness; fear and inhibition; noise in the ears and head; the appearance of blisters on the skin; nausea, vomiting, abdominal pain; urinary disturbance.
- Severe degree. Symptoms appear instantly: a sharp decrease in pressure, blue skin, almost no pulse, lack of response to any irritants, cessation of breathing and cardiac activity.
Symptoms
Photo: peterkfitness.com
In case of shock, you can pay attention to the patient’s appearance. Such a person has pale and cold-to-the-touch skin. The exception is septic and anaphylactic shock, in which the skin is warm at the beginning of development, but then it does not differ in any way from the characteristics of other types of shock. General weakness, dizziness, and nausea are pronounced. Excitement may develop, followed by lethargy or coma. Blood pressure decreases significantly, which poses a certain danger. As a result, the stroke volume of blood required to supply organs and tissues with oxygen is reduced. Therefore, tachycardia occurs - an increase in the number of heart contractions. In addition, the appearance of oligoanuria is noted, which means a sharp decrease in the amount of urine excreted.
With traumatic shock, patients complain of severe pain caused by the injury. Anaphylactic shock is accompanied by shortness of breath, which occurs due to bronchospasm. Significant blood loss can also lead to the development of shock, in which case attention is drawn to internal or external bleeding. In septic shock, elevated body temperature is detected, which is difficult to control by taking antipyretic drugs.
Clinical picture of shock
The clinical picture of shock differs depending on the severity of exposure to external stimuli. To correctly assess the condition of a person who has suffered shock and provide assistance with shock, several stages of this condition should be distinguished:
1. Shock 1st degree. The person retains consciousness and makes contact, although his reactions are slightly inhibited. Pulse indicators – 90-100 beats, systolic pressure – 90mm;
2. Shock 2 degrees. The person’s reactions are also inhibited, but he is conscious, answers questions correctly, and speaks in a muffled voice. There is rapid shallow breathing, a rapid pulse (140 beats per minute), blood pressure is reduced to 90-80 mm Hg. The prognosis for such shock is serious, the condition requires urgent anti-shock procedures;
3. Shock 3 degrees. A person’s reactions are inhibited, he does not feel pain and is adynamic. The patient speaks slowly and in a whisper, and may not answer questions at all, or in monosyllables. Consciousness may be completely absent. The skin is pale, with pronounced acrocyanosis, and covered with sweat. The victim's pulse is barely noticeable, palpable only in the femoral and carotid arteries (usually 130-180 beats/min). Shallow and rapid breathing is also observed. Venous central pressure may be below zero or zero, and systolic pressure may be below 70 mm Hg.
4. Stage 4 shock is a terminal state of the body, often expressed in irreversible pathological changes - tissue hypoxia, acidosis, intoxication. The patient's condition with this form of shock is extremely severe and the prognosis is almost always negative. The victim’s heart cannot be heard, he is unconscious and breathes shallowly with sobs and convulsions. There is no reaction to pain, the pupils are dilated. In this case, blood pressure is 50 mm Hg, and may not be determined at all. The pulse is also inconspicuous and is felt only in the main arteries. Human skin is gray, with a characteristic marble pattern and spots similar to those of a corpse, indicating a general decrease in blood supply.
Diagnostics
Photo: medaboutme.ru
For some time, the state of shock may go unnoticed, since there is no specific symptom indicating exclusively the development of shock. Therefore, it is important to evaluate all the symptoms the patient has and analyze the situation individually in each case. To diagnose shock, it is necessary to identify signs of insufficient blood circulation to tissues, as well as to detect the inclusion of compensatory mechanisms of the body.
First of all, attention is paid to the patient’s appearance. The skin is often cold to the touch and has a pale appearance. Cyanosis (bluish discoloration of the skin and/or visible mucous membranes) may be detected. To confirm hypotension, blood pressure is measured. Patients complain of general weakness, dizziness, nausea, palpitations, and the amount of urine excreted sharply decreases.
It is important to quickly compare all the symptoms, make the correct diagnosis and begin appropriate treatment.
The occurrence of pathology
What is the pathogenesis of shock? Let's look at this in more detail. To develop a response, the body must have:
- Time period.
- Disorders of cellular metabolism.
- Reducing the amount of circulating blood.
- Damage incompatible with life.
Under the influence of negative factors, reactions begin to develop in the body:
- Specific - depends on the nature of the impact.
- Nonspecific - depends on the strength of the impact.
The first ones are called the general adaptation syndrome, which always proceeds in the same way and has three stages:
- Anxiety is a reaction to damage.
- Resistance is a manifestation of defense mechanisms.
- Exhaustion is a violation of adaptation mechanisms.
Thus, based on the above arguments, shock is a nonspecific reaction of the body to a strong impact.
In the mid-nineteenth century, N.I. Pirogov added that the pathogenesis of shock includes three phases. Their duration depends on the patient's response and duration of exposure.
- Compensated shock. The pressure is within normal limits.
- Decompensated. Blood pressure is reduced.
- Irreversible. Organs and systems of the body are damaged.
Now let's take a closer look at the etiopathogenetic classification of shock.
Treatment
Photo: likar.info
Shock is an emergency condition that can lead to irreversible consequences. Therefore, it is extremely important to provide timely medical assistance. Before specialists arrive, people nearby should take first aid measures. First, you need to give the person a horizontal position with the leg end raised. Such actions help to increase venous return to the heart, which leads to an increase in stroke volume of the heart. During shock, the heart can no longer cope with the stroke volume of blood required to deliver the required amount of oxygen to the tissues. A horizontal position with elevated legs, although it does not completely compensate for the insufficiency of the stroke volume of the heart, but helps to improve this condition.
Secondly, warming the body is recommended. For this purpose, heating pads with warm water are suitable, which are placed in the armpits and on the area of the groin folds. In addition, you can use a warm blanket.
Medical care consists of infusion therapy and the administration of drugs whose action is aimed at narrowing blood vessels. Infusion therapy is based on the introduction of various solutions of a certain volume and concentration into the bloodstream to fill the vascular bed.
The use of medications that constrict blood vessels is necessary to maintain blood pressure.
In case of breathing problems, oxygen therapy or mechanical ventilation is used.
These general measures are aimed at combating the pathogenesis of shock; there is also symptomatic treatment, different for each type of shock. For example, in case of traumatic shock, it is necessary to administer painkillers, immobilize fractures, or apply a sterile dressing to the wound. Cardiogenic shock requires treatment of the cause contributing to the development of shock. Hypovolemic shock is often associated with blood loss, so it is important to understand that without eliminating the cause, that is, stopping the bleeding (application of a tourniquet, pressure bandage, squeezing a vessel in the wound, etc.), general measures will not have the desired effect. Septic shock is accompanied by fever, so antipyretics are used as symptomatic treatment, and antibacterial drugs are prescribed to eliminate the cause itself. When treating anaphylactic shock, it is important to prevent delayed systemic manifestations; glucocorticosteroids and antihistamines are used for this purpose. It is also necessary to stop the phenomenon of bronchospasm.
Traumatic
Now let's talk about what traumatic shock is. Wounds, cuts, severe burns, concussions - everything that is accompanied by a serious human condition causes this pathological process. Blood flow in veins, arteries, and capillaries is weakened. A large amount of blood is lost. The pain syndrome is pronounced. There are two phases of traumatic shock:
- Erectile. Occurs simultaneously with injury. During this period, the nervous system is highly excited.
- Torpidnaya. There is a depression of the nervous system, the activity of the kidneys, lungs, heart, and liver.
The second phase, in turn, is divided into the following degrees:
- Easy. The person is conscious, there is slight lethargy and shortness of breath. Reflexes are slightly reduced. The pulse is rapid, the skin is pale.
- Average. Lethargy and lethargy are clearly expressed. The pulse is increased.
- Heavy. The victim is conscious, but does not perceive what is happening. The skin has an earthy gray color. The tips of the fingers and nose are bluish. The pulse is increased.
- State of pre-agony. The person has no consciousness. It is almost impossible to determine the pulse.
Medicines
Photo: alkotraz.ru
When shock develops, it is important to provide access to a vein as quickly as possible, preferably not to one, but to several at once. This is necessary to start infusion therapy, as well as administer drugs directly into the bloodstream. Infusion therapy influences the main links of pathogenesis. It is able to maintain an optimal level of BCC (circulating blood volume), which leads to stabilization of hemodynamics, improves microcirculation, thereby increasing the delivery of oxygen to tissues, and improves metabolism in cells.
Infusion solutions used for shock include:
- crystalloids (isotonic NaCl solution, Ringer's solution, glucose solutions, mannitol, sorbitol);
- colloids (hemodez, polydesis, polyoxidin, polyglucin, rheopolyglucin).
Usually a combination of crystalloid and colloid solutions is used. This tactic allows you to replenish the volume of circulating blood, and also regulates the balance of intracellular and interstitial fluids. The choice of volume and ratio of crystalloid and colloid solutions depends on each clinical case, which has its own characteristics.
Of the drugs that cause narrowing of the lumen of blood vessels, the main one is adrenaline. Intravenous administration promotes the accumulation of the required concentration of the drug directly in the blood, which leads to the most rapid manifestation of the effect than with other methods of administration. Dobutamine and dopamine also have this effect. Their effect begins approximately 5 minutes after intravenous administration and lasts about 10 minutes.
First aid for shock
First of all, it is necessary to visually examine the victim and try to determine what caused the shock. If necessary, ask him a few clarifying questions. Next, if you do not find any external injuries, carefully place the patient in a horizontal position.
If there is vomiting or bleeding from the mouth, turn his head to the side to prevent him from choking. If the victim has a back injury, under no circumstances should he be moved or laid down. You need to leave it in the position in which it is currently located. Provide first aid if open wounds are detected: bandage, treat, apply a splint if necessary.
Before the ambulance arrives, monitor vital signs such as pulse, heart rate, and breathing.
Folk remedies
Photo: trumatter.files.wordpress.com
Shock of various etiologies requires exclusively medical care; no recipes of folk remedies can improve the patient’s condition. Therefore, it is important not to waste precious time, but to immediately call specialists who will provide the necessary assistance and save you from possible irreversible consequences. While waiting for the ambulance team to arrive, you should follow the first aid measures that were described earlier (put the person in a horizontal position with the leg end raised, warm the body). Not only the effectiveness of treatment, but also a person’s life depends on the correct actions!
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Painful
Painful shock - what is it? This is a condition that is caused by severe pain. Typically this situation occurs when: a fall or injury. If heavy blood loss is added to the pain syndrome, then death cannot be ruled out.
Depending on the reasons that caused this condition, the body’s reaction can be exogenous or endogenous.
- The exogenous type develops as a result of burns, injuries, surgeries and electric shocks.
- Endogenous. The reason for its appearance is hidden in the human body. Provokes a response: heart attack, hepatic and renal colic, rupture of internal organs, stomach ulcers and others.
There are two phases of pain shock:
- Initial. It doesn't last long. During this period, the patient screams and rushes about. He is agitated and irritable. Breathing and pulse are increased, blood pressure is increased.
- Torpidnaya. Has three degrees:
- First, the central nervous system is inhibited. The pressure drops, moderate tachycardia is observed, reflexes are reduced.
- The second – the pulse quickens, breathing is shallow.
- The third one is hard. The pressure has been reduced to critical levels. The patient is pale and cannot speak. Death may occur.