Allergist
Bykov
Sergey Anatolyevich
17 years of experience
Allergist (immunologist), Candidate of Medical Sciences, member of the Russian Association of Allergists and Clinical Immunologists, member of the European Academy of Allergology and Clinical Immunology (EAACI).
Make an appointment
Anaphylactic shock is a condition that in 20% of cases or more can lead to death. It is characterized as the body’s strongest immune reaction to an irritant, one or another allergen. This affects the skin and mucous membranes, as well as the digestive, respiratory and cardiovascular systems. If the patient does not receive prompt medical attention for anaphylactic shock, death may occur. Therefore, it is so important to know the first aid measures for the victim, the signs and symptoms of this condition.
Causes of anaphylactic shock
Anaphylactic shock can occur due to many factors, be it food, drugs or animals. The main causes of anaphylactic shock:
| Allergen group | Main allergens |
| Medications |
|
| Animals |
|
| Plants |
|
| Food |
|
What allergens can cause shock?
Types of likely irritants:
- various medicines, serums, vaccines, etc.;
- food products, most often nuts, citrus fruits, fish, honey, chocolate, eggs, strawberries, preservatives. Often intolerance is caused by food contaminated with parasites;
- aeroallergens (pollen from plants, trees during the flowering season, dust, mold spores);
- antibiotics, especially the penicillin series;
- painkillers (most often novocaine);
- poison that is injected by insects (bees, wasps, etc.) when bitten;
- saliva, skin scales, fur, fluff of domestic animals;
- irritants at work (formaldehyde, nickel salts, etc.).
A state of shock occurs most quickly when the provocateur enters the body intramuscularly or intravenously. Slower - if the path was through the respiratory tract or skin. After eating, signs of anaphylactic shock are observed after 1-2 hours.
What happens in the body during shock?
The pathogenesis of the disease is quite complex and consists of three successive stages:
- immunological
- pathochemical
- pathophysiological
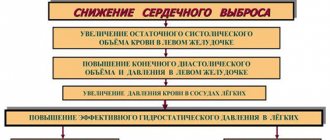
The pathology is based on contact of a specific allergen with cells of the immune system, after which specific antibodies (Ig G, Ig E) are released. These antibodies cause a huge release of inflammatory factors (histamine, heparin, prostaglandins, leukotrienes, and so on). Subsequently, inflammatory factors penetrate into all organs and tissues, causing disruption of circulation and blood clotting in them, up to the development of acute heart failure and cardiac arrest.
Typically, any allergic reaction develops only upon repeated contact with the allergen. Anaphylactic shock is dangerous because it can develop even when the allergen first enters the human body.
What is anaphylaxis?
Anaphylactic shock, or anaphylaxis, is an acute condition that occurs as an immediate allergic reaction that occurs when the body is repeatedly exposed to an allergen (foreign substance).
It can develop in just a few minutes, is a life-threatening condition and requires emergency medical attention.
Mortality is about 10% of all cases and depends on the severity of anaphylaxis and the speed of its development. The annual incidence is approximately 5-7 cases per 100,000 people.
Children and young people are mainly susceptible to this pathology, since most often it is at this age that a repeated encounter with the allergen occurs.
Symptoms of anaphylactic shock
Variants of the course of the disease:
- Malignant (fulminant) - characterized by a very rapid development of acute cardiovascular and respiratory failure in the patient, despite the therapy. The outcome in 90% of cases is fatal.
- Prolonged - develops with the introduction of long-acting drugs (for example, bicillin), so intensive therapy and monitoring of the patient must be extended to several days.
- Abortion is the easiest option; the patient’s condition is not in danger. Anaphylactic shock is easily relieved and does not cause residual effects.
- Recurrent - characterized by repeated episodes of this condition due to the fact that the allergen continues to enter the body without the knowledge of the patient.
In the process of developing symptoms of the disease, doctors distinguish three periods:
- Precursor period
Initially, patients feel general weakness, dizziness, nausea, headache, and rashes on the skin and mucous membranes in the form of hives (blisters) may appear. The patient complains of a feeling of anxiety, discomfort, lack of air, numbness of the face and hands, deterioration of vision and hearing.
- High period
It is characterized by loss of consciousness, a drop in blood pressure, general pallor, increased heart rate (tachycardia), noisy breathing, cyanosis of the lips and extremities, cold sticky sweat, cessation of urine output or, conversely, urinary incontinence, itching.
- Period of recovery from shock
May continue for several days. Patients remain weak, dizzy, and lack of appetite.
Adrenaline (epinephrine)
Adrenaline or epinephrine is the most important drug that “starts” the heart and increases blood pressure. In the first seconds from the onset of an anaphylactic reaction, you can pour half the contents of the ampoule under the patient’s tongue, where absorption is most intense.
Epinephrine solution can also be used to inject the injection site of the drug that triggered the allergy, or the area around the insect bite. Adrenaline will cause a local narrowing of the arteries and prevent the allergen from spreading throughout the body.
Severity of the condition
| Mild course | Moderate | Severe course | |
| Arterial pressure | Decreases to 90/60 mm Hg | Decreases to 60/40 mm Hg | Not determined |
| Precursor period | 10-15 minutes | 2-5 minutes | Seconds |
| Loss of consciousness | Momentary fainting | 10-20 minutes | More than 30 minutes |
| Effect of treatment | Treats well | The effect is delayed, requires long-term observation | No effect |
For mild flow
Precursors for mild shock usually develop within 10-15 minutes:
- skin itching, erythema, urticaria rash
- feeling of heat and burning throughout the body
- if the larynx swells, the voice becomes hoarse, even aphonic
- Quincke's edema of various localizations
A person manages to complain to others about his feelings during mild anaphylactic shock:
- They feel headache, dizziness, chest pain, decreased vision, general weakness, lack of air, fear of death, tinnitus, numbness of the tongue, lips, fingers, pain in the lower back, in the abdomen.
- There is cyanotic or pale skin on the face.
- Some people may have bronchospasm - wheezing can be heard at a distance, difficulty breathing.
- In most cases, vomiting, diarrhea, abdominal pain, involuntary urination or defecation occur.
- But even then, patients lose consciousness.
- Pressure is sharply reduced, thready pulse, muffled heart sounds, tachycardia
For moderate cases
Harbingers:
- As well as in mild cases, general weakness, dizziness, anxiety, fear, vomiting, heart pain, suffocation, Quincke's edema, urticaria, cold sticky sweat, cyanosis of the lips, pallor of the skin, dilated pupils, involuntary defecation and urination.
- Often - tonic and clonic convulsions, followed by loss of consciousness.
- Low or undetectable blood pressure, tachycardia or bradycardia, thready pulse, muffled heart sounds.
- Rarely - gastrointestinal, nosebleeds, uterine bleeding.
Severe course
The rapid development of shock does not give the patient time to complain about his sensations, since loss of consciousness occurs within a few seconds. A person needs immediate medical attention, otherwise sudden death occurs. The patient has severe pallor, foam at the mouth, large drops of sweat on the forehead, diffuse cyanosis of the skin, dilated pupils, tonic and clonic convulsions, wheezing breathing with prolonged exhalation, blood pressure is not determined, heart sounds are not heard, the pulse is thready, almost palpable.
There are 5 clinical forms of pathology:
- Asphyxial - in this form, patients have symptoms of respiratory failure and bronchospasm (shortness of breath, difficulty breathing, hoarseness), often developing Quincke's edema (swelling of the larynx until breathing stops completely);
- Abdominal - the predominant symptom is abdominal pain, simulating symptoms of acute appendicitis or perforated gastric ulcer (due to spasm of intestinal smooth muscles), vomiting, diarrhea;
- Cerebral - a feature of this form is the development of edema of the brain and meninges, manifested in the form of convulsions, nausea, vomiting that does not bring relief, a state of stupor or coma;
- Hemodynamic - the first symptom is pain in the heart area, reminiscent of myocardial infarction and a sharp drop in blood pressure;
- Generalized (typical) – occurs in most cases, includes all common manifestations of the disease.
Diagnosis of anaphylactic shock
Diagnosis of the pathology must be carried out as quickly as possible, so the prognosis for the patient’s life largely depends on the doctor’s experience. Anaphylactic shock is easily confused with other diseases; the main factor in making a diagnosis is the correct history taking!
- A general blood test reveals anemia (decrease in the number of red blood cells), leukocytosis (increase in white blood cells) with eosinophilia (increase in eosinophils).
- A biochemical blood test determines an increase in liver enzymes (AST, ALT, alkaline phosphatase, bilirubin), and kidney tests (creatinine, urea).
- A plain chest x-ray reveals interstitial pulmonary edema.
- Enzyme immunoassay is used to detect specific antibodies (Ig G, Ig E).
- If the patient finds it difficult to answer, after which he develops an allergic reaction, he is recommended to consult an allergist with allergy tests.
How to recognize anaphylaxis in a child?
The diagnosis of shock is made based on the typical clinical picture, blood pressure levels, heart rate, and the results of laboratory and instrumental studies. Anamnesis is of great importance.
To make a diagnosis you need:
- Physical examination (listening to the heart and lungs, palpation, percussion).
- Measurement of blood pressure and pulse.
- Visual inspection.
- Examination of the larynx.
- Assessment of neurological status.
- General (clinical) blood test. Detects anemia (decrease in hemoglobin and red blood cells), a high content of leukocytes and an increase in eosinophils.
- Blood chemistry.
- Linked immunosorbent assay.
- Allergy tests. The content of tryptase, interleukin-5, histamine and immunoglobulin is determined.
- Skin allergy tests. Conducted after assistance has been provided.
- Instrumental studies (ultrasound of the heart, electrocardiography).
In case of shock, a preliminary diagnosis is made based only on the clinical picture. Tests and other studies are carried out later due to the urgency of treatment.
Differential diagnosis of anaphylactic shock (table)
Shock must be distinguished from cardiac pathology and other emergency conditions.
| Pathology | Causes | Predominant symptoms |
| Anaphylactic shock | Contact with an allergen | Decreased blood pressure, feeling of fear, impaired consciousness, rashes, swelling |
| Cardiogenic shock | Heart attack, myocarditis, poisoning, tamponade, thromboembolism, severe infections | Radiating chest pain, signs of respiratory failure and pulmonary edema |
| Acute heart failure | Coronary heart disease, dilated cardiomyopathy, arrhythmias, hypertension | Attacks of suffocation, feeling of lack of air, cough with sputum, swelling of the neck veins, cyanosis of the skin, drop in blood pressure, thready pulse |
| Septic shock | Foci of purulent infection, prolonged hospitalization, contaminated wounds, immunodeficiency | Persistent arterial hypotension, fever |
| Myocardial infarction | Diabetes mellitus, atherosclerosis of the coronary arteries, coronary thrombosis, smoking, angina pectoris, high blood pressure, lipid metabolism disorders, unhealthy diet, obesity | Chest pain lasting more than half an hour, not relieved by nitrates, increased pressure followed by a drop, shortness of breath, agitation, tachycardia, increased temperature |
| Status epilepticus | Epilepsy, traumatic brain injury, tumors, encephalitis, cysts, cerebrospinal fluid congestion, diabetes, poisoning | Low blood pressure, impaired consciousness, convulsions, vomiting, rapid heartbeat, dysfunction of the pelvic organs, dilated pupils, respiratory disorders |
| Hypoglycemic coma | Failure to comply with the dosage and frequency of administration of insulin and oral hypoglycemic agents, lack of knowledge of injection techniques, skipping meals | Feeling of hunger, cold and sticky sweat, weakness, loss of consciousness, shallow breathing, drowsiness, hand tremors, convulsions |
| Pulmonary embolism | Deep vein occlusion by thrombus, thrombophilia, cardiovascular disease, sepsis, antiphospholipid syndrome | Arterial hypotension (pressure may be normal), fainting, shortness of breath, tachycardia |
Pre-medical first aid - algorithm of actions for anaphylactic shock
- Lay the patient on a flat surface, raise his legs (for example, place a blanket rolled up under them);
- Turn your head to one side to prevent aspiration of vomit, remove dentures from your mouth;
- Provide a flow of fresh air into the room (open a window, door);
- Take measures to stop the entry of the allergen into the victim’s body - remove the sting with poison, apply an ice pack to the bite or injection site, apply a pressure bandage above the bite site, and so on.
- Feel the patient's pulse: first on the wrist, if it is absent, then on the carotid or femoral arteries. If there is no pulse, begin performing indirect cardiac massage - clasp your hands and place them on the middle part of the sternum, apply rhythmic points 4-5 cm deep;
- Check if the patient is breathing: see if there are movements of the chest, apply a mirror to the patient’s mouth. If there is no breathing, it is recommended to begin artificial respiration by inhaling air into the patient’s mouth or nose through a napkin or handkerchief;
- Call an ambulance or transport the patient yourself to the nearest hospital.
Emergency care algorithm for anaphylactic shock (medical care)
- Monitoring vital functions - measuring blood pressure and pulse, determining oxygen saturation, electrocardiography.
- Ensuring airway patency - removing vomit from the mouth, removing the lower jaw using the triple Safar maneuver, tracheal intubation. In case of spasm of the glottis or Quincke's edema, it is recommended to perform a conicotomy (performed in emergency cases by a doctor or paramedic, the essence of the manipulation is to cut the larynx between the thyroid and cricoid cartilages to ensure air flow) or tracheotomy (performed only in a medical institution, the doctor dissects the tracheal rings ).
- Administration of adrenaline – 1 ml of 0.1% solution of adrenaline hydrochloride is diluted to 10 ml with saline solution. If there is a direct injection site for the allergen (bite site, injection site), it is advisable to inject it with diluted adrenaline subcutaneously. Then it is necessary to administer 3-5 ml of the solution intravenously or sublingually (under the root of the tongue, as it is abundantly supplied with blood). The remaining adrenaline solution must be injected into 200 ml of saline and continued intravenous drip under blood pressure control.
- Administration of glucocorticosteroids (hormones of the adrenal cortex) - dexamethasone at a dosage of 12-16 mg or prednisolone at a dosage of 90-12 mg is mainly used.
- Administration of antihistamines - first by injection, then switch to tablet forms (diphenhydramine, suprastin, tavegil).
- Inhalation of humidified 40% oxygen at a rate of 4-7 liters per minute.
- In case of severe respiratory failure, the administration of methylxanthines is indicated - 2.4% aminophylline 5-10 ml.
- Due to the redistribution of blood in the body and the development of acute vascular insufficiency, it is recommended to administer crystalloid (ringer, ringer-lactate, plasmalit, sterofundin) and colloid (gelofusin, neoplasmazhel) solutions.
- To prevent cerebral and pulmonary edema, diuretics are prescribed - furosemide, torasemide, minnitol.
- Anticonvulsants for the cerebral form of the disease - 25% magnesium sulfate 10-15 ml, tranquilizers (sibazon, relanium, seduxen), 20% sodium hydroxybutyrate (GHB) 10 ml.
First aid kit contents
Expert opinion
Makarov Igor Tarasovich
Hunter and fisherman with 20 years of experience. Wildlife lover
According to the standards, the packaging must contain drugs according to a certain list. It includes medications that help relieve the clinical manifestations of anaphylactic shock.
- Glucocorticosteroids. Prednisolone is most often included in the first aid kit. This is a potent anti-shock drug that can eliminate swelling and relieve allergy symptoms. It is used intravenously. The set should contain 10 ampoules.
- The styling should contain an antihistamine. It helps block histamine, which is a trigger for allergies. First aid kits are equipped with solutions for intramuscular and intravenous administration: Tavegil, Suprastin.
- To enhance the antihistamine effect, the above drugs are enhanced by the administration of Diphenhydramine. It not only helps relieve the manifestation of an allergic reaction, but also has a calming effect.
- To normalize cardiac activity, Adrenaline 0.1% is used. There should be 10 ampoules in the pack. The drug is used for intramuscular administration, as well as for local injection. Adrenaline has a vasoconstrictor effect. After its administration, heart function quickly normalizes.
- In anaphylactic shock, a spasm of the respiratory system occurs. Eufillin is used to dilate the bronchi. It helps saturate the blood with oxygen. The set should contain ten ampoules.
This is interesting: How to knit a straight knot: diagram
In addition to the basic composition, the anti-shock first aid kit should contain the following:
- syringes;
- cotton wool;
- bandages;
- alcohol wipes;
- alcohol;
- catheter for insertion into a vein;
- tourniquet;
- system for intravenous infusions;
- mask for artificial respiration;
- adhesive plaster.
The first aid kit should also contain saline solution, a blood pressure raising agent (usually supplied with caffeine), glucose solution, atropine, and gloves. The composition must contain at least two types of glucocorticosteroids.
Anaphylactic shock occurs for various reasons. It can be triggered by a reaction to medications, intolerance, to insect venom, snake bites, or animal bites. Often, a state of shock occurs as a reaction to food allergens, during a blood transfusion, or after a transplant.
The composition of a pharmacy is regulated by the SanPiN document. The law also regulates who should have a first aid kit.
Consequences of anaphylactic shock
Any disease does not go away without a trace, including anaphylactic shock. After relief of cardiovascular and respiratory failure, the patient may continue to have the following symptoms:
- Lethargy, lethargy, weakness, joint pain, muscle pain, fever, chills, shortness of breath, heart pain, as well as abdominal pain, vomiting and nausea.
- Prolonged hypotension (low blood pressure) is relieved by prolonged administration of vasopressors: adrenaline, mesaton, dopamine, norepinephrine.
- Pain in the heart due to ischemia of the heart muscle - administration of nitrates (isoket, nitroglycerin), antihypoxants (thiotriazoline, mexidol), cardiotrophics (riboxin, ATP) is recommended.
- Headache, decreased intellectual function due to prolonged cerebral hypoxia - nootropic drugs (piracetam, citicoline), vasoactive substances (Cavinton, ginko biloba, cinnarizine) are used;
- If infiltrates appear at the site of a bite or injection, local treatment is indicated - hormonal ointments (prednisolone, hydrocortisone), gels and ointments with a resolving effect (heparin ointment, troxevasin, lyoton).
Sometimes late complications occur after anaphylactic shock:
- hepatitis, allergic myocarditis, neuritis, glomerulonephritis, vestibulopathies, diffuse damage to the nervous system - which is the cause of death of the patient.
- 10-15 days after the shock, Quincke's edema, recurrent urticaria, and bronchial asthma may develop
- with repeated contact with allergenic drugs, diseases such as periarteritis nodosa, systemic lupus erythematosus.
Forms of development of anaphylaxis depending on the prevailing symptoms
Depending on which symptoms of anaphylactic shock predominate, several forms of the disease are distinguished:
- Typical . The first signs are skin manifestations, especially itching and swelling at the site of exposure to the allergen. Poor health and the appearance of headaches, causeless weakness, dizziness. The patient may experience severe anxiety and fear of death.
- Hemodynamic . A significant decrease in blood pressure without drug intervention leads to vascular collapse and cardiac arrest.
- Respiratory . Occurs when the allergen is directly inhaled with air flow. Manifestations begin with nasal congestion, hoarseness of the voice, then disturbances in inhalation and exhalation appear due to swelling of the larynx (this is the main cause of death in anaphylaxis).
- CNS lesions. The main symptoms are associated with dysfunction of the central nervous system, resulting in impaired consciousness, and in severe cases, generalized convulsions.
General principles for the prevention of anaphylactic shock
Primary prevention of shock
It involves preventing human contact with the allergen:
- elimination of bad habits (smoking, drug addiction, substance abuse);
- control over the quality production of medicines and medical devices;
- combating environmental pollution with chemical products;
- a ban on the use of certain food additives (tartrazine, bisulfites, agar-agar, glutamate);
- combating the simultaneous prescription of a large number of drugs by doctors.
Secondary prevention
Promotes early diagnosis and timely treatment of the disease:
- timely treatment of allergic rhinitis, atopic dermatitis, hay fever, eczema;
- conducting allergy tests to identify a specific allergen;
- careful collection of allergy history;
- indication of intolerable medications on the title page of the medical history or outpatient card in red ink;
- conducting sensitivity tests before intravenous or intramuscular administration of drugs;
- Observe patients after injection for at least half an hour.
Tertiary prevention
Prevents recurrence of the disease:
- maintaining personal hygiene rules
- Frequent cleaning of premises to remove house dust, mites, insects
- ventilation of premises
- removing excess upholstered furniture and toys from the apartment
- precise control of food intake
- use of sunglasses or a mask during the flowering period of plants
How can healthcare providers minimize the risk of shock in a patient?
To prevent anaphylactic shock, the main aspect is a carefully collected history of the patient’s life and illnesses. To minimize the risk of its development from taking medications, you should:
- Prescribe any drugs strictly according to indications, optimal dosage, taking into account tolerability and compatibility
- Do not administer multiple medications at the same time, only one drug. Once you are convinced of tolerability, you can prescribe the following
- The age of the patient should be taken into account, since daily and single doses of cardiac, neuroplegic, sedative, antihypertensive drugs for elderly people must be reduced by 2 times than doses for middle-aged patients
- When prescribing several medications that are similar in pharmaceutical form. action and chemical composition, take into account the risk of cross-allergic reactions. For example, if you are intolerant to promethazine, antihistamine derivatives of promethazine (diprazine and pipolfen) should not be prescribed; if you are allergic to procaine and anesthesin, there is a high risk of intolerance to sulfonamides.
- It is dangerous to prescribe penicillin antibiotics to patients with fungal diseases, since fungi and penicillin have common antigenic determinants.
- Antibiotics must be prescribed taking into account microbiological studies and determination of the sensitivity of microorganisms
- For antibiotic solvents, it is better to use saline or distilled water, since procaine often leads to allergic reactions
- Assess the functional state of the liver and kidneys
- Monitor the content of leukocytes and eosinophils in the blood of patients
- Before starting treatment, patients with a high risk of developing anaphylactic shock, 30 minutes and 3–5 days before the administration of the planned drug, are prescribed 2nd and 3rd generation antihistamines (Claritin, Semprex, Telfast), calcium supplements, and corticosteroids if indicated.
- To be able to apply a tourniquet above the injection site in case of shock, the first injection of the medication (1/10 of the dose, for antibiotics less than 10,000 units) should be administered into the upper 1/3 of the shoulder. If symptoms of intolerance occur, apply a tight tourniquet above the injection site until the pulse stops below the tourniquet, inject the injection site with adrenaline solution (9 ml of saline solution with 1 ml of 0.1% adrenaline), apply a heating pad with cold water to the injection area or cover with ice
- Treatment rooms should be equipped with anti-shock first aid kits and have tables with a list of medications that cause cross-allergic reactions with common antigenic determinants
- There should not be a room for patients with anaphylactic shock near the manipulation rooms, and also do not place patients with a history of shock in the rooms where patients are being administered drugs that cause allergies in the former.
- To avoid the occurrence of the Arthus-Sakharov phenomenon, the injection site should be monitored (skin itching, swelling, redness, and later, with repeated administration of medications, skin necrosis)
- For those patients who have suffered anaphylactic shock during hospital treatment, upon discharge, an o or “anaphylactic shock” is written in red pencil on the title page of the medical history.
- After discharge, patients with anaphylactic shock should be referred for medications to specialists at their place of residence, where they will be monitored at a dispensary and receive immunocorrective and hyposensitizing treatment.
Author:
Selezneva Valentina Anatolyevna physician-therapist
Who is at risk?
No one is immune from the development of anaphylaxis. It can start in anyone, but there are still those people for whom the risk of getting anaphylactic shock is much higher than others. These include people with a history of asthma (including bronchial asthma), eczema, urticaria, dermatitis, and allergic rhinitis.
Patients with mastocytosis are prone to similar allergic reactions. This is a disease in which there is a pathological proliferation of mast cells (immune cells of connective tissue) and their accumulation in tissues and bone marrow.
It is almost impossible to predict the possibility of developing anaphylactic shock. He is dangerous because of surprise. If a person has previously had anaphylactic shock, he must always have with him a card indicating the clinical picture of the shock he suffered, indicating allergens, and the results of the latest allergy tests.
You should pay attention to your well-being when taking previously untried medications, consuming unfamiliar and exotic food, visiting arboretums with unfamiliar flowering plants, and exercise caution when walking in nature, avoiding contact with insects, spiders and reptiles.
Anaphylactic (allergic) shock is rightfully considered the most dangerous manifestation of allergies. It is advisable for every person, even those without medical education, to know what to do in case of anaphylactic shock, since this can play a decisive role in saving their own life or the life of someone around them.
Allergic shock refers to the so-called immediate hypersensitivity reactions and develops in allergic people when any substance that has become an allergen for that person re-enters their body. Even knowing and clearly following the algorithm of actions for anaphylactic shock, it is not always possible to save the patient’s life, extremely severe pathological processes develop in his body so quickly.