Pharmacological properties of the drug Liprazide
A combination antihypertensive drug that contains an ACE inhibitor (lisinopril) and a thiazide diuretic (hydrochlorothiazide). Lisinopril blocks the formation of angiotensin II, which reduces its vasoconstrictor effect, as well as its stimulating effect on aldosterone production in the adrenal glands. As the drug acts, blood pressure decreases, peripheral vascular resistance decreases, preload on the heart decreases, pressure in the pulmonary circulation decreases, and intrarenal circulation slightly increases. Lisinopril has virtually no effect on heart rate and IOC. Hydrochlorothiazide has diuretic and natriuric effects and potentiates the antihypertensive effect of lisinopril. The duration of the antihypertensive effect of Liprazide is 36 hours after a single dose. After oral administration, the maximum concentration of lisinopril in the blood serum is achieved after 6–7 hours. Bioavailability is 25–50%. Lisinopril practically does not bind to plasma proteins and is not metabolized in the body; it is excreted unchanged in the urine. The half-life is at least 12.6 hours, the period of complete elimination is 30 hours. The hypotensive effect is observed within 1 hour after administration and persists for 24 hours. Food intake does not affect absorption rates. In case of impaired renal function, a decrease in the excretion of lisinopril is observed (this decrease becomes clinically important when the glomerular filtration rate is below 30 ml/min). In elderly patients, the renal clearance of the drug may change. The hypotensive effect of lisinopril persists with prolonged use; with abrupt cessation of lisinopril therapy, withdrawal syndrome does not develop. Hydrochlorothiazide after oral administration is absorbed by 60–80%. The maximum concentration in blood plasma is observed after 1.5–3 hours. Hydrochlorothiazide is poorly metabolized. Excretion of hydrochlorothiazide in patients with unchanged renal function occurs almost exclusively in the urine. About 50–75% of the dose administered orally is excreted unchanged in the urine. In elderly patients and in patients with impaired renal function, the clearance of hydrochlorothiazide is significantly reduced, which leads to a significant increase in its concentration in the blood plasma. In patients with liver cirrhosis, no changes in the pharmacokinetics of hydrochlorothiazide are observed.
Price, where to buy
The price of Liprazid 10 No. 30 in Ukraine is about 64 hryvnia, and in Russia the price of a similar package is close to 306 rubles.
- Online pharmacies in UkraineUkraine
Pharmacy24
- Liprazide 20 No. 30 tablets PAT NEC "Borshchagivsky chemical and pharmaceutical plant", Kiev, Ukraine
66 UAH. order - Liprazide 10 N30 tablets PAT NEC "Borshchagivsky chemical and pharmaceutical plant", Kiev, Ukraine
50 UAH order
Side effects of the drug Liprazide
Rarely require discontinuation of treatment. Possible dry cough, dizziness, headache, feeling of fatigue, nausea, less often - orthostatic hypotension, asthenia, skin rash of allergic origin, tachycardia, abdominal pain, diarrhea, dry mouth. In some cases - Quincke's edema, mood lability, confusion, impaired renal function, impotence, hyperkalemia, increased activity of liver transaminases, increased concentrations of creatinine, bilirubin in the blood serum, neutropenia, agranulocytosis, decreased levels of hemoglobin and red blood cells. Cases of the development of acute renal failure, arthralgia, myalgia, and fever have been described. With prolonged use, hypokalemia, hyponatremia, muscle weakness, and delayed nitrogen excretion in the form of uric acid may develop.
Composition and properties of Liprazide
The drug has two forms of release - tablets containing lisinopril 10 mg and hydrochlorothiazide 12.5 mg, as well as the same components in double dosage. The mechanism of action is associated with a combination of the hypotensive effect of an ACE inhibitor and a diuretic.
Lisinopril has the following properties:
- reduces the formation of angiotensin 2, which has a strong vasoconstrictor effect;
- inhibits the synthesis of aldosterone, which retains water and sodium in the body;
- slows down the destruction of bradykinin, which dilates arteries;
- increases the content of prostaglandins, which reduce blood pressure.
As a result, changes in hemodynamic parameters occur in the body - peripheral vascular resistance, pressure in the arteries and capillaries of the lungs, load on the heart, hypertrophy of the heart muscle, tone of the vascular walls, and loss of protein in the urine during nephropathy decrease.
Lisinopril increases minute blood volume and exercise tolerance in case of circulatory failure, improves coronary blood flow in ischemia. Does not cause withdrawal syndrome.
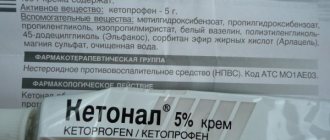
Results of biochemical blood tests before and after liprazide treatment
Hydrochlorothiazide interferes with the reabsorption of salts and water, which reduces the sensitivity of arterial walls to the action of stress hormones and promotes the dilation of small arteries. When combined with lisinopril, the hypotensive effect of this diuretic increases.
We recommend reading the article about drug treatment for stroke. From it you will learn about basic therapy for ischemic and hemorrhagic strokes, as well as drugs for the prevention of brain damage. And here is more information about thiazide diuretics.
Special instructions for the use of Liprazide
In case of renovascular hypertension (arterial hypertension), some patients, especially with bilateral renal artery stenosis or with stenosis of the artery of a single kidney, may experience a pronounced hypotensive effect, especially after taking the first dose of Liprazide, therefore the recommended initial dose of the drug is 2.5 or 5 mg (in terms of lisinopril). Taking diuretics should be stopped 2-3 days before Liprazide is prescribed. If this is not possible, the initial dose of the drug should not exceed 5 mg (in terms of lisinopril) due to the possible development of arterial hypotension. The drug is prescribed with caution to patients with gout, with impaired liver function and patients with diabetes mellitus, especially those receiving insulin or oral hypoglycemic agents. There is no experience of use in children.
Compound
- 1 tablet of Liprazide 10 contains 12.5 mg of hydrochlorothiazide and 10 mg of lisinopril. Additional substances: corn starch, mannitol, yellow iron oxide, magnesium stearate, calcium hydrogen phosphate dihydrate.
- 1 tablet of Liprazide 20 contains 12.5 mg of hydrochlorothiazide and 20 mg of lisinopril. Additional substances: corn starch, mannitol, yellow iron oxide, magnesium stearate, calcium hydrogen phosphate dihydrate.
Drug interactions Liprazide
The hypotensive effect of Liprazide is enhanced by the simultaneous administration of other antihypertensive drugs. When used simultaneously with potassium-sparing diuretics (spironolactone, triamterene, amiloride), hyperkalemia may develop, and with lithium salts, an increase in the level of lithium in the blood plasma. NSAIDs may reduce the effectiveness of Liprazide when used concomitantly. Liprazide may enhance the effects of alcohol. Hydrochlorothiazide may increase the toxicity of cardiac glycosides, antidepolarizing muscle relaxants, and reduce the effect of oral contraceptives.
Interaction
When using lisinopril with:
- lithium preparations temporarily increase the lithium in the blood and develop a toxic effect;
- anti-inflammatory non-steroidal drugs weaken the antihypertensive effect, hyperkalemia and deterioration of kidney function - this effect is usually reversible;
- Allopurinol increases the risk of renal dysfunction and leukopenia ;
- Lovastatin increases the risk of hyperkalemia ;
- Heparin, Cyclosporine, trimethoprim increases the likelihood of deterioration of kidney function and the appearance of hyperkalemia ;
- cytostatics, immunosuppressants, Procainamide increases the risk of leukopenia ;
- sympathomimetic agents may weaken the hypotonic effect of angiotensin-converting enzyme inhibitors ;
- tricyclic antidepressants, painkillers and antipsychotics increase hypotension ;
- hypoglycemic agents may reduce blood glucose
- Potassium-sparing diuretics and potassium supplements increase the risk of hyperkalemia ;
- diuretics enhance the antihypertensive effect;
- loop diuretics (Furosemide, ethacrynic acid) may develop arterial hypotension of varying severity;
- corticosteroids and estrogens may weaken the antihypertensive effect of the drug;
- antacids are likely to worsen the bioavailability of lisinopril .
Lisinopril is allowed to be prescribed together with thrombolytics, acetylsalicylic acid, β-blockers and nitrates.
When using hydrochlorothiazide with:
- non-depolarizing muscle relaxants stimulate the action of the latter and increase sensitivity to tubocurarine ;
- cardiac glycosides may increase the likelihood of side effects of the latter as a result of hypokalemia and hypomagnesemia ;
- drugs that cause fluctuations in the level of potassium in the blood (antiarrhythmic drugs of classes 1 and 3, antipsychotics and some others), the risk of cardiac arrhythmias ;
- Difluzanil increases the content of hydrochlorothiazide in the blood and decreases its hyperuricemic effect;
- anti-inflammatory non-steroidal drugs weaken the antihypertensive, natriuretic and diuretic effects of thiazides , increasing the risk of renal dysfunction;
- Diazepam, ethanol, narcotic analgesics, barbiturates, antidepressants are likely to enhance the hypotensive effect of hydrochlorothiazide ;
- lithium salts increase the content of lithium salts in the blood to toxic levels;
- pressor amines and norepinephrine weaken their effect on blood pressure;
- hypoglycemic drugs may reduce blood glucose hypoglycemia ;
- Sulfinpyrazone, Probenecid and Allopurinol may require dosage adjustment of uricosuric drugs , since hydrochlorothiazide increases uric acid in the blood;
- other antihypertensive drugs increase their effect;
- cytotoxic drugs worsen the renal excretion of the latter, as a result of which their myelosuppressive effect increases;
- salicylates enhance their toxic effect on the nervous system;
- anticholinergic drugs increase the bioavailability of thiazide-type diuretics;
- Cyclosporine increases the risk of hyperuricemia and gout;
- beta blockers and Diazoxide are likely to enhance their hyperglycemic effect;
- Amphotericin B, laxatives, motility stimulants, Calcitonin, glucocorticosteroids, adrenocorticotropic hormone worsen electrolyte imbalance;
- Vitamin D and calcium salts calcium excretion and increase its level in the blood;
- Trimethoprim increases the likelihood of developing hyperkalemia ;
- Carbamazepine may develop hyponatremia ;
- sympathomimetics may reduce the hypotensive effect;
- Digoxin increases the toxicity of the latter;
- tetracyclines or activated carbon weaken the absorption of hydrochlorothiazide ;
- Quinidine increases the possibility of ventricular fibrillation .
Analogs
Iruzid
Belupo (Croatia)
Price: from 397 rub.
Combined drug with lisinopril and hydrochlorothiazide. Available in tablets. Prescribed for the treatment of arterial hypertension.
Contraindications and side effects are similar to Liprazide.
Pros:
- Great quality
- Reduce blood pressure.
Minuses:
- May cause dizziness.
Side effects of Liprazide
According to the instructions, Liprazide can cause nausea, pain in the epigastric region, vomiting, loss of appetite, changes in stool, and dry mouth.
When taking the drug, heart rhythm disturbances, a maximum decrease in blood pressure, leukopenia, neutropenia, and anemia may occur.
Liprazide may cause dizziness, headache, increased patient fatigue, increased irritability, weakness, sleep disturbances, and convulsions.
Also, the drug can reduce the level of sodium in the blood, the level of potassium, magnesium and chlorine, reduce glucose tolerance, increase the level of calcium in the body, cholesterol, creatinine, urea.
Skin rash, itching, urticaria, bronchospasm, and Quincke's edema may occur.
When taking the drug, respiratory rhythm disturbances, pain in muscles and joints, decreased potency, and increased sweating appear.
Laboratory indicators may include leukocytosis, increased levels of urea, bilirubin, cholesterol, and decreased glucose tolerance.
In case of long-term use of Liprazide 20, gout may occur.
A decrease in the effectiveness of the drug occurs when it is used simultaneously with the following drugs:
- Cyclosporine;
- Estrogens;
- Potassium supplements, as well as potassium-sparing diuretics;
- Estrogens;
- Sodium chloride solution;
- Non-steroidal anti-inflammatory drugs.
If Liprazide is used with potassium-sparing diuretics or cyclosporine, the patient may experience hyperkalemia. In addition, the drug is not recommended for use simultaneously with lithium preparations.
During treatment, you should monitor the simultaneous use of other drugs with Liprazide to prevent side effects. In some cases, a change in the therapeutic effect may occur.
If an overdose of Liprazide 20 occurs, hypokalemia, severe arterial hypotension, angioedema, and hyponatremia may develop, the treatment of which should be carried out only under the supervision of specialists.
Contraindications
The drug is not prescribed until the age of 18, in case of individual intolerance to the components, as well as other medications from the group of ACE inhibitors. It is contraindicated in patients with the following diseases:
- severe failure of the kidneys and liver;
- angioedema;
- cessation of urine output;
- hemodialysis;
- increased calcium and uric acid levels;
- porphyria;
- disturbance of consciousness - precoma, coma;
- decompensated course of diabetes mellitus.
Hemodialysis
Caution in use and constant medical supervision are required for patients with:
- aortic valve stenosis;
- hypertrophic cardiomyopathy;
- narrowing of the arteries of the kidneys on both sides or one with a single functioning kidney;
- transplanted kidney;
- low blood pressure;
- underdevelopment of the bone marrow, hematopoietic disorders;
- diabetes mellitus;
- strict restriction of table salt in the diet;
- dehydration;
- autoimmune diseases;
- gout;
- coronary heart disease;
- cerebrovascular accidents;
- elderly patient.
Narrowing of the arteries of the kidneys, ischemic heart disease, circulatory disorders in the brain
Assessment of clinical effectiveness In recent years, approaches to the treatment of arterial hypertension (AH), based on the principles of monotherapy, have been replaced by the concept of the combined use of several antihypertensive drugs in order to achieve the target
E. P. Svishchenko, Doctor of Medical Sciences, professor, scientific supervisor; L. V. Bezrodnaya, Ph.D., Senior Researcher, Department of Hypertension, Institute of Cardiology named after. N. D. Strazhesko AMS of Ukraine, Kyiv
Evaluation of clinical effectiveness
In recent years, approaches to the treatment of arterial hypertension (AH), based on the principles of monotherapy, have been replaced by the concept of the combined use of several antihypertensive drugs in order to achieve the target level of blood pressure (BP). The results of clinical studies indicate that the majority of patients with hypertension (from 60 to 70%) require the prescription of two or more drugs to adequately reduce blood pressure [1]. The combined use of medications in small doses can not only reduce the frequency of adverse reactions caused by each of them, but also to increase the effectiveness of treatment due to the summation of the antihypertensive effect of drugs, the synergism of their action and influence on various parts of the pathogenesis of hypertension.
One of the most effective and appropriate combinations of antihypertensive drugs is the combined use of a thiazide diuretic and an angiotensin-converting enzyme (ACE) inhibitor [2]. Thiazide diuretics are still the gold standard of antihypertensive therapy, but there are a number of factors limiting their use. This is a reflex stimulation of the sympathetic-adrenal and renin-angiotensin systems due to a decrease in blood pressure and a decrease in circulating blood volume, an insufficient response to diuretics in young patients due to their initial increase in the tone of the sympathetic part of the autonomic nervous system and the predominance of the renin-angiotensin mechanism of blood pressure regulation, unfavorable metabolic changes that occur during diuretic therapy, increased insulin resistance, increased levels of glucose and uric acid in the blood plasma, the development of hypokalemia and hypomagnesemia. The simultaneous administration of diuretics with ACE inhibitors helps to avoid unwanted metabolic disorders and neutralize the activation of counter-regulatory mechanisms in response to a decrease in blood pressure and a decrease in the volume of circulating fluid. In turn, ACE inhibitors exhibit greater effectiveness when a diuretic is added to them rather than when the dose is increased beyond the standard [7]. The combination of these drugs is equally effective in both young and elderly patients due to the predominant action of one of the drugs.
It is known that the very fact of lowering blood pressure levels in the population has a beneficial effect on the prognosis of hypertension and helps reduce the risk of cardiovascular complications and mortality [3,4,5]. Large-scale studies in recent years have provided evidence that treatment outcomes—prevention and/or reduction of target organ damage—depend largely on the drugs used as antihypertensive therapy in a particular clinical setting. The advantage of ACE inhibitors is their ability to have a pronounced organoprotective effect, regardless of the antihypertensive effect [6,11].
Liprazide produced by Borshchagovsky Chemical Plant is a combination of fixed doses of the ACE inhibitor lisinopril (10 or 20 mg) and the diuretic hydrochlorothiazide (12.5 mg).
Lisinopril, a representative of the 3rd generation of ACE inhibitors, has all the advantages of drugs of this class. Its effectiveness in improving the prognosis of hypertension, not inferior to the effectiveness of older antihypertensive drugs (β-adrenergic blockers and diuretics), was shown in the STOP-2 study (The Swedish Trial in Old Patients with Hypertension, 2000) [14]. The use of lisinopril from the first day of acute myocardial infarction can improve the survival rates of patients in the early and late stages of the disease, and significantly reduce the incidence of heart failure and left ventricular dysfunction (GISSI-3, 1996) [9].
The results of the ATLAS study (Assessment of Treatment with Lisinopril and Survival, 1998) indicate that in heart failure lisinopril in high doses (32.5 or 35 mg/day) compared with its use in low doses (2.5 or 5 mg/day) day) significantly reduces the risk of overall mortality and reduces the frequency of all cases of hospitalization of patients by 13%, and for heart failure - by 24% [10].
The EUCLID (Eurodiab Controlled trial of Lisinopril in Insulin-dependent Diabetes) study provided evidence of the nephroprotective effect of lisinopril. It significantly reduces microalbuminuria in patients with type I diabetes mellitus and microalbuminuria without hypertension [11].
The combined use of the ACE inhibitor lisinopril and the diuretic hydrochlorothiazide in the drug Liprazide allows using the advantages of this combination: reducing the number of tablets used by patients along with increasing the effectiveness of therapy due to the summation of the antihypertensive effect, the influence on various mechanisms of maintaining high blood pressure and leveling the undesirable hemodynamic and humoral effects of monotherapy [7, 8]. Liprazide differs from other combination drugs with fixed doses of an ACE inhibitor and a diuretic available on the Ukrainian pharmaceutical market by the presence in its composition of a 3rd generation ACE inhibitor with a long (up to 12.5 hours) half-life.
The purpose of this study is to evaluate the clinical effectiveness of Liprazide and its effect on the daily blood pressure profile and intracardiac hemodynamics in patients with hypertension.
Material and methods
40 patients with stage II hypertension aged from 26 to 65 years were examined; the average duration of the disease was 9.5±1.2 years. The study did not include patients with symptomatic hypertension and concomitant myocardial lesions: post-infarction cardiosclerosis, persistent atrial fibrillation, severe left ventricular systolic dysfunction (ejection fraction
Daily blood pressure monitoring and cardiohemodynamic studies were performed after a 7-day drug-free period and after a 4-week course of therapy.
Liprazide produced by Borshchagovsky Chemical Plant was used as an antihypertensive drug. Treatment began with the administration of Liprazide-10 containing 10 mg of lisinopril and 12.5 mg of hydrochlorothiazide. If there was insufficient reduction in blood pressure, Liprazide-20 containing 20 mg of lisinopril and 12.5 mg of hydrochlorothiazide was used after two weeks. The goal of treatment is complete normalization of blood pressure (90 mm Hg and its reduction by less than 10 mm Hg.
Daily blood pressure monitoring was carried out using an ABPM-2 device (Meditech, Hungary); Data were recorded from 7 a.m. to 10 p.m. every 15 minutes, and from 10 p.m. to 7 a.m. every 30 minutes. We analyzed the average daily, average day and average night systolic blood pressure (SBP) and DBP, blood pressure variability (BP), daily index (DI), time index (TI) and T/P ratio - the ratio of the residual antihypertensive effect to the peak, the speed and magnitude of the morning increase in blood pressure from 4 to 10 am.
Indicators of intracardiac hemodynamics: end-systolic (ESO) and end-diastolic (EDV) volumes of the left ventricle, ejection fraction (EF), thickness of the interventricular septum (IVS) and the posterior wall of the left ventricle (PVS) during diastole were determined using two-dimensional echocardiography on Sonoline device (Siemens, Germany).
Statistical processing of the results was carried out on a computer using statistical programs Microsoft Exel 97 and Student's test.
Research results and discussion
Analysis of episodic blood pressure measurements showed that after 2 weeks, Liprazide-10 therapy was effective in 28 (72%) of 40 patients: a good treatment effect was observed in 22, satisfactory in 6. Patients in whom the achieved blood pressure did not normalize, after 2 Liprazide-20 was prescribed for weeks of therapy. At the end of the study, the treatment was effective in 37 (93%) patients: good effect - in 27 (68%), satisfactory - in 10 (25%) patients.
By the end of the observation period, the number of effectively treated patients increased, which was due to both an increase in the dose of lisinopril (Liprazide-20) in some patients and, obviously, an increase in the antihypertensive effect of the drug by the 4th week of therapy, which is inherent in all ACE inhibitors.
During the therapy, a positive clinical effect was observed in the form of a decrease or disappearance of headaches, dizziness, shortness of breath, pain in the heart, and decreased ability to work (Table 1).
Tolerability of Liprazide-10 and Liprazide-20 was good; only one patient complained of a slight cough during treatment, apparently associated with the bradykinin-accumulating effect of ACE inhibitors, but its occurrence did not require discontinuation of the drug.
When analyzing data from 24-hour blood pressure monitoring, it was revealed that the average daily systolic and diastolic blood pressure at the end of a 4-week course of Liprazide therapy decreased from 158.4±1.4/98.6±1.7 to 132.5±1.9/85. 6±2.1 mmHg Art. (R
The decrease in blood pressure under the influence of Liprazide was not accompanied by a reflex increase in heart rate: before treatment - 71.4±0.8 per minute during the day and 63.4±0.7 per minute at night, after 4 weeks of therapy - 69±0.6 and 62.5±0.8 per minute, respectively.
Treatment with Liprazide led to a significant decrease in “pressure load”, determined by the time index: IV SBP decreased by 68% per day, by 66% per day, and by 69% per night. The DBP time index at the end of the course of therapy decreased by 70% per day, during wakefulness - by 72% and by 69% during sleep (p
During Liprazide therapy, there was a decrease in the initially elevated variability of SBP and DBP during wakefulness and sleep (Fig. 1).
After 4 weeks of treatment, in the group of patients with increased blood pressure variability, daytime SBP variability decreased from 18.7 ± 0.4 to 14.6 ± 0.5 mm Hg. Art. (R
Violations of the circadian index were detected in 54% of patients. Liprazide therapy contributed to the normalization of disturbances in the daily blood pressure profile in the majority of patients, which before treatment had a circadian pattern (with an insufficient decrease in blood pressure at night) or an “over-dipper” (with an excessive decrease during this period). In the group of non-dipper patients (18 people), the daily SBP and DBP index increased respectively from 6.8±3.1% and 7.2±3.0% to 12.3±2.8% and 11.8±2 .5% (p
Analysis of the dynamics of the absolute increase in blood pressure in the morning and the rate of its increase during this period (from 4 to 10 a.m.) before and after treatment showed that Liprazide reduces the value of the morning increase in SBP by 63% (from 45.6 ± 5.2 to 16.8±6.3 mmHg, p
The initially increased rate of morning increase in blood pressure under the influence of Liprazide therapy decreased for SBP from 26.2±2.4 to 8.7±1.7 mm Hg. Art. per hour (r
It is known that an increase in blood pressure in the morning is associated with a risk of developing complications from the cardiovascular system: myocardial infarction, stroke and sudden death [12,13]. Therefore, the ability to reduce the morning increase in blood pressure is an important characteristic of an antihypertensive drug, depending on the duration of its action.
The duration of the antihypertensive effect of Liprazide after a single dose was judged by the value of the T/P coefficient, which characterizes the ratio of the residual effect of the drug to the maximum. After 4 weeks of treatment with Liprazide-10, the T/R ratio for SBP was 69%, for DBP - 67%. Liprazide-20 had a longer-lasting antihypertensive effect. For SBP while taking Liprazide-20, the T/R ratio was 74%, for DBP - 73%. Consequently, the high residual antihypertensive effect of Liprazide indicates its ability to have a pronounced protective effect on the patient’s body in the early morning hours, preventing a significant increase in blood pressure during this period.
A study of the effect of Liprazide on intracardiac hemodynamics showed a tendency to a decrease in the size of the left ventricle and an increase in the ejection fraction (the difference is not significant) (Table 2).
No significant changes in the thickness of the walls of the left ventricle were detected. The lack of regression of LV hypertrophy after 4 weeks during Liprazide therapy is associated with an insufficiently long observation period. It is believed that reliable dynamics of indicators can be obtained after 3 months of treatment.
During a biochemical blood test, no changes in the studied parameters were detected after treatment (Table 3).
Liprazide did not affect the content of K+ and Na+ in the blood plasma. There were also no changes in the levels of glucose, creatinine, uric acid, cholesterol and triglycerides after treatment.
Treatment with Liprazide did not have a significant effect on the parameters of general blood and urine tests. There was a tendency to increase daily diuresis, which is associated with a moderate diuretic effect of the drug.
Thus, analysis of 24-hour monitoring indicators showed that Liprazide reliably controls blood pressure levels during the day and night hours. Along with a decrease in the absolute values of SBP and DBP, Liprazide reduces the magnitude and speed of the morning increase in blood pressure, its variability, and normalizes the initially disturbed circadian rhythm of blood pressure.
After a single dose of Liprazide, a long-term antihypertensive effect is observed, determined by the value of the T/P ratio. Liprazide-10 has a residual antihypertensive effect of 69% of the maximum for SBP and 67% for DBP, which indicates the drug’s ability to cause a smooth and prolonged decrease in blood pressure throughout the day.
The results of a study of the clinical effectiveness of Liprazide in patients with hypertension showed that the drug is an effective antihypertensive agent, is well tolerated by patients and has a positive effect on the clinical course of the disease.
Mode of application
When calculating the dosage, the amount of lisinopril or hydrochlorothiazide previously used in monotherapy should be taken into account.
At the beginning of treatment with Liprazide, the instructions for use recommend taking 5-10 mg/day. lisinopril, then change the dosage if necessary.
A stable therapeutic effect is formed after 2-4 weeks of regular use. The recommended dose for prevention is 20 mg/day.
The drugs are prescribed taking into account the doses of lisinopril and hydrochlorothiazide. The dose is selected personally in accordance with the therapeutic effect.
During pregnancy and breastfeeding
The drug should not be used while pregnant. If the use of ACE inhibitors cannot be discontinued, then women planning motherhood should be switched to alternative safe drugs. In cases where pregnancy occurs during Liprazide therapy, the use of the medicine should be stopped immediately and other drugs approved during this period should be prescribed.
Breastfeeding women should refrain from therapy, since it has not been reliably established whether or not the active substance can pass into milk.
Overdose
Due to the intake of large amounts of drugs, patients may develop hypotension, shock, electrolyte disorders, renal dysfunction, bradycardia, anxiety, hyperventilation, etc.
To eliminate the pathology, supportive and symptomatic therapy is used, since there is no antidote to the drug. If a little time has passed after taking Liprazide, then standard measures are used to clear the drug: washing, inducing vomiting, administering enterosorbents. Hemodialysis is also used.