Dilaprel
Active substance:
Ramipril*
Pharmgroup:
ACE inhibitors
Analogs for the active substance:Amprilan Vasolong Corpril Pyramid Ramigamma Ramipril Tritace Hartil | Application area:Sudden increase in blood pressure Hypertensive circulatory disorder Hypertensive state Hypertensive crises Hypertension Arterial hypertension Hypertension is malignant Essential hypertension Hypertonic disease Hypertensive crises Hypertensive crisis Decompensated chronic heart failure Diabetic nephropathy Diabetic nephropathy due to type 1 diabetes mellitus Diabetic nephropathy in patients with type I diabetes Kidney diseases Congestive circulatory failure Congestive heart failure with high afterload Congestive chronic heart failure Malignant hypertension Malignant hypertension Malignant hypertension Changes in liver function in heart failure Isolated systolic hypertension Isolated systolic hypertension Cardiomyopathy with severe chronic heart failure Compensated chronic heart failure Hypertensive crisis Hypertensive crisis Megaloureter Impaired renal blood flow Ureteral dysfunction Renal dysfunction Renal dysfunction Nondiabetic nephropathy Insufficiency of renal excretory function Nephrogenic osteopathy Nephropathic syndrome Diabetic nephropathy Minimal change nephropathy Exacerbation of hypertension Swelling due to circulatory failure Edema of cardiac origin Cardiac edema Edema syndrome in heart diseases Edema syndrome in congestive heart failure Edema syndrome in heart failure Edema syndrome in heart failure or cirrhosis of the liver Primary arterial hypertension Maintaining kidney function Right ventricular failure Proteinuria in patients with type 2 diabetes mellitus Renovascular diseases Congestive heart failure Congestive heart failure Heart failure with low cardiac output Chronic heart failure Cardiac edema Transient arterial hypertension Chronic decompensated heart failure Chronic congestive heart failure Chronic heart failure Chronic kidney disease Essential arterial hypertension Essential arterial hypertension Essential hypertension Essential hypertension |
Dilaprel plus
Patients with previous diuretic therapy
If possible, it is necessary to discontinue diuretics 2-3 days (depending on the duration of their action) before starting treatment with DILAPREL® PLUS or at least reduce the dose of diuretics taken. Treatment should begin with taking 1 capsule. with a dosage of 0.625 mg + 2.5 mg 1 time per day in the morning. After taking the first dose and after increasing the dose of DILAPREL® PLUS, patients should be under medical supervision for at least 8 hours to avoid an uncontrolled hypotensive reaction.
IHD and cerebrovascular insufficiency
The risk of arterial hypotension exists in all patients, however, in patients with coronary artery disease and cerebrovascular insufficiency, special caution should be exercised when treated with DILAPREL® PLUS. Treatment should begin with a daily dose of 0.625 mg + 2.5 mg (initial dose).
Renal dysfunction
Therapy with DILAPREL® PLUS is contraindicated in patients with severe renal failure (creatinine clearance less than 30 ml/min). In some patients with arterial hypertension without previous renal impairment, symptoms of acute renal failure may appear during therapy with DILAPREL® PLUS. In this case, treatment with DILAPREL® PLUS should be discontinued. In the future, you can resume combination therapy using low doses of DILAPREL® PLUS, or use indapamide and ramipril in monotherapy. Such patients require regular monitoring of potassium levels and creatinine concentrations in the blood plasma every 2 weeks after the start of therapy and every subsequent 2 months of therapy with DILAPREL® PLUS.
Acute renal failure often develops in patients with severe CHF or underlying renal impairment, incl. with bilateral renal artery stenosis or stenosis of the artery of a single functioning kidney. Taking DILAPREL® PLUS is contraindicated in patients with bilateral renal artery stenosis or stenosis of the artery of a single functioning kidney.
Arterial hypotension and water-electrolyte imbalance
Before starting treatment with DILAPREL® PLUS, it is necessary to eliminate hyponatremia and hypovolemia. Hyponatremia is associated with a risk of a sudden decrease in blood pressure (especially in patients with bilateral renal artery stenosis or arterial stenosis of a single functioning kidney). Therefore, during dynamic monitoring of patients, attention should be paid to possible symptoms of dehydration and decreased electrolyte levels in the blood plasma, for example after prolonged diarrhea or vomiting. Such patients require regular monitoring of blood plasma electrolyte levels. With a pronounced decrease in blood pressure, intravenous administration of 0.9% sodium chloride solution may be required.
Transient arterial hypotension is not a contraindication for continued therapy. After restoration of blood volume and blood pressure, you can resume therapy with DILAPREL® PLUS, using low doses of the drug, or use indapamide and ramipril in monotherapy.
Potassium content
The combined use of indapamide and ramipril may lead to the development of hypokalemia, especially in patients with diabetes mellitus or renal failure. While taking DILAPREL® PLUS, it is necessary to regularly monitor the potassium content in the blood plasma. In patients with hypokalemia, the use of DILAPREL® PLUS is contraindicated.
Excipients
It should be taken into account that the excipients of the drug DILAPREL® PLUS include lactose monohydrate. The use of DILAPREL® PLUS is contraindicated in patients with lactose intolerance, lactase deficiency, and glucose-galactose malabsorption.
Indapamide
Liver dysfunction
When using thiazide and thiazide-like diuretics in patients with impaired liver function, hepatic encephalopathy may develop, especially in case of water-electrolyte imbalance. In this case, you should immediately stop taking DILAPREL® PLUS.
Photosensitivity
Cases of photosensitivity reactions have been reported while taking thiazide and thiazide-like diuretics. If photosensitivity reactions develop while taking DILAPREL® PLUS, treatment should be discontinued. If it is necessary to continue therapy with DILAPREL® PLUS, it is recommended to protect exposed skin from direct exposure to sunlight and artificial UV rays.
Sodium content in blood plasma
Before starting treatment, it is necessary to determine the sodium content in the blood plasma. While taking the drug, this indicator should be regularly monitored. All diuretic drugs can cause hyponatremia, sometimes leading to extremely serious consequences. Regular monitoring of sodium levels is necessary because Initially, a decrease in sodium content in the blood plasma may not be accompanied by the appearance of pathological symptoms. The most careful monitoring of sodium levels is indicated in patients with cirrhosis and elderly patients.
Potassium content in blood plasma
Therapy with thiazide and thiazide-like diuretics is associated with a risk of hypokalemia (plasma potassium levels below 3.4 mmol/l) in the following categories of patients: elderly patients, debilitated patients, or those receiving concomitant drug therapy with other antiarrhythmic drugs and drugs that can prolong the interval QT, patients with liver cirrhosis, peripheral edema or ascites, coronary artery disease, heart failure. Hypokalemia in such patients increases the toxic effect of cardiac glycosides and increases the risk of developing arrhythmias.
In addition, patients with an increased QT interval on the ECG are at increased risk, and it does not matter whether this increase is caused by congenital causes or the effect of drugs.
Hypokalemia, like bradycardia, is a condition that contributes to the development of severe arrhythmias and especially arrhythmias, which can be fatal. In all the cases described above, it is necessary to regularly monitor the potassium content in the blood plasma. The first measurement of potassium content in the blood plasma should be carried out within the first week from the start of therapy with DILAPREL® PLUS.
If hypokalemia is detected, appropriate treatment should be prescribed.
Calcium content in blood plasma
Thiazide and thiazide-like diuretics reduce the excretion of calcium by the kidneys, leading to a slight and temporary increase in calcium levels in the blood plasma. Severe hypercalcemia may be a consequence of latent hyperparathyroidism.
You should stop taking DILAPREL® PLUS before testing the function of the parathyroid glands.
Plasma glucose concentration
It is necessary to monitor plasma glucose concentrations in patients with diabetes mellitus, especially in the presence of hypokalemia.
Uric acid
Patients with elevated plasma uric acid concentrations do not have an increased risk of developing gout. In patients with gout, the frequency of attacks may increase or the course of gout may worsen.
Diuretics and kidney function
Thiazide and thiazide-like diuretics are fully effective only in patients with normal or slightly impaired renal function (plasma creatinine concentration in adults below 25 mg/l or 220 µmol/l). In elderly patients, normal plasma creatinine concentrations are calculated taking into account age, body weight and gender.
It should be taken into account that at the beginning of treatment, patients may experience a decrease in the rate of CF due to hypovolemia, which, in turn, is caused by the loss of fluid and sodium ions while taking diuretic drugs. As a result, the concentration of urea and creatinine in the blood plasma may increase. If renal function is not impaired, such temporary functional renal failure, as a rule, passes without consequences, however, with existing renal failure, the patient's condition may worsen.
Athletes
Indapamide may give a positive result during doping control.
Ramipril
Neutropenia/agranulocytosis
In patients taking ACE inhibitors, cases of neutropenia/agranulocytosis may develop. The risk of developing neutropenia is dose-dependent and depends on the drug taken and the presence of concomitant diseases. In patients with normal renal function in the absence of other complications, neutropenia rarely develops and resolves spontaneously after discontinuation of ACE inhibitors. Particular caution must be observed in patients with systemic connective tissue diseases (including systemic lupus erythematosus, scleroderma), as well as during therapy with immunosuppressants, allopurinol or procainamide, especially with existing renal dysfunction. Such patients may develop a severe infection that does not respond to intensive antibiotic therapy. It is recommended to periodically monitor the number of leukocytes in the blood. The patient should be warned that if any signs of an infectious disease appear (sore throat, fever), consult a doctor immediately.
Angioedema (Quincke's edema)
In rare cases, during therapy with ACE inhibitors, angioedema of the face, extremities, lips, tongue, uvula, pharynx and/or larynx may develop. If these symptoms appear, you should immediately stop taking DILAPREL® PLUS. The patient's condition should be monitored until signs of edema disappear completely. If the swelling affects only the face and lips, its manifestations usually go away without special treatment, however, antihistamines can be used to more quickly relieve symptoms.
Angioedema, accompanied by swelling of the tongue, pharynx and/or larynx, can lead to airway obstruction and death. In this case, you should immediately administer epinephrine (adrenaline) subcutaneously at a dose of 1:1000 (0.3 to 0.5 ml) and/or ensure airway patency. In the future, such patients should not be treated with ACE inhibitors. Patients with a history of angioedema not associated with taking ACE inhibitors may have an increased risk of developing angioedema when taking drugs of this group.
In rare cases, intestinal angioedema develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain as an isolated symptom or in combination with nausea and vomiting, in some cases without previous angioedema of the face and with normal levels of C1-esterase. The diagnosis is made using computed tomography of the abdominal cavity, ultrasound, or at the time of surgery. Symptoms disappear after stopping ACE inhibitors. In patients with abdominal pain receiving ACE inhibitors, the possibility of developing intestinal angioedema must be taken into account when making a differential diagnosis.
Anaphylactoid reactions during desensitization
There are isolated reports of the development of long-term life-threatening anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy with hymenopteran insect venom (bees, wasps). ACE inhibitors should be used with caution in patients prone to allergic reactions undergoing desensitization procedures. ACE inhibitors are contraindicated for use in patients receiving desensitizing therapy with venom from hymenoptera insects, such as bees and wasps. The development of anaphylactoid reactions can be avoided by temporarily discontinuing the ACE inhibitor at least 24 hours before the start of the desensitization procedure.
Anaphylactoid reactions during LDL apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be discontinued before each LDL apheresis procedure using dextran sulfate.
Anaphylactoid reactions during hemodialysis
In patients receiving ACE inhibitors, anaphylactoid reactions were observed during hemodilysis using high-flow membranes. Therefore, it is necessary to use a different type of membrane or use an antihypertensive drug of a different pharmacotherapeutic group.
Cough
During therapy with an ACE inhibitor, a dry, persistent cough may develop, which disappears after discontinuation of drugs in this group. If a patient develops a dry cough, one should be aware of the possible connection of this symptom with taking an ACE inhibitor. If the doctor believes that ACE inhibitor therapy is necessary for the patient, taking DILAPREL® PLUS can be continued.
Risk of hypotension and/or renal failure
In some pathological conditions, significant activation of the RAAS may be observed, especially with severe hypovolemia and a decrease in the content of electrolytes in the blood plasma (against the background of a salt-free diet or long-term use of diuretics), in patients with initially low blood pressure, bilateral renal artery stenosis or stenosis of the artery of a single kidney, CHF or liver cirrhosis with edema and ascites. The use of an ACE inhibitor causes blockade of the RAAS and therefore may be accompanied by a sharp decrease in blood pressure and/or an increase in the concentration of creatinine in the blood plasma, indicating the development of acute renal failure. These phenomena are more often observed when taking the first dose of ramipril or during the first 2 weeks of therapy. Sometimes these conditions develop acutely and during other periods of therapy. In such cases, when resuming therapy, it is recommended to use DILAPREL® PLUS at a lower dose and then gradually increase the dose.
Diabetes
When using DILAPREL® PLUS in patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, blood glucose concentrations should be regularly monitored during 1 month of therapy.
Renovascular hypertension
The use of ACE inhibitors has a beneficial effect in patients with renovascular hypertension, both awaiting surgery and when surgery is not possible. Treatment with DILAPREL® PLUS should begin with a low dose of the drug in a hospital setting, monitoring renal function and potassium levels in the blood plasma. Some patients may develop functional renal failure, which quickly disappears when the drug is discontinued.
Surgery/general anesthesia
The use of ACE inhibitors in patients undergoing surgery under general anesthesia can lead to a significant decrease in blood pressure, especially when using general anesthetic agents that have an antihypertensive effect. It is recommended to stop taking ACE inhibitors 48 hours before surgery, warning the anesthesiologist about the use of ACE inhibitors.
Anemia
Anemia may develop in patients who have undergone a kidney transplant or in patients undergoing hemodialysis. In this case, the decrease in Hb concentration is greater, the higher its initial concentration was. This effect does not appear to be dose-dependent, but may be related to the mechanism of action of ACE inhibitors. A slight decrease in Hb concentration occurs during the first 6 months of treatment, then the Hb concentration remains stable and is completely restored after discontinuation of the drug. In such patients, treatment can be continued, but a complete blood count should be performed regularly.
Aortic stenosis/mitral stenosis/hypertrophic obstructive cardiomyopathy (HOCM)
ACE inhibitors are contraindicated in patients with left ventricular outflow tract obstruction and aortic and/or mitral stenosis and HOCM.
Liver failure
In rare cases, while taking ACE inhibitors, cholestatic jaundice occurs, with the progression of which the rapid development of fulminant liver necrosis, sometimes with fatal outcome, is possible. If jaundice appears or a significant increase in the activity of liver transaminases while taking ACE inhibitors, the patient should stop taking DILAPREL® PLUS.
Hyperkalemia
During treatment with ACE inhibitors, hyperkalemia may develop. Risk factors for hyperkalemia are renal failure, old age, diabetes mellitus, some concomitant conditions (decrease in blood volume, acute heart failure in the stage of decompensation, metabolic acidosis), simultaneous use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), as well as drugs potassium or potassium-containing substitutes for table salt and the use of other drugs that increase the content of potassium in the blood plasma (for example, heparin). Hyperkalemia can cause serious heart rhythm problems, sometimes fatal. The simultaneous use of the above drugs is contraindicated.
Other risk groups
In patients with CHF (IV functional class according to the NYHA
) and patients with type 1 diabetes mellitus (risk of spontaneous increase in potassium levels), treatment should begin with low doses of DILAPREL® PLUS and be carried out under constant medical supervision.
In patients with arterial hypertension and coronary artery disease, β-blockers should not be discontinued: ACE inhibitors should be used together with β-blockers.
Elderly patients
In elderly patients, before starting to take DILAPREL® PLUS, it is necessary to evaluate renal function and potassium levels in the blood plasma. In order to prevent the development of arterial hypotension, sequential adjustment of the initial dose of the drug is carried out in accordance with blood pressure indicators, especially with a decrease in blood volume.
Ethnic differences
ACE inhibitors have a less pronounced antihypertensive effect in patients of the Black race compared to representatives of other races.
Impact on the ability to drive vehicles and machinery.
During treatment with DILAPREL® PLUS, it is necessary to refrain from engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, including driving, because While taking the drug DILAPREL® PLUS, dizziness and a decrease in the speed of psychomotor reactions and attention may occur, especially after taking the first dose.
Instructions:
Clinical and pharmacological group
01.024 (ACE inhibitor)
Release form, composition and packaging
Hard gelatin capsules, size No. 3, with a white body and a yellow cap; the contents of the capsules are a powder or compacted mass of white or almost white color, which disintegrates when pressed with a glass rod.
| 1 caps. | |
| ramipril | 2.5 mg |
Excipients: lactose - 143 mg, colloidal silicon dioxide (Aerosil) - 3 mg, calcium stearate - 1.5 mg.
Composition of hard gelatin capsules: gelatin, titanium dioxide, yellow iron oxide dye.
7 pcs. — contour cell packaging (2) — cardboard packs. 7 pcs. — contour cell packaging (4) — cardboard packs. 10 pcs. — contour cell packaging (1) — cardboard packs. 10 pcs. — contour cell packaging (2) — cardboard packs. 10 pcs. — contour cell packaging (3) — cardboard packs. 10 pcs. — contour cell packaging (5) — cardboard packs. 10 pcs. — contour cell packaging (6) — cardboard packs. 14 pcs. — contour cell packaging (1) — cardboard packs. 14 pcs. — contour cell packaging (2) — cardboard packs. 14 pcs. — contour cell packaging (4) — cardboard packs.
Hard gelatin capsules, size No. 3, yellow; the contents of the capsules are a powder or compacted mass of white or almost white color, which disintegrates when pressed with a glass rod.
| 1 caps. | |
| ramipril | 5 mg |
Excipients: lactose - 140.5 mg, colloidal silicon dioxide (Aerosil) - 3 mg, calcium stearate - 1.5 mg.
Composition of hard gelatin capsules: gelatin, titanium dioxide, yellow iron oxide dye.
7 pcs. — contour cell packaging (2) — cardboard packs. 7 pcs. — contour cell packaging (4) — cardboard packs. 10 pcs. — contour cell packaging (1) — cardboard packs. 10 pcs. — contour cell packaging (2) — cardboard packs. 10 pcs. — contour cell packaging (3) — cardboard packs. 10 pcs. — contour cell packaging (5) — cardboard packs. 10 pcs. — contour cell packaging (6) — cardboard packs. 14 pcs. — contour cell packaging (1) — cardboard packs. 14 pcs. — contour cell packaging (2) — cardboard packs. 14 pcs. — contour cell packaging (4) — cardboard packs.
pharmachologic effect
Antihypertensive drug, ACE inhibitor. Ramipril inhibits ACE, blocks the conversion of angiotensin I to angiotensin II, as a result of which, regardless of the activity of plasma renin, a hypotensive effect develops (in the patient’s “lying” and “standing” position) without a compensatory increase in heart rate. Reduces aldosterone production. Reduces peripheral vascular resistance or afterload, pressure in the pulmonary capillaries (preload), resistance in the pulmonary vessels; increases minute blood volume and exercise tolerance. With long-term use, it promotes the reverse development of myocardial hypertrophy in patients with arterial hypertension. Reduces the frequency of arrhythmias during myocardial reperfusion; improves blood supply to ischemic myocardium; prevents changes in the vascular endothelium caused by a high-cholesterol diet.
Strengthens coronary and renal blood flow.
The onset of the hypotensive effect is 1.5 hours after oral administration, the maximum effect is after 5-9 hours, the duration of action is 24 hours. There is no withdrawal syndrome.
In patients with heart failure that developed in the first days of acute myocardial infarction (2-9 days), taking ramipril, starting from 3 to 10 days of acute myocardial infarction, reduces the risk of mortality (by 27%), the risk of sudden death (by 30). %), the risk of progression of chronic heart failure to severe (III-IV functional class according to the NYHA classification)/resistant to therapy (by 27%), the likelihood of subsequent hospitalization due to the development of heart failure (by 26%).
In diabetic and non-diabetic nephropathy, taking ramipril slows the rate of progression of renal failure and the time of onset of end-stage renal failure and, thereby, reduces the need for hemodialysis or kidney transplantation. In the initial stages of diabetic or non-diabetic nephropathy, ramipril reduces the severity of albuminuria.
Pharmacokinetics
Suction
After oral administration, ramipril is rapidly absorbed from the gastrointestinal tract (50-60%). Eating slows down its absorption, but does not affect the completeness of absorption. After taking ramipril orally, the Cmax of ramipril and ramiprilat is achieved after 1 hour and 2-4 hours, respectively.
Bioavailability for ramipril after oral administration of 2.5-5 mg is 15-28%; for ramiprilat - 45%.
Distribution
Plasma protein binding for ramipril is 73%, ramiprilat is 56%. Vd of ramipril - 90 l, ramiprilat - 500 l.
After daily administration at a dose of 5 mg/day, a stable concentration of ramiprilat in the blood plasma is achieved by day 4.
In animal studies, ramipril has been shown to be excreted in breast milk.
Metabolism
It is metabolized in the liver to form the active metabolite ramiprilat (6 times more active in inhibiting ACE than ramipril) and inactive metabolites - diketopiperazine ester, diketopiperazine acid, as well as glucuronides ramipril and ramiprilat. All metabolites formed, with the exception of ramiprilat, have no pharmacological activity.
Removal
T1/2 of ramipril - 5.1 hours. In the distribution and elimination phase, a decrease in the concentration of ramiprilat in the blood serum occurs with T1/2 - 3 hours, followed by a transition phase with T1/2 - 15 hours and a long final phase with very low concentrations of ramiprilat in plasma blood and T1/2 - 4-5 days. T1/2 increases with chronic renal failure.
Excreted by the kidneys - 60%, through the intestines - 40% (mainly in the form of metabolites).
Pharmacokinetics in special clinical situations
If renal function is impaired, the excretion of ramipril and its metabolites slows down in proportion to the decrease in CC.
If liver function is impaired, the conversion to ramiprilat slows down.
In heart failure, the concentration of ramiprilat increases by 1.5-1.8 times.
In healthy elderly volunteers (65-76 years), the pharmacokinetics of ramipril and ramiprilat do not differ significantly from those in young healthy volunteers.
Dosage
The drug is taken orally. Capsules must be swallowed whole with a sufficient amount (1/2 cup) of water, regardless of meals (i.e., capsules can be taken before, during or after meals).
The dose is selected depending on the therapeutic effect and tolerability of the drug.
Arterial hypertension
The initial dose is 2.5 mg 1 time/day in the morning. If, when taking the drug at this dose for 3 weeks or more, it is not possible to normalize blood pressure, then the dose can be increased to 5 mg/day. If the drug is insufficiently effective at a dose of 5 mg, after 2-3 weeks it can be further doubled to the maximum recommended dose of 10 mg/day. As an alternative to increasing the dose to 10 mg/day if the hypotensive effect of a dose of 5 mg/day is insufficient, it is possible to add other antihypertensive drugs to the treatment, in particular diuretics or slow calcium channel blockers.
Chronic heart failure
The initial dose is 1.25 mg/day (it is possible to use ramipril in another dosage form - 2.5 mg scored tablets). Depending on the patient's response to the therapy, the dose can be increased. It is recommended to double it at intervals of 1-2 weeks. Doses of 2.5 mg or more should be taken 1 time/day or divided into 2 doses. The maximum daily dose is 10 mg.
For heart failure that developed during the first few days (from 2 to 9 days) after acute myocardial infarction
The initial dose is 2.5 mg 2 times a day, morning and evening. If the patient does not tolerate this initial dose (an excessive decrease in blood pressure is observed), then it is recommended to take 1.25 mg 2 times a day for two days (in this case, ramipril can be used in another dosage form - tablets of 2.5 mg with a score). Then, depending on the patient's response, the dose may be increased. It is recommended that the dose be doubled at intervals of 1-3 days when increasing it. Later, the total daily dose, which was initially divided into 2 doses, can be administered in 1 dose. The maximum recommended dose is 10 mg/day.
Currently, the experience of treating patients with severe chronic heart failure (III-IV functional class according to the NYHA classification), which arose immediately after acute myocardial infarction, is insufficient.
If a decision is made to treat such patients with Dilaprel®, it is recommended that treatment begin with the lowest effective dose - 1.25 mg 1 time / day (in this case, ramipril can be used in another dosage form - 2.5 mg scored tablets), and Particular care should be taken whenever the dose is increased.
For diabetic or non-diabetic nephropathy
The initial dose is 1.25 mg (it is possible to use ramipril in another dosage form - 2.5 mg tablets with a score line) 1 time / day. The dose can be increased to 5 mg 1 time/day. The maximum daily dose is 5 mg.
Special patient groups
In patients with impaired renal function with CC from 50 to 20 ml/min/1.73 m2, the initial daily dose is usually 1.25 mg (in this case, you can use the drug ramipril in another dosage form - 2.5 mg scored tablets). The maximum permissible daily dose is 5 mg.
In patients with incompletely corrected loss of fluid and electrolytes, patients with severe arterial hypertension, as well as patients for whom an excessive decrease in blood pressure poses a certain risk (for example, with severe atherosclerotic lesions of the coronary and cerebral arteries), the initial dose is reduced to 1.25 mg / day (in In this case, you can use ramipril in another dosage form - tablets of 2. mg with a score).
In patients receiving prior diuretic therapy, it is necessary, if possible, to discontinue diuretics 2-3 days (depending on the duration of action of the diuretics) before starting treatment with Dilaprel®, or at least reduce the dose of diuretics taken. Treatment of such patients should begin with the lowest dose, equal to 1.25 mg of ramipril (in this case, ramipril can be used in another dosage form - 2.5 mg scored tablets) 1 time / day in the morning. After taking the first dose and whenever the dose of ramipril and/or loop diuretics is increased, patients should be under medical supervision for at least 8 hours to avoid an uncontrolled hypotensive reaction.
In elderly patients (over 65 years of age), the initial dose should be reduced to 1.25 mg/day (in this case, ramipril can be used in another dosage form - 2.5 mg scored tablets).
In patients with impaired liver function, the blood pressure response to taking Dilaprel® can either increase (due to slower elimination of ramiprilat) or decrease (due to slower conversion of low-active ramipril to active ramiprilat). Therefore, careful medical supervision is required at the beginning of treatment. The maximum permissible daily dose is 2.5 mg.
Overdose
Symptoms: excessive peripheral vasodilation with the development of a pronounced decrease in blood pressure, shock; bradycardia, fluid and electrolyte disturbances, acute renal failure, stupor.
Treatment: gastric lavage, taking adsorbents, sodium sulfate (preferably within 30 minutes after administration).
With a pronounced decrease in blood pressure - replenishment of blood volume, restoration of water and electrolyte balance in the blood, intravenous administration of catecholamines, angiotensin II; for bradycardia - installation of an artificial pacemaker. In case of overdose, it is necessary to monitor serum concentrations of creatinine and electrolytes. Hemodialysis is ineffective.
Drug interactions
Contraindicated combinations
Use of certain high-flux membranes with a negatively charged surface (for example, polyacrylonitrile membranes) during hemodialysis or hemofiltration, use of dextran sulfate during LDL apheresis: risk of severe anaphylactic reactions.
Combinations not recommended
With potassium salts, potassium-sparing diuretics (for example, amiloride, triamterene, spironolactone): a more pronounced increase in serum potassium levels is possible (with simultaneous use, regular monitoring of serum potassium levels is required).
Combinations to use with caution
With antihypertensive drugs (especially diuretics) and other drugs that lower blood pressure (nitrates, tricyclic antidepressants): potentiation of the hypotensive effect (when combined with diuretics, the sodium content in the blood serum should be monitored).
With sleeping pills, narcotic analgesics and painkillers: increased hypotensive effect.
With vasopressor sympathomimetics (epinephrine): reducing the hypotensive effect of ramipril (regular blood pressure monitoring is required).
With allopurinol, procainamide, cytostatics, immunosuppressants, systemic corticosteroids and other drugs that can affect hematological parameters: combined use increases the risk of developing leukopenia.
With lithium salts: increased serum concentration of lithium and increased cardio- and neurotoxic effects of lithium.
With hypoglycemic agents for oral administration (sulfonylurea derivatives, biguanides), insulin: due to a decrease in insulin resistance under the influence of ramipril, the hypoglycemic effect of these drugs may be enhanced, up to the development of hypoglycemia.
Combinations to Consider
With NSAIDs (indomethacin, acetylsalicylic acid): the effect of ramipril may be weakened, the risk of renal dysfunction and increased potassium levels in the blood serum may be increased.
With heparin: an increase in serum potassium levels is possible.
With sodium chloride: weakening of the hypotensive effect of ramipril and less effective treatment of symptoms of chronic heart failure.
With ethanol: increased symptoms of vasodilation; Ramipril may increase the adverse effects of ethanol on the body.
With estrogens: weakening of the hypotensive effect of ramipril (fluid retention).
Desensitization therapy for hypersensitivity to insect venoms: ACE inhibitors, including ramipril, increase the likelihood of developing severe anaphylactic or anaphylactoid reactions to insect venoms.
Use during pregnancy and lactation
Dilaprel® is contraindicated during pregnancy and lactation (breastfeeding).
Before starting treatment, you should make sure there is no pregnancy. If the patient becomes pregnant during treatment, it is necessary to replace Dilaprel® therapy with another therapy as soon as possible. Otherwise, there is a risk of fetal damage, especially in the first trimester of pregnancy.
It is recommended to closely monitor neonates exposed in utero to ACE inhibitors for hypotension, oliguria, and hyperkalemia. In oliguria, it is necessary to maintain blood pressure and renal perfusion by administering appropriate fluids and vasoconstrictors. Neonates are at risk for oliguria and neurological disorders, possibly due to decreased renal and cerebral blood flow due to the reduction in blood pressure caused by ACE inhibitors.
If treatment with Dilaprel® is necessary during lactation, breastfeeding should be discontinued.
Side effects
Determination of the frequency of adverse reactions: very often (≥10%); often (≥1% -<10%); uncommon (≥0.1% - <1%); rarely (≥0.01% - <0.1%); very rare (<0.01%, including isolated reports); frequency unknown (it is not possible to determine the frequency of occurrence based on available data).
From the cardiovascular system: often - excessive decrease in blood pressure, orthostatic hypotension, syncope, chest pain; uncommon - myocardial ischemia, including the development of an attack of angina or myocardial infarction, tachycardia, arrhythmias (appearance or intensification), palpitations, peripheral edema, flushing of the facial skin; rarely - development or intensification of circulatory disorders against the background of stenotic vascular lesions, vasculitis; frequency unknown - Raynaud's syndrome,
From the urinary system: rarely - impaired renal function, including the development of acute renal failure, an increase in the amount of urine excreted, an increase in existing proteinuria, an increase in the concentration of urea and creatinine in the blood.
From the reproductive system: infrequently - transient impotence due to erectile dysfunction, decreased libido; frequency unknown - gynecomastia.
From the nervous system: often - headache, a feeling of “lightness” in the head, a feeling of fatigue; infrequently - dizziness; depressed mood, anxiety, increased excitability, restlessness, sleep disturbances, including drowsiness; rarely - tremor, imbalance, confusion, asthenia; frequency unknown - cerebral ischemia, including ischemic stroke and transient cerebrovascular accident, impaired psychomotor reactions, paresthesia (burning sensation), impaired attention.
From the senses: infrequently - visual disturbances, including blurred vision, ageusia (loss of taste sensitivity), dysgeusia (impaired taste sensitivity); rarely - conjunctivitis, hearing impairment, tinnitus; frequency unknown - parosmia (impaired perception of smells).
From the musculoskeletal system: often - muscle cramps, myalgia; infrequently - arthralgia.
From the digestive system: often - inflammatory reactions in the stomach and intestines, indigestion, discomfort in the abdominal area, dyspepsia, diarrhea, nausea, vomiting; uncommon - pancreatitis, incl. and with a fatal outcome, increased activity of pancreatic enzymes in the blood plasma, intestinal angioedema, abdominal pain, gastritis, constipation, dry oral mucosa, increased activity of liver enzymes and the concentration of conjugated bilirubin in the blood plasma, anorexia, decreased appetite; rarely - glossitis, cholestatic jaundice, hepatocellular lesions; frequency unknown - aphthous stomatitis, acute liver failure, cholestatic or cytolytic hepatitis (death was extremely rare).
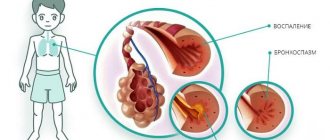
From the respiratory system: often - dry cough (worsening at night when lying down), sinusitis, bronchitis, shortness of breath; infrequently - bronchospasm, including worsening of bronchial asthma, nasal congestion.
Dermatological reactions: often - skin rash, in particular macular-papular; infrequently - skin itching, hyperhidrosis (excessive sweating); rarely - exfoliative dermatitis, onycholysis; very rarely - photosensitivity reactions; frequency unknown - pemphigus, aggravation of psoriasis, psoriasis-like dermatitis, pemphigoid or lichenoid (lichenoid) exanthema or enanthema, alopecia.
Allergic reactions: uncommon - angioedema, incl. and with a fatal outcome (swelling of the larynx can cause airway obstruction, leading to death); rarely - urticaria; frequency unknown - toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, anaphylactic or anaphylactoid reactions (with ACE inhibition, the number of anaphylactic or anaphylactoid reactions to insect venoms increases), increased concentration of antinuclear antibodies.
From the hematopoietic system: infrequently - eosinophilia; rarely - leukopenia, including neutropenia and agranulocytosis, a decrease in the number of red blood cells in the peripheral blood, a decrease in hemoglobin concentration, thrombocytopenia; frequency unknown - suppression of bone marrow hematopoiesis, pancytopenia, hemolytic anemia.
From laboratory parameters: often - increased potassium content in the blood; frequency unknown - decreased sodium content in the blood.
Other: infrequently - hyperthermia.
Storage conditions and periods
The drug should be stored out of the reach of children, in a dry place, protected from light, at a temperature not exceeding 25°C. Shelf life: 2 years.
Indications
- arterial hypertension;
- chronic heart failure (as part of combination therapy, in particular in combination with diuretics);
- heart failure that developed during the first few days (from 2 to 9 days) after acute myocardial infarction;
- diabetic or non-diabetic nephropathy, preclinical and clinically pronounced stages, incl. with severe proteinuria, especially when combined with arterial hypertension.
Contraindications
- history of angioedema (hereditary or idiopathic, as well as after taking ACE inhibitors) (risk of rapid development of angioedema);
- hemodynamically significant stenosis of the renal arteries (bilateral or unilateral in the case of a solitary kidney);
- arterial hypotension (systolic blood pressure less than 90 mm Hg) or conditions with unstable hemodynamic parameters;
- hemodynamically significant stenosis of the aortic or mitral valve;
— hypertrophic obstructive cardiomyopathy;
- primary hyperaldosteronism;
— severe renal failure (creatinine clearance less than 20 ml/min with a body surface of 1.73 m2);
- hemodialysis;
- pregnancy;
- lactation period;
- nephropathy, treated with corticosteroids, NSAIDs, immunosuppressants and/or other cytotoxic agents;
— chronic heart failure in the stage of decompensation (experience of clinical use is insufficient);
- age under 18 years (efficacy and safety have not been established);
— apheresis of LDL using dextran sulfate (risk of developing hypersensitivity reactions);
- hyposensitizing therapy for hypersensitivity reactions to insect poisons, such as bees, wasps;
- lactase deficiency, lactose intolerance, glucose-galactose malabsorption;
- hypersensitivity to the components of the drug;
- hypersensitivity to other ACE inhibitors;
Additional contraindications when using Dilaprel® in the acute stage of myocardial infarction:
— severe chronic heart failure (III-IV functional class according to the NYHA classification);
- unstable angina;
- life-threatening ventricular arrhythmias;
- “pulmonary” heart.
Carefully:
- conditions in which an excessive decrease in blood pressure is especially dangerous (with atherosclerotic lesions of the coronary and cerebral arteries);
- conditions accompanied by an increase in the activity of the RAAS, in which, with ACE inhibition, there is a risk of a sharp decrease in blood pressure with deterioration of renal function (severe arterial hypertension, especially malignant arterial hypertension; chronic heart failure, especially severe or for which other drugs with antihypertensive effects are taken; hemodynamically significant unilateral renal artery stenosis in the presence of both kidneys; previous use of diuretics; disturbances in water and electrolyte balance as a result of insufficient intake of fluid and table salt, diarrhea, vomiting, profuse sweating);
- liver dysfunction (lack of experience with use: it is possible to either enhance or weaken the effects of ramipril; in patients with liver cirrhosis with ascites and edema, significant activation of the RAAS is possible);
- impaired renal function (creatinine clearance > 20 ml/min with a body surface of 1.73 m2) due to the risk of developing hyperkalemia and leukopenia;
— condition after kidney transplantation;
- systemic connective tissue diseases, incl. systemic lupus erythematosus, scleroderma, concomitant therapy with myelotoxic drugs that can cause changes in the peripheral blood picture (possible inhibition of bone marrow hematopoiesis, development of neutropenia or agranulocytosis);
— diabetes mellitus (risk of developing hyperkalemia);
- old age (risk of increased hypotensive effect);
- hyperkalemia.
special instructions
Treatment with Dilaprel® is usually long-term, its duration in each case is determined by the doctor. During treatment, regular medical supervision is required, in particular for patients with impaired liver and kidney function.
Before starting treatment with Dilaprel®, it is necessary to eliminate hyponatremia and hypovolemia. In patients who have previously taken diuretics, it is necessary to discontinue them or at least reduce their dose 2-3 days before starting Dilaprel® (in this case, the condition of patients with chronic heart failure should be carefully monitored, due to the possibility of developing their decompensation due to an increase in blood volume).
After taking the first dose of the drug, as well as when increasing its dose and/or the dose of diuretics (especially loop diuretics), it is necessary to ensure careful medical monitoring of the patient for at least 8 hours so that appropriate measures can be taken in a timely manner in case of an excessive decrease in blood pressure.
If Dilaprel® is used for the first time or at a high dose in patients with increased RAAS activity, their blood pressure should be carefully monitored, especially at the beginning of treatment, because these patients have an increased risk of excessive reduction in blood pressure.
In case of malignant arterial hypertension and heart failure, especially in the acute stage of myocardial infarction, treatment with Dilaprel® should only be started in a hospital setting.
In patients with chronic heart failure, taking the drug can lead to the development of a pronounced decrease in blood pressure, which in some cases is accompanied by oliguria or azotemia and rarely by the development of acute renal failure.
Caution should be exercised when treating elderly patients, because... They may be particularly sensitive to ACE inhibitors; monitoring of renal function is recommended during the initial phase of treatment. In patients for whom a decrease in blood pressure may pose a certain risk (for example, in patients with atherosclerotic narrowing of the coronary or cerebral arteries), treatment should be initiated under strict medical supervision.
Caution should be exercised during physical activity and/or hot weather due to the risk of increased sweating and dehydration with the development of arterial hypotension due to a decrease in blood volume and a decrease in sodium concentration in the blood.
It is not recommended to drink alcohol during treatment with Dilaprel®.
Transient arterial hypotension is not a contraindication for continuing treatment after stabilization of blood pressure. If severe arterial hypotension develops again, the dose should be reduced or the drug discontinued.
Cases of angioedema of the face, extremities, lips, tongue, pharynx or larynx have been observed in patients treated with ACE inhibitors. If swelling occurs in the face (lips, eyelids) or tongue, or difficulty swallowing or breathing, the patient should immediately stop taking the drug
Angioedema localized in the area of the tongue, pharynx, or larynx (possible symptoms: difficulty swallowing or breathing) can be life-threatening and requires urgent measures to relieve it: subcutaneous injection of 0.3-0.5 mg or intravenous drip of 0.1 mg of epinephrine (under the control of blood pressure, heart rate and ECG) followed by the use of corticosteroids (iv, intramuscular or orally); IV administration of antihistamines (H1- and H2-histamine receptor blockers) is also recommended, and in case of insufficiency of C1-esterase enzyme inactivators, the need to administer C1-esterase enzyme inhibitors in addition to epinephrine can be considered. The patient should be hospitalized and monitored until symptoms are completely relieved, but not less than 24 hours.
Cases of intestinal angioedema, manifested by abdominal pain with or without nausea and vomiting, have been observed in patients receiving ACE inhibitors; in some cases, angioedema of the face was simultaneously observed. If a patient develops the symptoms described above during treatment with ACE inhibitors, the possibility of developing intestinal angioedema should be considered when making a differential diagnosis.
Treatment aimed at desensitization to insect venom (bees, wasps) and concomitant use of ACE inhibitors can initiate anaphylactic and anaphylactoid reactions (for example, decreased blood pressure, shortness of breath, vomiting, allergic skin reactions), which can sometimes be life-threatening. During treatment with ACE inhibitors, hypersensitivity reactions to insect venom (for example, bees, wasps) develop faster and are more severe. If desensitization to insect venom is necessary, the ACE inhibitor should be temporarily replaced with an appropriate drug of a different class.
With the use of ACE inhibitors, life-threatening, rapidly developing anaphylactoid reactions, sometimes up to the development of shock, have been described during hemodialysis or plasma filtration using certain high-flow membranes (for example, polyacrylonitrile membranes). It is necessary to avoid the combined use of Dilaprel® and this type of membrane, for example, for urgent hemodialysis or hemofiltration. In this case, it is preferable to use other membranes or avoid taking ACE inhibitors. Similar reactions were observed with LDL apheresis using dextran sulfate. Therefore, this method should not be used in patients receiving ACE inhibitors.
In patients with impaired liver function, the response to treatment with Dilaprel® may be either enhanced or weakened. In addition, in patients with severe liver cirrhosis with edema and/or ascites, significant activation of the RAAS is possible, so special care is required when treating these patients.
Before surgery (including dentistry), it is necessary to warn the anesthesiologist about the use of ACE inhibitors.
Monitoring laboratory parameters before and during treatment with Dilaprel® (up to 1 time per month for the first time for 3-6 months of treatment)
When treating with ACE inhibitors, it is recommended to monitor renal function in the first weeks of treatment and subsequently. Particularly careful monitoring is required in patients with acute and chronic heart failure, impaired renal function, after kidney transplantation, patients with renovascular diseases, including patients with hemodynamically significant unilateral renal artery stenosis in the presence of two kidneys (in such patients, even a slight increase in serum creatinine concentration may be indicator of decreased kidney function).
Regular monitoring of serum potassium levels is recommended. Particularly careful monitoring of potassium levels in the blood serum is required for patients with impaired renal function, significant disturbances in water and electrolyte balance, and chronic heart failure.
It is recommended to monitor indicators of a general blood test to identify possible leukopenia. More regular monitoring is recommended at the beginning of treatment and in patients with impaired renal function, as well as in patients with connective tissue diseases or in patients simultaneously receiving other drugs that can change the peripheral blood picture. Monitoring the number of leukocytes is necessary for the early detection of leukopenia, which is especially important in patients with an increased risk of its development, as well as at the first signs of infection. If neutropenia is detected (the number of neutrophils is less than 2000/μl), discontinuation of treatment with ACE inhibitors is required.
If symptoms associated with leukopenia appear (for example, fever, enlarged lymph nodes, tonsillitis), urgent monitoring of the peripheral blood picture is necessary. If signs of bleeding appear (tiny petechiae, red-brown rashes on the skin and mucous membranes), monitoring the number of platelets in the peripheral blood is also necessary.
If jaundice or a significant increase in the activity of liver enzymes occurs, treatment with Dilaprel® should be discontinued and patients should be monitored by physicians.
Impact on the ability to drive vehicles and operate machinery
During treatment with Dilaprel®, it is necessary to refrain from engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions, including driving, because While taking it, you may experience dizziness, decreased speed of psychomotor reactions, and decreased attention, especially after taking the first dose.
Use for renal impairment
Use is contraindicated in severe renal failure (creatinine clearance less than 20 ml/min with a body surface of 1.73 m2);
Conditions for dispensing from pharmacies
The drug is available with a prescription.
Dilaprel (capsules 10 mg N28) JSC Vertex - Russia in pharmacies in Yekaterinburg
| Registration certificate number: | LP-000892 |
| Registration date: | 18.10.2011 |
| Expiration date of the registration certificate: | 18.10.2016 |
| Legal entity in whose name the registration certificate was issued: | CJSC Vertex - Russia |
| Manufacturer: | CJSC Vertex - Russia |
| Trade name of the medicinal product: | Dilaprel ( |
| International nonproprietary or chemical name: | Ramipril |
1. Packaging of capsules 2.5 mg 10 pcs., blister packs (1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 2. Packaging of capsules 5 mg 14 pcs., blister packs (1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 3. Packaging 5 mg capsules 10 pcs., polymer jars (1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 4. Packaging 2.5 mg capsules 14 pcs., contour cell packaging ( 1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 5. Packaging of 5 mg capsules 10 pcs., cellular contour packs (3) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 6. Packaging of 2.5 mg capsules 10 pcs., blister packs (3) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 7. Packaging of 5 mg capsules 10 pcs., blister packs (1) - cardboard packs Registration number LP-000169 Registration date 13.01 .2011 8. Packaging of capsules 5 mg 10 pcs., blister packs (5) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 9. Packaging of capsules 2.5 mg 10 pcs., blister packs (2) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 10. Packaging of 2.5 mg capsules, 14 pcs., contour blister packs (2) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 11. Packaging of 5 mg capsules, 10 pcs., packs cellular contour packs (2) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 12. Packaging 2.5 mg capsules 10 pcs., cellular contour packs (5) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 13. Packaging 5 mg capsules 30 pcs., polymer jars (1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 14. Packaging 2.5 mg capsules 30 pcs., polymer jars (1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 15. Packaging of capsules 2.5 mg 14 pcs., blister packs (4) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 16. Packaging of capsules 5 mg 14 pcs., blister packs (2) - packs cardboard Registration number LP-000169 Registration date 01/13/2011 17. Packaging 2.5 mg capsules 10 pcs., blister contour packaging (6) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 18. Packaging 2.5 mg capsules 10 pcs. polymer jars (1) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 19. Packaging 5 mg capsules 10 pcs., cellular contour packs (6) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 20. Packaging capsules 5 mg 14 pcs., blister packs (4) - cardboard packs Registration number LP-000169 Registration date 01/13/2011 DILAPREL® Representation: ATX code: C09AA05 Registration certificate holder: VERTEKS, JSC ramipril Release form, composition and packaging Capsules 1 capsule. ramipril 2.5 mg 10 - contour blister packs (3) - cardboard packs. 10 - contour cell packaging (1) - cardboard packs. 10 - contour cell packaging (2) - cardboard packs. 10 - contour cell packaging (5) - cardboard packs. 10 - contour cell packaging (6) - cardboard packs. 7 - contour cell packaging (2) - cardboard packs. 7 - contour cell packaging (4) - cardboard packs. 14 - contour cell packaging (4) - cardboard packs. 14 - contour cell packaging (1) - cardboard packs. Capsules 1 capsule. ramipril 5 mg 10 - contour blister packs (3) - cardboard packs. 10 - contour cell packaging (1) - cardboard packs. 10 - contour cell packaging (2) - cardboard packs. 10 - contour cell packaging (5) - cardboard packs. 10 - contour cell packaging (6) - cardboard packs. 7 - contour cell packaging (2) - cardboard packs. 7 - contour cell packaging (4) - cardboard packs. 14 - contour cell packaging (4) - cardboard packs. 14 - contour cell packaging (1) - cardboard packs. Clinical and pharmacological group: ACE inhibitor Indications for use of the drug DILAPREL® - arterial hypertension; - chronic heart failure (as part of combination therapy, in particular in combination with diuretics); - heart failure that developed during the first few days (from the 2nd to the 9th day) after acute myocardial infarction; - diabetic or non-diabetic nephropathy, preclinical and clinically pronounced stages, including with severe proteinuria, especially when combined with arterial hypertension. Dosage regimen Capsules must be swallowed whole and washed down with a sufficient amount (1/2 glass) of water, regardless of meals (that is, capsules can be taken before, during or after meals). The dose is selected depending on the therapeutic effect and tolerability of the drug by the patient. Arterial hypertension Orally, initial dose – 2.5 mg, once, in the morning. If, when taking the drug at this dose for 3 weeks or more, it is not possible to normalize blood pressure, then the dose can be increased to 5 mg of Dilaprel®. If the dose of 5 mg is insufficiently effective, after 2-3 weeks it can be further doubled to the maximum The recommended daily dose is 10 mg. As an alternative to increasing the dose to 10 mg per day if the hypotensive effect of a daily dose of 5 mg is insufficient, it is possible to add other antihypertensive drugs to the treatment, in particular diuretics or blockers of “slow” calcium channels. Chronic heart failure Initial dose – 1.25 mg/(it is possible to use ramipril in another dosage form: 2.5 mg scored tablets). Depending on the patient's response to the therapy, the dose can be increased. It is recommended to double it at intervals of 1-2 weeks. Doses of 2.5 mg or more should be taken once or divided into 2 doses. The maximum daily dose is 10 mg. For heart failure that develops during the first few days (from the 2nd to the 9th day) after acute myocardial infarction The initial dose is 5 mg, divided into 2 doses, 2.5 mg in the morning and evening. If the patient does not tolerate this initial dose (an excessive decrease in blood pressure is observed), then it is recommended that he be given 1.25 mg 2 times a day for two days (in this case, the drug ramipril can be used in another dosage form: tablets of 2.5 mg with a score). Then, depending on the patient's response, the dose may be increased. It is recommended that the dose be doubled at intervals of 1-3 days when increasing it. Later, the total daily dose, which was initially divided into two doses, can be given once. The maximum recommended dose is 10 mg. Currently, the experience of treating patients with severe chronic heart failure (III-IV functional class according to the NYHA classification), which arose immediately after acute myocardial infarction, is insufficient. If a decision is made to treat such patients with Dilaprel®, it is recommended that treatment begin with the lowest possible dose - 1/25 mg 1 time per day (in this case, ramipril can be used in another dosage form: 2.5 mg tablets with a score ) and special care should be taken whenever the dose is increased. For diabetic or non-diabetic nephropathy, the initial dose is 1.25 mg (it is possible to use the drug ramipril in another dosage form: tablets of 2.5 mg with a score) 1 time per day. The dose can be increased to 5 mg 1 time per day. The maximum daily dose is 5 mg. Use of the drug Dilaprel® in certain groups of patients Patients with impaired renal function With CC from 50 to 20 ml/min per 1.73 m2 of body surface, the initial daily dose is usually 1.25 mg (in this case, you can use the drug ramipril in another dosage form: tablets of 2.5 mg with a score). The maximum permissible daily dose is 5 mg. Patients with incompletely corrected loss of fluid and electrolytes, patients with severe arterial hypertension, as well as patients for whom an excessive decrease in blood pressure poses a certain risk (for example, with severe atherosclerotic lesions of the coronary and cerebral arteries) The initial dose is reduced to 1.25 mg/day (in this case You can use the drug ramipril in another dosage form: tablets of 2. mg with a score). Patients with previous diuretic therapy It is necessary, if possible, to discontinue diuretics 2-3 days (depending on the duration of action of the diuretics) before starting treatment with Dilaprel®, or at least reduce the dose of diuretics taken. Treatment of such patients should begin with the lowest dose, equal to 1.25 mg ramipril a (in this case, the drug ramipril can be used in another dosage form: 2.5 mg scored tablets), taken once a day, in the morning. After taking the first dose and each time after increasing the dose of ramipril and (or) loop diuretics, patients should be under medical supervision for at least 8 hours to avoid an uncontrolled hypotensive reaction. Elderly patients (over 65 years old) The initial dose is reduced to 1.25 mg per day (in this case, ramipril can be used in another dosage form: 2.5 mg scored tablets). Patients with impaired liver function The blood pressure response to taking Dilaprel® can either increase (due to slower excretion of ramiprilat) or decrease (due to slower conversion of low-active ramipril to active ramiprilat). Therefore, careful medical supervision is required at the beginning of treatment. The maximum permissible daily dose is 2.5 mg. Side effects The undesirable effects listed below are given in accordance with the following gradations of the frequency of their occurrence: very often: (? 10%); often: (?1% -<10%); uncommon: (?0.1% - <1%); rarely: (?0.01% - <0.1%); very rare: (<0.01%, including isolated reports); frequency unknown: based on available data, it is not possible to determine the frequency of occurrence. From the cardiovascular system: often - excessive decrease in blood pressure, orthostatic hypotension, syncope, chest pain; uncommon - myocardial ischemia, including the development of an attack of angina or myocardial infarction, tachycardia, arrhythmias (appearance or intensification), palpitations, peripheral edema, “flushes” of blood to the skin of the face. From the genitourinary system: infrequently - impaired renal function, including the development of acute renal failure, an increase in the amount of urine excreted, an increase in existing proteinuria, an increase in the concentration of urea and creatinine in the blood, transient impotence due to erectile dysfunction, decreased libido; frequency unknown - gynecomastia. From the central nervous system: often - headache, a feeling of “lightness” in the head, a feeling of fatigue; infrequently - dizziness, ageusia (loss of taste sensitivity), dysgeusia (impaired taste sensitivity); depressed mood, anxiety, increased excitability, restlessness, sleep disturbances, including drowsiness; rarely - tremor, imbalance, development or intensification of circulatory disorders against the background of stenotic vascular lesions, vasculitis, confusion, asthenia; frequency unknown - Raynaud's syndrome, cerebral ischemia, including ischemic stroke and transient cerebrovascular accident, impaired psychomotor reactions, paresthesia (burning sensation), parosmia (impaired odor perception), impaired attention. From the senses: infrequently - visual disturbances, including blurred vision; rarely - conjunctivitis, hearing impairment, tinnitus. From the musculoskeletal system: often - muscle cramps, myalgia; infrequently - arthralgia. From the digestive system: often - inflammatory reactions in the stomach and intestines, indigestion, discomfort in the abdominal area, dyspepsia, diarrhea, nausea, vomiting; infrequently - pancreatitis, including with a fatal outcome, increased activity of pancreatic enzymes in the blood plasma, intestinal angioedema, abdominal pain, gastritis, constipation, dryness of the oral mucosa, increased activity of liver enzymes and the concentration of conjugated bilirubin in blood plasma, anorexia, loss of appetite; rarely - glossitis, cholestatic jaundice, hepatocellular lesions; frequency unknown - aphthous stomatitis, acute liver failure, cholestatic or cytolytic hepatitis (death was extremely rare). From the respiratory system: often - “dry” cough (worsening at night when lying down), sinusitis, bronchitis, shortness of breath; infrequently - bronchospasm, including worsening of bronchial asthma, nasal congestion. From the skin: often - skin rash, in particular macular-papular; uncommon - angioedema, including death (swelling of the larynx can cause airway obstruction leading to death), itching, hyperhidrosis (excessive sweating); rarely - exfoliative dermatitis, urticaria, onycholysis; very rarely - photosensitivity reactions; frequency unknown - toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme pemphigus, worsening psoriasis, psoriasis-like dermatitis, pemphigoid or lichenoid (lichenoid) exanthema or enanthema, alopecia; anaphylactic or anaphylactoid reactions (with ACE inhibition, the number of anaphylactic or anaphylactoid reactions to insect venoms increases), increased concentration of antinuclear antibodies. From the hematopoietic organs: infrequently - eosinophilia; rarely - leukopenia, including neutropenia and agranulocytosis, a decrease in the number of red blood cells in the peripheral blood, a decrease in hemoglobin concentration, thrombocytopenia; frequency unknown - suppression of bone marrow hematopoiesis, pancytopenia, hemolytic anemia. Other: infrequently - hyperthermia. Laboratory indicators often include increased potassium levels in the blood; unknown frequency - decreased sodium levels in the blood. Contraindications to the use of the drug DILAPREL® - hypersensitivity to ramipril, other ACE inhibitors, or to any of the components of the drug; - history of angioedema (hereditary or idiopathic, as well as after taking LPF inhibitors) - risk of rapid development of angioedema; - hemodynamically significant stenosis of the renal arteries (bilateral or unilateral in the case of a solitary kidney); — arterial hypotension (systolic blood pressure less than 90 mm Hg) or conditions with unstable hemodynamic parameters; - hemodynamically significant stenosis of the aortic or mitral valve or hypertrophic obstructive cardiomyopathy (HOCM); - primary hyperaldosteronism; - severe renal failure (creatinine clearance less than 20 ml/min with a body surface of 1.73 m:); - hemodialysis; - pregnancy; - lactation period; - nephropathy, treated with glucocorticosteroids, non-steroidal anti-inflammatory drugs, immunosuppressants and/or other cytotoxic agents; — chronic heart failure in the stage of decompensation (experience of clinical use is insufficient); - age under 18 years (efficacy and safety have not been established); - apheresis of low-density lipoproteins using dextran sulfate (risk of developing hypersensitivity reactions); - hyposensitizing therapy for hypersensitivity reactions to insect poisons, such as bees, wasps; - lactase deficiency, lactose intolerance, glucose-galactose malabsorption. Additional contraindications when using the drug Dilapre® in the acute stage of myocardial infarction: - severe chronic heart failure (III-IV functional class according to the NYHA classification); - unstable angina; - life-threatening ventricular disorders in the heart. With caution: - conditions in which an excessive decrease in blood pressure is especially dangerous (with atherosclerotic lesions of the coronary and cerebral arteries); - conditions accompanied by increased activity of the renin-angiotensin-aldosterone system (RAAS), in which, with ACE inhibition, there is a risk of a sharp decrease in blood pressure with deterioration of renal function: - severe arterial hypertension, especially malignant arterial hypertension; - chronic heart failure, especially severe or for which other drugs with antihypertensive effects are taken; - hemodynamically significant unilateral renal artery stenosis (in the presence of both kidneys); - previous use of diuretics; - disturbances in water and electrolyte balance as a result of insufficient intake of liquid and table salt, diarrhea, vomiting, profuse sweating. - liver dysfunction (lack of experience with use: both strengthening and weakening of the effects of ramipril are possible; in patients with cirrhosis of the liver with ascites and edema, significant activation of the RAAS is possible; - impaired renal function (creatinine clearance more than 20 ml/min with a body surface of 1.73 m2 ) Due to the risk of hyperkalemia and leukopenia;-the condition after kidney transplantation;-systemic diseases of the connective tissue, including systemic lupus erythematosus, scleroderma, accompanying therapy with myelotoxic drugs that can cause changes in the picture of peripheral blood (it is possible to inhibit bosomostium hematopoiesis, development, development. neutropenia or agranulocytosis); - diabetes mellitus (risk of hypercalemia); - elderly (risk of increased hypotensive effects); - hyperkalemia. The use of the drug dilaprele® during pregnancy and breastfeeding dilaprel® should not be used during pregnancy. Therefore, before the treatment, it is necessary to make sure that the treatment should be convinced In the absence of pregnancy. If the patient became pregnant during the treatment period, it is necessary to replace the drug therapy with diladriel® with another therapy as early as possible. Otherwise, there is a risk of fetal damage, especially in the I trimester of pregnancy. If the treatment of diladrel® is necessary during lactation, then breastfeeding should be stopped. Conditions of vacation from pharmacies are released by prescription. The conditions and terms of storage in a dry place protected from light at a temperature of not higher than 25 ° C. Keep out of the reach of children. Best before date. 2 years. Do not use after expiration date.
Dilaprel®
Treatment with Dilaprel® is usually long-term, its duration in each case is determined by the doctor. During treatment, regular medical supervision is required, in particular for patients with impaired liver and kidney function.
Before starting treatment with Dilaprel®, it is necessary to eliminate hyponatremia and hypovolemia. In patients who have previously taken diuretics, it is necessary to discontinue them or at least reduce their dose 2-3 days before starting Dilaprel® (in this case, the condition of patients with chronic heart failure should be carefully monitored, due to the possibility of developing their decompensation due to an increase in blood volume).
After taking the first dose of the drug, as well as when increasing its dose and/or the dose of diuretics (especially loop diuretics), it is necessary to ensure careful medical monitoring of the patient for at least 8 hours so that appropriate measures can be taken in a timely manner in case of an excessive decrease in blood pressure.
If Dilaprel® is used for the first time or at a high dose in patients with increased RAAS activity, their blood pressure should be carefully monitored, especially at the beginning of treatment, because these patients have an increased risk of excessive reduction in blood pressure.
In case of malignant arterial hypertension and heart failure, especially in the acute stage of myocardial infarction, treatment with Dilaprel® should only be started in a hospital setting.
In patients with chronic heart failure, taking the drug can lead to the development of a pronounced decrease in blood pressure, which in some cases is accompanied by oliguria or azotemia and rarely by the development of acute renal failure.
Caution should be exercised when treating elderly patients, because... They may be particularly sensitive to ACE inhibitors; monitoring of renal function is recommended during the initial phase of treatment.
In patients for whom a decrease in blood pressure may pose a certain risk (for example, in patients with atherosclerotic narrowing of the coronary or cerebral arteries), treatment should be initiated under strict medical supervision.
Caution should be exercised during physical activity and/or hot weather due to the risk of increased sweating and dehydration with the development of arterial hypotension due to a decrease in blood volume and a decrease in sodium concentration in the blood.
It is not recommended to drink alcohol during treatment with Dilaprel®.
Transient arterial hypotension is not a contraindication for continuing treatment after stabilization of blood pressure. If severe arterial hypotension develops again, the dose should be reduced or the drug discontinued.
Cases of angioedema of the face, extremities, lips, tongue, pharynx or larynx have been observed in patients treated with ACE inhibitors. If swelling occurs in the face (lips, eyelids) or tongue, or difficulty swallowing or breathing, the patient should immediately stop taking the drug.
Angioedema localized in the area of the tongue, pharynx, or larynx (possible symptoms: difficulty swallowing or breathing) can be life-threatening and requires urgent measures to relieve it: subcutaneous injection of 0.3-0.5 mg or intravenous drip of 0.1 mg of epinephrine (under the control of blood pressure, heart rate and ECG) followed by the use of corticosteroids (iv, intramuscular or orally); IV administration of antihistamines (H1- and H2-histamine receptor blockers) is also recommended, and in case of insufficiency of C1-esterase enzyme inactivators, the need to administer C1-esterase enzyme inhibitors in addition to epinephrine can be considered. The patient should be hospitalized and monitored until symptoms are completely relieved, but not less than 24 hours.
Cases of intestinal angioedema, manifested by abdominal pain with or without nausea and vomiting, have been observed in patients receiving ACE inhibitors; in some cases, angioedema of the face was simultaneously observed. If a patient develops the symptoms described above during treatment with ACE inhibitors, the possibility of developing intestinal angioedema should be considered when making a differential diagnosis.
Treatment aimed at desensitization to insect venom (bees, wasps) and concomitant use of ACE inhibitors can initiate anaphylactic and anaphylactoid reactions (for example, decreased blood pressure, shortness of breath, vomiting, allergic skin reactions), which can sometimes be life-threatening. During treatment with ACE inhibitors, hypersensitivity reactions to insect venom (for example, bees, wasps) develop faster and are more severe. If desensitization to insect venom is necessary, the ACE inhibitor should be temporarily replaced with an appropriate drug of a different class.
With the use of ACE inhibitors, life-threatening, rapidly developing anaphylactoid reactions, sometimes up to the development of shock, have been described during hemodialysis or plasma filtration using certain high-flow membranes (for example, polyacrylonitrile membranes). It is necessary to avoid the combined use of Dilaprel® and this type of membrane, for example, for urgent hemodialysis or hemofiltration. In this case, it is preferable to use other membranes or avoid taking ACE inhibitors. Similar reactions were observed with LDL apheresis using dextran sulfate. Therefore, this method should not be used in patients receiving ACE inhibitors.
Before surgery (including dentistry), it is necessary to warn the anesthesiologist about the use of ACE inhibitors.
Before starting and during therapy with ACE inhibitors, it is necessary to count the total number of leukocytes and determine the leukocyte formula.
In patients with chronic heart failure, taking Dilaprel® can lead to the development of a pronounced decrease in blood pressure, which in some cases is accompanied by oliguria or azotemia and rarely by the development of acute renal failure. Patients with malignant arterial hypertension or concomitant decompensated CHF should begin treatment in a hospital setting.
In patients with impaired liver function, the response to treatment with Dilaprel® may be either enhanced or weakened. In addition, in patients with severe liver cirrhosis with edema and/or ascites, significant activation of the RAAS is possible, so special care should be taken when treating these patients.
Monitoring laboratory parameters before and during treatment with Dilaprel® (up to 1 time per month in the first 3-6 months of treatment)
is especially important in patients with an increased risk of neutropenia - with impaired renal function, systemic connective tissue diseases or in patients receiving high doses of the drug, as well as at the first signs of infection. If neutropenia is confirmed (neutrophil count less than 2000/μl), therapy with ACE inhibitors should be discontinued.
When treating with ACE inhibitors, it is recommended to monitor renal function in the first weeks of treatment and subsequently. Particularly careful monitoring is required in patients with acute and chronic heart failure, impaired renal function, after kidney transplantation, patients with renovascular diseases, including patients with hemodynamically significant unilateral renal artery stenosis in the presence of two kidneys (in such patients, even a slight increase in serum creatinine concentration may be indicator of decreased kidney function).
Regular monitoring of serum potassium levels is recommended. Particularly careful monitoring of potassium levels in the blood serum is required for patients with impaired renal function, significant disturbances in water and electrolyte balance, and chronic heart failure.
It is recommended to monitor the complete blood count to identify possible leukopenia. More regular monitoring is recommended at the beginning of treatment and in patients with impaired renal function, as well as in patients with connective tissue diseases or in patients simultaneously receiving other drugs that can change the peripheral blood picture. Monitoring the number of leukocytes is necessary for the early detection of leukopenia, which is especially important in patients with an increased risk of its development, as well as at the first signs of infection. If symptoms associated with leukopenia appear (for example, fever, enlarged lymph nodes, tonsillitis), urgent monitoring of the peripheral blood picture is necessary. If signs of bleeding appear (tiny petechiae, red-brown rashes on the skin and mucous membranes), monitoring the number of platelets in the peripheral blood is also necessary.
If jaundice or a significant increase in the activity of liver enzymes occurs, treatment with Dilaprel® should be discontinued and the patient should be monitored medically.
Use in pediatrics
The safety and effectiveness of Dilaprel® in children and adolescents under 18 years of age has not been established.
Impact on the ability to drive vehicles and operate machinery
During treatment with Dilaprel®, it is necessary to refrain from engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions (dizziness is possible, especially after taking the initial dose of an ACE inhibitor in patients taking diuretics.