Indications for use
Captopril is widely used to test renal function under stress conditions using scintigraphy.
Captopril is used as a single drug (contains only captopril) and in combination with other drugs, such as thiazide diuretics, to treat hypertension and heart failure. Combination with diuretics provides synergistic effects that lead to better reduction in blood pressure levels.
To prolong the life of patients with severe CHF, a combination with cardiac glycosides and beta-blockers is possible and indicated.
Other indications for the use of captopril are short-term treatment (4 weeks) after myocardial infarction and diabetic nephropathy with macroproteinuria in patients with type 1 diabetes mellitus.
Advantages of the drug
Captopril is a fairly effective drug used for heart failure and hypertension.
The drug has the following advantages:
- decrease in pressure indicators;
- lack of influence on potency in men;
- the possibility of using the medicine for elderly patients;
- the development of nephropathy is suppressed;
- the development of cancer is minimal;
- antioxidant effect;
- Death from heart failure when using the drug is extremely rare.
In addition, it is worth noting that Captopril has a fairly low price, and you can find it in any pharmacy.
Mechanism of action
Captopril leads to a decrease in the formation of angiotensin II from angiotensin I due to ACE inhibition. Reduced production of angiotensin II causes a weakening of blood vessel tone and, consequently, a decrease in blood pressure.
In addition, a decrease in the level of angiotensin II leads to a decrease in the release of aldosterone from the adrenal cortex and, thus, captopril affects the water balance (renin-angiotensin-aldosterone system).
Mechanism of action of ACE inhibitors
Captopril reduces the angiotensin-mediated mitogenic effect on cardiac cells, which leads to adverse changes (myocardial remodeling), especially after a “heart attack”.
Varieties, names, composition
Currently, the drug is available in several of the following varieties:
- Captopril-Vero;
- Captopril Hexal;
- Captopril Sandoz;
- Captopril-AKOS;
- Captopril-Acri;
- Captopril-Ros;
- Captopril-Sar;
- Captopril-STI;
- Captopril-UBF;
These varieties of the drug actually differ from each other only by the presence of an additional word in the name, which reflects the abbreviation or well-known name of the manufacturer of a particular type of drug.
Otherwise, the varieties of the drug are practically no different from each other, since they are produced in the same dosage form, contain the same active substance, etc. Moreover, often even the active substance in the drug varieties is identical, since it is purchased from large manufacturers China or India.
The differences in the names of the varieties of Captopril are due to the need for each pharmaceutical company to register the drug they produce under an original name that is different from others.
Side effects
Most of the side effects of captopril are associated with slow elimination (due to ACE inhibition) and accumulation of bradykinin. These include skin reactions such as exanthema and urticaria, as well as angioedema. Extremely severe allergic and skin reactions are rare.
Respiratory side effects include dry cough, hoarseness and sore throat. Also, very rarely, asthma attacks and dyspnea may occur.
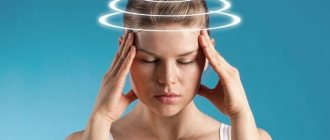
An excessive decrease in blood pressure may occur as a result of the underlying effect of captopril. Because of this, dizziness, headache, and drowsiness are observed. Serious cardiovascular side effects such as angina, myocardial infarction and syncope have been reported only in isolated cases.
Interference with the regulation of water and electrolyte balance can lead to functional renal failure. Proteinuria (the presence of protein in the urine above normal) was rarely observed.
The use of captopril during pregnancy causes growth and bone development disorders in the fetus, which are directly associated with an increase in infant mortality, therefore captopril is contraindicated during pregnancy and should be replaced with other drugs.
Captopril
Arterial hypotension
In patients with arterial hypertension, when using captopril, severe arterial hypotension is observed only in rare cases. The likelihood of developing this condition increases with increased fluid loss and hyponatremia (for example, after intensive treatment with diuretics, restriction of sodium intake, in patients on dialysis, and in patients with diarrhea or vomiting).
Captopril should be prescribed with caution to patients on a low-salt or salt-free diet. Circulating blood volume and blood sodium levels should be adjusted before captopril is prescribed. The possibility of a sharp decrease in blood pressure can be minimized by first withdrawing (4-7 days before) the diuretic or increasing sodium chloride intake (about a week before starting treatment), or by prescribing low doses of captopril at the beginning of treatment (6.25-12 .5 mg/day). Renal function should be regularly monitored before and during treatment with captopril. Excessive reduction in blood pressure due to antihypertensive medications may increase the risk of myocardial infarction or stroke in patients with coronary heart disease or cerebrovascular disease. If arterial hypotension develops, the patient should take a horizontal position with legs elevated.
Intravenous administration of 0.9% sodium chloride solution may be required.
In patients with CHF, a transient decrease in blood pressure by more than 20% of the initial value is observed in approximately half of the cases. The degree of reduction in blood pressure is maximum in the early stages of treatment (after taking the first few doses of captopril) and stabilizes within one to two weeks from the start of treatment. Blood pressure usually returns to baseline without a decrease in therapeutic efficacy within two months. In patients with CHF, treatment should begin with low doses of captopril (6.25-12.5 mg/day) under medical supervision. Increasing the dose of captopril should be done with extreme caution. Transient arterial hypotension in itself is not a reason to discontinue treatment. In cases where arterial hypotension becomes stable, the dose should be reduced and/or discontinued use of the diuretic and/or captopril.
Aortic or mitral stenosis/hypertrophic obstructive cardiomyopathy
Like all drugs that have a vasodilating effect, ACE inhibitors should be used with extreme caution in patients with left ventricular outflow tract obstruction. In case of hemodynamically significant obstruction, the use of captopril is not recommended.
Renal dysfunction
Some patients with kidney disease, especially those with severe renal artery stenosis, experience increases in serum urea nitrogen and creatinine concentrations after lowering blood pressure. This increase is usually reversible when captopril therapy is discontinued. In these cases, it may be necessary to reduce the dose of captopril and/or discontinue the diuretic.
With long-term use of captopril, approximately 20% of patients experience an increase in serum urea and creatinine concentrations by more than 20% compared to normal or baseline values.
In less than 5% of patients, especially with severe nephropathy, treatment discontinuation is required due to an increase in creatinine concentration.
Renovascular hypertension
Patients with bilateral renal artery stenosis or stenosis of the artery of a solitary kidney have an increased risk of developing arterial hypotension and renal failure when using ACE inhibitors. Renal failure may initially manifest itself as only slight changes in plasma creatinine levels. The use of captopril in such patients is not recommended.
Kidney transplant
There is no experience with the use of captopril in patients who have recently undergone kidney transplantation. Therefore, the use of captopril in such patients is not recommended.
Proteinuria
When using captopril, 0.7% of patients experienced proteinuria greater than 1000 mg per day. In 90% of cases, proteinuria occurred in patients with impaired renal function, as well as when using high doses of captopril (more than 150 mg per day). Approximately 20% of patients with proteinuria developed nephrotic syndrome. In most cases, proteinuria disappeared or decreased in severity after taking captopril within 6 months, regardless of whether the drug was stopped or not. Renal function indicators (blood urea nitrogen and creatinine concentrations) in
patients with proteinuria were almost always within normal limits. In patients with kidney disease, the protein content in the urine should be determined before starting treatment and periodically throughout the course of therapy.
Liver dysfunction
In rare cases, the use of ACE inhibitors has been accompanied by the development of a syndrome that begins with the appearance of cholestatic jaundice or hepatitis and progresses to fulminant liver necrosis, sometimes with death. The mechanism of development of this syndrome is unknown. If a patient receiving ACE inhibitor therapy develops jaundice or a significant increase in liver enzyme activity, captopril treatment should be discontinued and appropriate adjuvant therapy should be instituted. The patient should be under appropriate supervision.
Neutropeia/agranulocytosis/thrombocytopeia/anemia
In patients taking ACE inhibitors. cases of neutropenia/agranulocytosis, thrombocytopenia and anemia were noted. Neutropenia is rare in patients with normal renal function and no other abnormalities. In renal failure, simultaneous administration of captopril and allopurinol led to neutropenia.
Captopril should be used with extreme caution in patients with systemic connective tissue diseases (systemic lupus erythematosus, scleroderma, etc.) taking immunosuppressants, allopurinol or procainamide, or a combination of these complicating factors, especially if there are pre-existing renal dysfunction.
In 13% of cases, neutropenia resulted in death. In almost all cases, death was observed in patients with connective tissue diseases, renal or heart failure, while taking immunosuppressants, or a combination of both of these factors.
Due to the fact that the majority of fatal cases of neutropenia due to ACE inhibitors developed in such patients, their white blood cell count should be monitored before starting treatment, in the first 3 months - every 2 weeks, then every 2 months. In all patients, the number of leukocytes in the blood should be monitored monthly in the first 3 months after starting captopril therapy, then every 2 months. If the number of leukocytes is below 4000/μl, a repeat general blood test is indicated; below 1000/μl, the drug is stopped while monitoring the patient continues. Typically, restoration of the number of neutrophils occurs within 2 weeks after discontinuation of captopril.
Some patients developed serious infectious diseases, which in some cases did not respond to intensive antibiotic therapy. When using captopril in patients with a high risk of neutropenia/agranulocytosis, regular monitoring of the number of leukocytes in the blood is recommended. Patients should be warned to seek immediate medical attention if any signs of an infectious disease (eg, fever, sore throat) occur.
Hypersensitivity reactions/agioedema
Rare cases of angioedema of the face, extremities, lips, tongue, vocal folds and/or larynx have been observed with the use of ACE inhibitors, including captopril. Angioedema may develop at any time during treatment. If angioedema develops, you should immediately stop taking captopril and carefully monitor the patient's condition until symptoms disappear completely.
If the swelling is localized to the face, no special treatment is usually required (antihistamines can be used to reduce the severity of symptoms). Even in cases where only swelling of the tongue is observed without the development of respiratory distress syndrome, patients may require long-term observation, since therapy with antihistamines and corticosteroids may not be sufficient.
Angioedema, associated with swelling of the larynx and tongue, can be fatal in very rare cases. If the swelling spreads to the tongue, pharynx or larynx and there is a threat of developing airway obstruction, 0.3-0.5 ml of a 0.1% solution of epinephrine (adrenaline) should be immediately administered subcutaneously and/or the airway should be ensured ( intubation or tracheostomy). In rare cases, during therapy with ACE inhibitors, intestinal edema (angioedema of the intestines) has developed, which is manifested by abdominal pain in combination with or without nausea and vomiting, sometimes without previous angioedema of the face and with normal levels of Cl-esterase. Diagnosis is made using abdominal computed tomography, ultrasound, or surgery. Symptoms disappeared after stopping the ACE inhibitors. The possibility of developing intestinal edema must be taken into account when carrying out the differential diagnosis of abdominal pain in patients taking ACE inhibitors.
Patients with a history of angioedema not associated with ACE inhibitors may be at greater risk of developing angioedema during ACE inhibitor therapy.
In representatives of the Negroid race, cases of the development of angioedema when using ACE inhibitors were observed with a higher frequency compared to representatives of other races.
An increased risk of angioedema was observed in patients concomitantly taking ACE inhibitors and drugs such as mTOR inhibitors (temsirolimus, sirolimus, everolimus), dipeptidyl peptidase type IV inhibitors (sitagliptin, saxagliptin, vildagliptin, linagliptin), estramustine, neutral endopeptidase inhibitors (racecadotril). , sacubitril) and tissue plasminogen activators.
Anaphylactoid reactions during desensitization with an allergen from Hymenoptera venom
In rare cases, during therapy with ACE inhibitors, life-threatening anaphylactoid reactions were observed in patients undergoing desensitization with an allergen from the venom of Hymenoptera. In such patients, these reactions were prevented by temporarily stopping ACE inhibitor therapy before desensitization began. The use of captopril should be avoided in patients receiving bee venom immunotherapy.
Anaphylactoid reactions during low-density lipoprotein apheresis (LDL apheresis)
Life-threatening anaphylactoid reactions have rarely been observed in patients taking ACE inhibitors during LDL apheresis using dextran sulfate. The development of these reactions can be prevented by temporarily stopping the inhibitor
ACE before each LDL apheresis procedure.
Hemodialysis using high-flow membranes
When performing hemodialysis in patients receiving ACE inhibitors, the use of high-flow polyacrylonitrile dialysis membranes (for example, AN69®) should be avoided, since in such cases the risk of developing anaphylactoid reactions increases. In such cases, it is necessary to use a different type of dialysis membrane or use antihypertensive drugs of other classes.
Diabetes
In patients with diabetes mellitus receiving oral hypoglycemic agents or insulin while using ACE inhibitors, blood glucose concentrations should be regularly monitored.
Patients taking oral hypoglycemic agents or insulin should be informed before starting the use of ACE inhibitors of the need to regularly monitor blood glucose concentrations (hypoglycemia), especially during the first month of simultaneous use of these drugs.
Cough
When taking ACE inhibitors, a characteristic cough is often observed. As a rule, the cough is non-productive, constant and stops after discontinuation of the drug. Cough associated with the use of ACE inhibitors. should be taken into account in the differential diagnosis of dry cough.
Surgery/general anesthesia
During major surgical operations, as well as when using general anesthesia agents that have an antihypertensive effect, patients taking ACE inhibitors may experience an excessive decrease in blood pressure (since captopril blocks the formation of angiotensin II, caused by compensatory release of renin). In such cases, to correct low blood pressure, measures aimed at increasing the volume of circulating blood are used.
Hyperkalemia
In some cases, against the background of the use of ACE inhibitors, incl. captopril, an increase in serum potassium levels is observed.
Risk factors for the development of hyperkalemia are renal failure, old age (over 65 years), diabetes mellitus, some concomitant conditions (decrease in blood volume, acute heart failure in the stage of decompensation, metabolic acidosis), simultaneous use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene or amiloride), as well as potassium preparations, potassium-containing table salt substitutes and other drugs that increase the level of potassium in the blood plasma (such as heparin, tacrolimus, cyclosporine; drugs containing cotrimoxazole [trimethoprim + sulfamethoxazole]).
The use of potassium supplements, potassium-sparing diuretics, or potassium-containing table salt substitutes, especially in patients with impaired renal function, can lead to a significant increase in serum potassium levels. Hyperkalemia can cause serious heart rhythm disturbances, sometimes fatal. It is recommended to avoid the simultaneous use of potassium-sparing diuretics and potassium supplements. If it is necessary to simultaneously use captopril and the drugs listed above containing potassium or increasing the potassium content in the blood plasma, caution should be exercised and the potassium content in the blood serum should be regularly monitored.
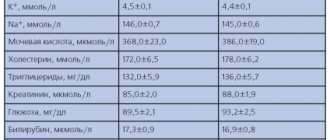
Hypokalemia
When using ACE inhibitors simultaneously with thiazide diuretics, the risk of hypokalemia cannot be excluded. Therefore, in such cases, regular monitoring of potassium levels in the blood should be carried out during therapy.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
The simultaneous use of drugs from different groups that act on the RAAS is not recommended (double blockade of the RAAS), since it has been associated with an increased incidence of side effects such as arterial hypotension, hyperkalemia, and decreased renal function (including acute renal failure). The simultaneous use of ACE inhibitors with medicinal products containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
In cases where the simultaneous administration of two drugs acting on the RAAS is necessary, their use should be carried out under the supervision of a physician with extreme caution and with regular monitoring of renal function, blood pressure and electrolyte levels in the blood plasma.
Lithium preparations
The simultaneous use of captopril and drugs containing lithium is not recommended due to the risk of potentiating the toxicity of the latter.
Ethnic differences
ACE inhibitors are less effective in blacks than in Caucasians, which may be due to the higher prevalence of low renin activity in blacks.
Other
When taking captopril, a false-positive urine test for acetone may occur.
Interactions
Captopril enhances the hypoglycemic effect of insulin and oral antidiabetic agents, and also enhances the effect of immunosuppressants.
By interfering with the water and electrolyte balance, captopril retains ions in the body, which should be taken into account when using potassium-sparing diuretics and lithium preparations together.
In combination with other antihypertensive drugs, the dose must be adjusted correctly to prevent an excessive decrease in blood pressure.
Instructions for use
Captopril should be taken one hour before meals. You should not bite the tablet, but swallow it whole, do not chew it. You need to take the tablet with at least half a glass of water.
The number of doses and doses should be determined individually after tests and appropriate research.
According to the instructions, the dosage of the drug depends on certain disorders and diseases. If arterial hypertension is observed, then Capriptol is usually drunk twice a day, 250 ml, then it is increased to achieve a positive effect. However, more than 100 ml cannot be consumed. However, in some cases, when there is no effect and persistent hypertension is present, the drug is prescribed 75 mg twice a day.
In case of heart failure, a minimum dosage of 2-3 times a day is first prescribed. Its increase is also gradual, however, not earlier than the tenth day of administration. Usually the maximum daily dosage here is 50-75 ml. If there is no effect, then it is doubled. It is also important to know that Captopril is most often prescribed with diuretics so that the effect is stronger.
For elderly patients, dosage determination is individual. Beginning the course of treatment is mandatory with a minimum dose. Its increase occurs only when necessary.
Captopril recipe in Latin
Captopril is available in pharmacies in the form of 12.5 tablets; 25, 50 and 100 mg. Let's, for example, write out a prescription for captopril in Latin 25 mg 30 tablets (more details about the recipe for tablets in Latin and the recipe in Latin). We will prescribe it to be taken urgently if there is a persistent increase in blood pressure under the tongue.
Rp.: Captoprili 25 mg Dtd N 30 in tab. S. Urgently if there is a persistent increase in blood pressure under the tongue.
Contraindications
Absolute contraindications to the use of Captopril are the following:
- liver failure;
- kidney dysfunction;
- progressive renal artery stenosis;
- hypotension;
- cardiogenic shock;
- mitral valve stenosis;
- after a kidney transplant;
- aortic stenosis;
- primary hyperaldosteronism;
- hyperkalemia;
- pregnancy;
- age under 18;
- hereditary angioedema;
- breast-feeding;
- individual intolerance.
There are exceptions when it is necessary to see a doctor. For example, with leukopenia, cerebral ischemia, thrombocytopenia, diabetes mellitus, being on hemodialysis, kidney transplant, age over 65 years, hypertrophic cardiomyopathy, etc.
Reviews
Almost 100% of reviews about the drug are positive. This is explained by the high quality and effectiveness of the medicine for the diseases that it eliminates. Reviews contain information about the speed and quality of blood pressure reduction with this drug.
The drug is an indispensable medicine for blood pressure. The product does not exclude negative reviews. They are associated with side effects that have caused people to stop taking the medication.
Use in childhood
Captopril for high blood pressure should not be prescribed to children under 18 years of age. If it is not possible to replace Captopril with another drug, the doctor prescribes the minimum possible dosage to eliminate the risk of developing adverse reactions in the body. Children are prescribed 1-1.5 mg of the drug per 1 kg of body weight.
For children, the medicine is prescribed as a last resort in a minimal dosage.
Overdose
In case of an overdose of the drug, the following symptoms are observed:
- Hypotension
- A sharp decrease in pressure;
- State of shock;
- Being in a stupor;
- Heart rate decreases (less than 60 beats per minute);
- Poor blood circulation in the brain;
- Kidney failure;
- Angioedema.
In order to eliminate the symptoms of an overdose, it is necessary to prohibit taking the drug, and also to rinse the stomach. In order to replenish blood volume, it is necessary to administer saline. intravenous solution. Symptomatic therapy is also carried out to eliminate symptoms. This therapy helps support the functioning of important organs for a person. Adrenaline is used for this. If you need to take the drug with other drugs, you should pay attention to drugs that increase potassium in the blood.
You should be careful with painkillers and alcohol, as Captopril significantly enhances their effect. Many drugs significantly enhance the effect of Captopril. These include diuretics and vasodilators. Because of them, blood pressure may decrease.
When taking Captopril with immune drugs, there is an increased risk of a decrease in the level of white blood cells, as well as the occurrence of other diseases.
Pharmacological properties of the drug Captopril
Pharmacodynamics . Captopril is the first synthetic ACE inhibitor. By blocking the conversion of angiotensin I to angiotensin II, it has a vasodilating effect, thereby reducing peripheral vascular resistance (afterload), wedge pressure in the pulmonary capillaries (preload) and pressure in the pulmonary vessels; increases IOC and exercise tolerance. With long-term use, captopril reduces the severity of left ventricular myocardial hypertrophy. Reduces the tone of the efferent arterioles of the glomeruli of the kidneys, thereby improving intraglomerular hemodynamics and preventing the development of diabetic nephropathy. Pharmacokinetics . When taken orally, the drug is quickly and almost completely (at least 75%) absorbed into the gastrointestinal tract. In the presence of food, bioavailability is reduced by 30–40%. The maximum concentration in blood plasma is reached after 30–90 minutes. Protein binding, predominantly albumin, is 25–30%. Penetrates through histohematic barriers, including the blood-brain barrier, and crosses the placenta. Metabolized in the liver. The half-life is less than 3 hours and increases with renal failure. It is excreted mainly by the kidneys in the form of metabolites and unchanged (up to 50%). Within 24 hours, up to 25% of the drug is eliminated. The maximum decrease in blood pressure after taking the drug orally is observed after 60–90 minutes. The duration of the hypotensive effect is dose-dependent and reaches optimal values within several weeks.
Use during pregnancy and lactation
The drug should not be taken by pregnant women. If a woman finds out about pregnancy after prescribing a course, she must inform her doctor, who will select another method of therapy that is harmless to the intrauterine development of the child.
Captopril tablets for blood pressure should not be taken during lactation, since the main component of the drug passes into breast milk, which can negatively affect the development of the baby. If treatment with Captopril cannot be avoided, the woman should stop breastfeeding during treatment.