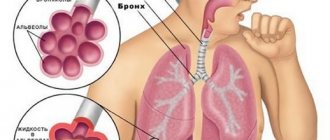
Pathologies of the respiratory system are among the most common diseases. The harmful effects of bad habits, polluted urban air and a sedentary lifestyle are serious risk factors for the breathing of modern people. The presence of pulmonary symptoms - prolonged cough, sputum discharge in the morning, shortness of breath, often perceived as normal, is often a sign of dangerous diseases. To identify and assess the severity of respiratory system disorders, special studies are carried out, which include spirometry. What kind of analysis this is is of interest to many patients who are prescribed this test. Spirometry allows you to assess lung capacity, inspiratory/expiratory speed, the degree of ventilation failure and obstruction.
General information
In medicine, various methods are known for studying the function of external respiration.
Such studies play an important role in a comprehensive examination of patients with diseases of the bronchi and lungs. Thanks to them, it is possible to determine the presence of respiratory failure in a patient long before the appearance of the first clinical symptoms. Modern medicine makes it possible to identify the nature, type, severity and dynamics of development of certain pathological changes, and to monitor the effectiveness of treatment. What is spirography and how is it performed? Spirography (spirometry) is a method for determining the function of external respiration, the main method for diagnosing and assessing the functional state of the lungs. The method is widely used in pulmonology and therapy and is considered the most informative.
What does it show?
What is spirometry in medicine and what does this study show? During the examination, the doctor determines the following indicators:
- the volume of inhaled and exhaled air – tidal volume of the lungs;
- vital capacity of the lungs - the maximum amount of air that the patient can breathe deeply;
- forced vital capacity of the lungs - the difference in volumes at the very beginning and at the end of a full exhalation;
- functional residual capacity - the remaining air after a quiet exhalation;
- residual volume after maximum expiration;
- total capacity;
- forced expiratory volume in the first second of forced expiration;
- peak volumetric velocity;
- instantaneous volumetric velocity;
- minute volume of breathing;
- maximum ventilation of the lungs.
With the help of a spirograph, it is possible to obtain the most reliable and informative results and, accordingly, carry out an accurate diagnosis.
Computer spirometry can reveal:
- airway obstruction;
- the severity of a particular disease;
- symptoms of COPD and bronchial asthma ;
- hidden bronchospasm ;
- optimal treatment tactics;
- the effectiveness of current therapy over time.
Other testing methods
Spirometry is the simplest and most widely used pulmonary function test, but other diagnostic modalities may be required for a definitive diagnosis.
The diffusion capacity of the lungs determines how well oxygen enters the blood from inhaled air, using a mixture containing 0.3% carbon monoxide (CO). The amount of CO remaining in the exhaled air indicates how well a person can absorb the gas. The breathing performed in this test is less intense than in a spirometry test, but may take longer.
A blood test determines the level of hemoglobin it contains. Hemoglobin is responsible for the absorption of oxygen.
Pulse oximetry assesses the level of oxygen in the blood using a sensor that is placed on the surface of the skin.
An arterial blood gas test determines the levels of oxygen and carbon dioxide in the blood.
Measuring exhaled nitric oxide (NO) levels determines how much nitric oxide is in a person's exhaled air.
Chest X-rays and CT scans of the chest are used to examine the lungs and diagnose certain conditions.
Indications
This method is actively used in therapy and pulmonology for the following indications:
- long-lasting, lingering cough for no reason, for 3-4 weeks or more, often after a cold, acute respiratory viral infection or bronchitis ;
- feeling of pressure and “stuffiness” in the chest, shortness of breath ;
- if the patient has difficulty inhaling and exhaling;
- “wheezing” or “wheezing” breathing when inhaling;
- long-term smoking experience;
- the patient suffers from frequent exacerbations of bronchitis , shortness of breath , and lacks air;
- with a family history, if there are relatives with diseases of the respiratory system and allergic diseases;
- it is necessary to adjust the treatment of bronchial asthma ;
- work in hazardous production.
Important data for the development of further treatment tactics can be obtained by taking a spirogram for bronchial asthma , chronic obstructive pulmonary disease , after and during various medical procedures.
Normal indicators
Spirography indicators for a pulmonologist are the main parameter for making an accurate diagnosis. The data obtained have a direct correlation with the physiological parameters of the human body (weight, height, gender).
The table of normal spirometry readings and deviations is as follows:
| Indicators | Norm | Acceptable rate | Deviations | ||
| Moderate | Significant | Sharp | |||
| vital capacity | >90 | 85-89 | 70-84 | 50-69 | <50 |
| FEV1 | >85 | 75-84 | 55-74 | 35-54 | <35 |
| FEV1/FVC | >70 | 65-69 | 55-64 | 40-54 | <40 |
| OOL | 90-125 | 126-140 85-89 | 141-175 70-84 | 176-225 50-69 | >225 <50 |
| OEL | 90-110 | 110-115 85-89 | 116-125 75-84 | 126-140 60-74 | >140 <60 |
| OOL/OEL | <105 | 105-108 | 109-115 | 116-125 | >125 |
Correctly interpreted spirometry results will help prevent complications of pathological processes and identify respiratory diseases at an early stage of development.
Contraindications
The list of contraindications for this study is quite small. But, nevertheless, spirography should not be performed:
- after a recent heart attack or stroke ;
- for aortic aneurysm , hypertension ;
- patients with pneumothorax , bleeding ;
- if the patient has recently undergone surgery on the chest or abdomen;
- in acute heart failure .
Spirometry is included in the list of mandatory preventive examinations that must be performed annually.
What affects the reliability of the result?
Spirometry shows incorrect results if medical recommendations have been violated. The accuracy of the parameters also depends on the serviceability of the device.
The reliability of the data obtained is affected by the following features:
- the person inhaled prematurely;
- the mouthpiece was loosely clamped, so an air trap occurred;
- the patient exhaled quickly;
- the person has excessively clamped his lips and teeth;
- there was a short exhalation;
- During the examination, emotional instability was observed in the patient;
- there was no maximum effort during exhalation;
- During the research, the person was bothered by a strong cough;
- air was exhaled through the nose.
Incorrect results require careful diagnosis, since incorrect data can prevent an accurate diagnosis and the most effective treatment.
Preparing for the study
The results may be significantly affected by several factors that cannot be ignored.
The examination is carried out in the morning, on an empty stomach. At least 6-8 hours should pass after the last meal. It is acceptable to drink some warm water and eat one light cracker. On the day of the study, you should not smoke or drink strong tea or coffee.
Before starting, it is not recommended to carry out medical procedures or morning exercises. It is better to wear clothes that are loose and do not restrict your chest. Before spirometry, it is better to sit quietly for 20 minutes.
You should also take a break from taking certain medications. For example, bronchodilators:
- Salbutamol , Berodual , Ventolina - 6 hours;
- Seretide , Symbicort , Foster , Serevent , Foradil and the drug Oxis - 12 hours;
- long-acting theophyllines ( Spiriva ) – per day.
Price
The price of spirometry ranges from 1000-2300 rubles. and depends on the center where the research is performed. The procedure is widespread and is often used for research in pulmonology.
The cost of spirography in government institutions is lower, but the examination period may take some time. The price of the study is also affected by the need to carry out the procedure with additional medications (with samples).
The normal functioning of the human body depends on its saturation with oxygen. This function is assigned to the organs of the respiratory system. With the development of certain pathological processes, external respiration fails. Spirometry helps identify abnormalities.
The results are compared with normal values in the table and an accurate diagnosis is established. The data obtained is also necessary for drawing up an effective treatment regimen.
How is spirometry performed?
Before digital technology became widespread, doctors used mechanical spirometers , usually water ones. In the research apparatus, the air exhaled by the patient penetrated into a cylinder located in a vessel with water. During exhalation, the cylinder moved upward and the recording device connected to it left a graph on the moving paper. The graph showed the change in volume over time. Unfortunately, examinations using this type of instrument were quite labor-intensive and required additional manual calculation of the necessary parameters.
Types of modern digital spirometers
Now digital devices for studying respiratory function are widely used - digital spirometers , spirographs . The device records patient data in the modes of quiet breathing, maximum ventilation and forced exhalation. They also carry out various functional tests, with bronchodilators , provocative tests, and so on.
How is spirography performed? The doctor or specialist conducting the study usually uses additional programs that facilitate the calculation of the necessary parameters. Data on the patient’s weight, height and age, concomitant chronic diseases and medications taken may be needed.
After spirometry itself, a table is calculated with individual indicators for the patient, the values of the necessary parameters and a graphical representation of the air flow - spirogram . If there are irregularities in the spirogram, the doctor may prescribe additional examinations. For example, with the use of bronchodilators . The procedure is quite comfortable and painless.
Methodology:
- the patient, pressing his lips tightly to the mouthpiece of the spirograph, breathes calmly for 10 seconds;
- the doctor commands when you need to inhale as deeply as possible so that the lungs are filled with air as much as possible;
- the patient exhales with maximum force into the sensor tube.
Spirometry procedure
During the procedure the following steps are performed:
A clip is placed on the nose to close the nostrils.
The person inhales as much air as he can through his mouth.
The lips are sealed tightly around the tube.
The person breathes quickly and forcefully into the tube for several seconds.
The test is usually repeated at least three times to ensure an accurate result. The highest scores are usually used as the final result.
The doctor may prescribe a bronchodilator, which is inhaled, and then the test is performed again. This will measure the effect of the bronchodilator on a person's ability to breathe.
Decoding the results of spirography
The doctor deciphers the results of spirometry, makes a diagnosis, gives recommendations for treatment and further examinations.
During decoding of the lung spirogram, the specialist determines the key values necessary for making a diagnosis. The graph below shows a forced expiratory spirogram with key parameters:
- FVC – forced vital capacity;
- FEV1 – forced expiratory volume in 1 second;
- SOS25-75 is the average speed of the forced expiratory flow, corresponding to 25 - 75% FVC.
Forced expiratory spirogram
Some indicators of spirometry norm:
- RR is the frequency of respiratory movements that the patient performed within a minute. Normally - from 16 to 18 units.
- MOD - breathing volume per minute. All the air that passed through the patient's lungs within a minute. Depends on many factors.
- DO - tidal volume. The entire air mass that enters the lung tissue during one normal breath. Normally - from 500 to 800 ml.
- SOS - average volumetric velocity. The rate of forced expiration in the middle of the respiratory movement. With its help, obstructive pathologies are determined.
Below is a table of normal spirometry readings. It should be noted that the assessment of the results of this functional study is carried out by a specialist and must contain accurate data, be concise and informative. In addition to the usual statement of facts that certain indicators are normal and these are not, the result of the study should take into account the principles of clinical decision-making, where the probability of disease after the study is calculated taking into account the probability of disease before the study. The quality of the procedure performed, the probability of false-negative and -positive interpretation, the accuracy of the results and key values are also taken into account.
| Options | Designations | Normal value | Units | |
| Men | Women | |||
| Total lung capacity | TLC | 7,0 | 6,2 | l |
| Vital capacity of the lungs | V.C. | 5,6 | 5,0 | l |
| Forced vital capacity | FVC | 5,6 | 5,0 | l |
| Residual volume | RV | 1,4 | 1,2 | l |
| Functional residual capacity | FRC | 3,2 | 2,8 | l |
| One second capacity | FEV1 | 4,5 | 4,0 | l |
| Maximum expiratory forces of respiratory flow | V*Emax | 10 | l/s | |
| Respiratory limit value (at a frequency of 1/min) | 110 | 100 | l/min | |
| Compliance of breathing apparatus (lungs + chest) | CTl+Th | 1,3 | l/k Pa-1 | |
| Compliance of the chest | CTh | 2,6 | l/k Pa-1 | |
| Compliance of the lungs | CTl | 2,6 | l/k Pa-1 | |
| Airway resistance | R.L. | 0,13 | kPa/l*s | |
The flow-volume loop, the graph of which is shown below, also has an important diagnostic value after spirometry. The vertical axis shows the flow velocity, and the horizontal axis shows the lung volume. Modern spirometers build it automatically.
Normal view of a flow-volume loop
Spirometry: patient sensations
Most often, patients tolerate spirometry well. They do not have any discomfort or pain. In rare cases, a test using a bronchodilator is accompanied by a feeling of palpitations and slight trembling in the upper and lower extremities. This should not be a cause for concern, since this condition is temporary and not dangerous to the patient's health.
In extremely rare situations, reactions such as a coughing attack or bronchospasm may occur, as a result of which further spirometry must be stopped and medical assistance provided to the patient.
Reviews
Reviews from patients who completed this study are generally good. They note that spirometry is highly informative; the procedure is not expensive, but at the same time simple and financially accessible.
- “... I went through this procedure before, during and after treatment. Each time it was clearly visible on the graph what was wrong and what was changing for the better. I did it once using Salbutamol. But, unfortunately, I was allergic to it. And the procedure itself is simple and useful.”
- “...My daughter was examined. The procedure is necessary, it is easy to undergo, does not harm the body in any way and is cheap, the result is immediately obvious. However, problems arose with the fact that my daughter coughed and could not always accurately follow the doctor’s commands. But we seem to have managed it."
- “... Spirometry was performed several times during the prof. examinations during study. Sometimes I retook the tests several times, but in the end everything turned out to be normal.”
The feasibility of studying the lungs with a bronchodilator
Spirometry (the table describes normal values to compare test results and make an accurate diagnosis) with a bronchodilator allows you to assess the state of the respiratory process before and after using the drug. This type of examination is carried out for bronchitis or bronchial asthma.
The likelihood that hidden bronchospasm will go unnoticed is reduced. Its presence is evidenced by changing readings obtained after a standard procedure.
Examination for young patients
Testing is not recommended for children under 5 years of age. Children are likely to receive unreliable spirogram data: the acquired skills do not allow them to correctly perform the necessary breathing maneuvers.
From the age of 9, a full examination is possible along with adults. Young patients should be diagnosed in specialized institutions for children.
Creating a relaxed atmosphere is the key to successful spirometry. A worker with a pedagogical approach and the use of a playful form has greater authority in the eyes of the child and will be able to carry out the procedure most effectively.