January 14, 2021
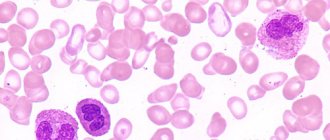
Hello, dear readers of the KtoNaNovenkogo.ru blog. People with a normally functioning circulatory system can be easily distinguished from the general crowd.
It is the coordinated functioning and the necessary balance of all the numerous components that make up the blood that provide a person with an excellent mood, vigor, activity, fullness of strength and energy.
Let's consider the features of platelets, which are one of the three main formed components in the blood - why it needs them and what their imbalance can lead to.
The role of platelets in the body
The main functions of red blood cells are as follows:
- Providing primary hemostasis. As soon as there is a violation of the anatomical integrity of the body’s tissues and blood vessels, these structures, as a result of a complex process, are concentrated in the affected area. Adhesion (sticking) begins, and then aggregation (clumping).
A primary plug is created, which becomes a kind of valve that prevents blood from leaving the vessel. This is the main mechanism for the primary stop of the pathological process.
However, it is not permanent; purely physical measures to prevent the release of blood are not enough in such a volume. Another mechanism is also involved.
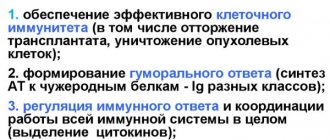
- The so-called secondary hemostasis. Provides active release and stimulation of the synthesis of special substances called coagulation factors. This includes several connections that share basic functionality.
The production of such leads to rapid blood clotting and restoration of normal functioning of the body. In this case, hemodynamics (blood flow) is not disturbed, the process is balanced by the anticoagulative (anti-clotting) effect of other substances. Therefore, the blood remains liquid, despite all the changes that occur.
- The third function concerns ensuring the normal condition of blood vessels. Platelets in some way determine the stable state of the endothelium - the inner lining of capillaries, veins and arteries.
Objectively, when solving this problem, the permeability of the blood supply structures is reduced in order to avoid the spontaneous formation of hematomas, including large ones. This function is carried out in parallel with others.
Platelets play a role in hemostasis and indirectly affect the condition of blood vessels, the speed and quality of nutrition of all body tissues. If at least one function is disrupted, significant distortions begin in the activity of all blood systems.
Also, deviations in laboratory parameters are detected almost immediately, as the body tries to compensate for functional disorders.
There is also a plus here, since diseases quickly make themselves known with changes that are easy to track.
Basic laboratory tests for blood clotting
Norms of coagulogram indicators
The process of blood clotting can begin with damage to the surface of the endothelium (vascular wall), then the internal mechanism of prothrombinase formation occurs. Coagulation can also be triggered by blood contact with tissue thromboplastin, which is hidden in the tissue cell if the membrane is intact. But it comes out when the vessel is damaged (an external mechanism for the formation of prothrombinase). The launch of one or another mechanism explains the fact that the clotting time of a capillary blood sample (external path) is 2-3 times less than that of a venous blood sample (internal path).
Laboratory tests based on these mechanisms are used to determine the time required for blood clotting. The Lee-White coagulation study is carried out by collecting blood into two test tubes from a vein, while the formation of prothrombinase along the external pathway is studied according to Sukharev (blood from a finger) . This blood clotting test is quite simple to perform. In addition, it does not require special preparation (it is taken on an empty stomach) and a lot of time to produce, because capillary blood (as mentioned above) coagulates 2-3 times faster than venous blood. The normal blood clotting time according to Sukharev is from 2 to 5 minutes. If the time of clot formation is shortened, it means that there is an accelerated formation of prothrombinase in the body. This happens in the following cases:
- After massive blood loss, to which the coagulation system responds with hypercoagulation;
- DIC syndrome in stage 1;
- Negative effects of oral contraceptives.
Delayed formation of prothrombinase will be expressed by prolongation of clot formation time and observed under certain conditions:
- Deep deficiency of factors I, VIII, IX, XII;
- Hereditary coagulopathies;
- Liver damage;
- Treatment with anticoagulants (heparin).
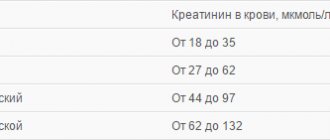
Tables of platelet norms according to age
The normal platelet count in the blood is 100-400 x10^9/l. both for women and for men, but the values are conditional, deviations up or down are possible, depending on the specific situation. They are determined, among other things, by gender, age and the current state of human health; hormonal phenomena, such as gestation, also have a huge impact.
Among women
| Age (years) | Levels in units per liter |
| 12-16 | 100-250 |
| 17-25 | 170-380 |
| 27-36 | 170-400 |
| 37- 60 | 170-350 |
| After 60 years | 170-310 |
During pregnancy
| Trimester | Norm |
| 1 | 170-340 |
| 2 | 150-320 |
| 3 | 140-310 |
In men
| Age | Normal level (U/l) |
| 12-16 | 100-260 |
| 17-25 | 120-270 |
| 26-45 | 190-400 |
| After 45 | 190-380 |
In children
| Age | Norms (Unit/l) |
| Birth | 270-300 |
| Up to 12 months | 280-300 |
| 2-3 years | 280-290 |
| 4-5 years | 280-290 |
| 6-8 years | 270-290 |
| 8-12 years | 170-270 |
| 13-18 years old | 100-260 (depending on gender and general health, some other factors) |
Platelets in a blood test are designated as PLT; indicators should be looked for in this column.
In any case, interpretation of diagnostic results is carried out not by the patients themselves, but by hematology specialists.
It should be taken into account that counting methods vary in individual laboratories. Therefore, it is possible to say whether platelets in the blood are normal or not after studying the reference indicators.
Also, when assessing the diagnostic results, the patient’s age, gender, and health status are taken into account. Clinicians and laboratory workers themselves do not do this; they produce a generalized result that must be assessed with a professional eye.
How is their level determined?
Let us immediately note that, as such, there is no separate analysis for the determination of platelet plates.
An assessment of their functions and condition is carried out in conjunction with a general analysis of the blood clinic, displaying the result with the abbreviation - PLT (mandatory indicator) and the measurement of thrombocrit - PCT (the level of their concentration in the total volume of blood).
This analysis does not take into account the ratio of age groups and platelet forms (irritation and degeneration).
A more detailed analysis of platelet properties is determined in certain conditions (before surgery, during bleeding, and other critical conditions) by the hemostasiogram (coagulogram) method using screening tests that determine the consistency of the hemostasis process.
Reasons for increasing PLT
There are many factors that increase platelet levels, if we talk about the most common ones:
- Neoplasms in the patient's body. Tumors of various origins. Whether they are malignant or, much less commonly, benign. Especially when the process of decay begins. Bleeding is detected. Or during germination of the walls of organs and tissues, with the development of destruction of large vessels. The question remains open; the patient needs to be examined.
- Iron-deficiency anemia. It occurs frequently and is accompanied by a decrease in the amount of hemoglobin due to a lack of this element in the body. Recovery in nutritional form is usually not difficult. In any case, it is necessary to urgently treat the person so as not to provoke dangerous complications.
- Disorders of the digestive tract. Stomach, liver, other structures. It is necessary to start treatment as quickly as possible. In particularly difficult situations, such as cancer, cirrhosis, hepatitis, the participation of a whole group of specialists will be required, and success is not guaranteed.
- Infectious lesions of the body by viruses, fungi or bacterial agents provoke an increase in platelet synthesis and carry an equally high danger. With quality therapy, the problem can be completely eliminated. In such a situation, the disorder is temporary, transient.
- Inflammatory phenomena. Infectious most often, but not only. The other type is non-septic changes. These include autoimmune diseases. There are many options here. From joint damage - rheumatoid arthritis, to systemic lupus erythematosus, generalized or localized vasculitis, and other forms of the pathological process. In all cases, the level of platelets is higher than normal, within varying limits, while in parallel the content of CRP and C-reactive protein increases, which is used as a verification sign.
- Congenital abnormalities in the development of connective tissue. These are usually genetically determined disorders. They are difficult to correct, and therefore a high-quality restoration of platelet concentration is not always possible. It all depends on the specific clinical case and the qualifications of the doctors involved in providing care.
These reasons are the culprits in adults and children equally often.
If platelets are elevated, there is a high probability of hypercoagulation and clot formation, which is extremely dangerous. Because it can cause fatal complications. It's a matter of time, the probability is growing every month, if not every day.
Reasons for the decline in indicators
There are even more of them. The vast majority of factors reducing platelet levels are pathological.
Among them:
- Heart attack. Acute circulatory disorder in the heart muscle, myocardium. It is accompanied not only by obvious symptoms of the disorder, but also by changes in laboratory parameters.
As a rule, restoration of adequate platelet numbers occurs much later. We are talking about weeks or even more.
However, the indicator is not informative for diagnosing and studying the dynamics of recovery. Therefore, we are talking about an accompanying change that has little effect on the processes in the body.
- Tumors. As in the previous case, both malignant neoplasms and benign structures. At the initial stages of the pathological process, there are no deviations in the blood picture. The rate of disease progression can be assessed by the level of formed cells.
- Iron-deficiency anemia. Insufficient intake of iron into the human body. Occurs for various reasons. It is significant that against the background of IDA, the platelet content in the blood can either increase or decrease.
The question remains open. It all depends on the individual characteristics of the patient’s body. Based on changes in laboratory tests, it is possible to assess the dynamics of the pathological process.
- Liver pathologies. Hepatitis, regardless of its origin, cirrhosis, cancer processes. Organ dysfunctions are accompanied by chain changes that ultimately affect the nature and quality of hemostasis in the body of patients.
- Kidney diseases. Insufficiency, all kinds of nephropathies and other disorders, including those of an inflammatory nature, pyelonephritis, glomerulonephritis and others cause low platelet levels.
- Problems with the thyroid gland.
- Hyperlipidemia. Increased levels of fatty compounds: cholesterol and others. It is indirectly manifested by atherosclerosis, which, although does not cause a decrease in platelet concentration, does indicate the development of metabolic problems. Diagnostics sometimes requires movement along such a complex chain.
- Helminthic lesions. Infestations, regardless of the type of parasite and its location.
There are also natural factors of platelet changes:
- Pregnancy. Gestation itself affects the level of formed cells; deviations are possible both larger and smaller. Each situation is assessed individually.
- Postponed birth. Some time after the complex resolution of the process, a drop in platelet levels is observed. This is a temporary and usually non-threatening condition.
- Hormonal changes. The menstrual cycle, puberty (puberty), transition to menopause in men and women - platelets are below normal throughout the entire peak period.
- Taking certain medications. Typically, the change in the concentration of formed cells is not so great as to provoke consequences dangerous to health or life. To find out about the possibility of such a side effect, it is recommended to refer to the annotation. Such factors are always indicated in the instructions for the medication.
The causes of low platelet levels are mainly pathological; they are determined during diagnosis; based on the results, we can talk about the need for treatment or the lack thereof.
Thrombocytosis in pregnant women
The options described above also apply to pregnant women, but several more factors are added that affect the increase in platelets.
- Antiphospholipid syndrome is an autoimmune abnormality associated with intense thrombus formation, and during pregnancy this risk increases many times over.
- Toxicosis in pregnant women is characterized by nausea, vomiting, and bloating. Dehydration and insufficient fluid intake against the background of dyspeptic symptoms provoke thrombocythemia.
A significant increase in the level of blood platelets worsens the course of pregnancy until it fails. The deadline does not matter at all.
Additional examinations
A general blood test alone is not enough to determine the essence of the problem. Auxiliary techniques are used.
- Oral questioning of the patient. To identify the main health complaints, which are not always present. Symptoms are systematized and used to accurately determine the nature of the process and put forward hypotheses.
- Anamnesis collection. Investigation of factors that could potentially be responsible for changes in platelet levels.
- Coagulogram. Assessment of blood coagulation rate. An informative technique that indirectly indicates the condition and number of formed cells. Used as one of the main examination methods.
- Ultrasound of the abdominal organs. To identify pathologies of the digestive tract.
- Testing for tuberculosis. Sputum delivery. Often mycobacteria provoke abnormalities in platelet counts.
- Chest X-ray. Review methodology.
- In extreme cases, a bone marrow puncture is required, as well as a histological evaluation of the results obtained and a tissue sample.
All activities are carried out under the supervision of a doctor.
Treatment
Therapy depends on the form of the process that provokes laboratory abnormalities. In any case, the main task is to correct the root cause. The concentration of formed cells normalizes itself as soon as the key problem is solved.
With elevated platelets
There are many options:
- Anemia. It can be eliminated by administering iron supplements or correcting disorders of the digestive tract. The duration of therapy is up to six months, depending on the complexity.
- Tumors require surgical removal. Then, according to indications, radiotherapy and chemotherapy are prescribed.
- Infectious processes. For them, antibiotics (bacterial lesions), stimulators of interferon production or ready-made antibodies (viruses), specialized fungicides (fungi) are indicated. It is also possible to use anti-inflammatory and antipyretic medications. This is a symptomatic correction.
- Diseases of the digestive tract are eliminated depending on the form. Various drugs are used; surgery is usually not required. A certain diet is also prescribed.
At lower values
- Liver diseases are treated based on the essence of the changes. Hepatitis requires systematic use of medications, including hepatoprotectors (Essentiale, Karsil), to prevent further destruction of the organ.
Cirrhosis requires identical therapy. In difficult cases, transplantation is required. It is possible as long as platelet functions are still performed.
Attention:
Once bleeding begins, transplantation is no longer possible. The patient simply will not survive the operation.
- Kidney pathologies. They also require the use of medications. Which ones depend on the case. In extreme, advanced situations, artificial blood purification is carried out through hemodialysis.
- Non-infectious, autoimmune inflammatory processes require the use of glucocorticoids. For example, Prednisolone or the much more powerful Dexamethasone. The question remains at the discretion of specialists. If the drugs are ineffective, immunosuppressants are used to suppress the intensity of the body’s false response.
The issue of therapy is decided according to the situation. There are many options, each of them is worthy of consideration, which could become the topic of a separate article.