Iron preparations for low hemoglobin are suitable for the treatment of anemia when the active substance content is more than 30 mg per tablet. The rating of the best tablets includes Tardiferon, it has a protective component, and iron is slowly released. Long-acting medication Ferretab prolong and Aktiferrin are prescribed during pregnancy. Sorbifer Durules is indicated for elderly patients.
To prevent iron deficiency, you can use vitamin complexes (Special dragee Merz, Fenyuls), dietary supplements (Aloe syrup with iron, Hematogen). If absorption in the intestine is impaired and if a rapid increase in hemoglobin is necessary, ampoules of Ferinject, Likferr 100 are prescribed. Drops and syrups are recommended for children - Maltofer, Aktiferrin.
What is anemia?
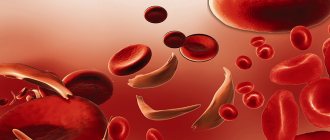
Anemia is a health problem in which the level of hemoglobin in the blood decreases.
Most often, the number of red blood cells decreases in parallel. Popularly, this pathology is also called “anemia.” Low hemoglobin is not an independent disease. It is the result of an underlying disease, therefore, if anemia is detected in a patient, the doctor is obliged to prescribe a comprehensive examination.
Concepts of pseudoanemia and hidden anemia:
Pseudoanemia is the entry of tissue fluid into the bloodstream during the resorption of edema.
Hidden anemia is the result of the loss of a significant part of the fluid composition of the blood due to dehydration (can be caused by diarrhea, vomiting, hyperhidrosis). In this situation, the blood begins to thicken, so laboratory analysis shows that the number of red blood cells and hemoglobin is normal, even if this is not the case.
Severity of anemia:
Based on severity, anemia is classified into:
- light
. Hemoglobin level is more than 100 g/l, erythrocytes - more than 3 T/l; - average
_ Hemoglobin level from 66 to 100 g/l, erythrocytes - from 2 to 3 T/l; - heavy
_ Hemoglobin level is less than 66 g/l.
Classification of anemia:
All anemias manifest themselves differently. Taking into account the cause of the pathological condition and its symptoms, there are four main types:
- posthemorrhagic anemia (caused by chronic/acute blood loss);
- hemolytic anemia (develops due to the destruction of red blood cells). This group includes hereditary hemolytic anemias: with a lack of glucose-6 phosphate dehydrogenase;
- thalassemia;
- sickle cell;
- Minkowski-Shoffar;
According to the color indicator of blood, anemia can be:
- normochromic
(hemoglobin is normal). This group includes hemolytic and posthemorrhagic anemia; - hyperchromic
(hemoglobin increased). These include folate deficiency and B12 deficiency anemia; - hypochromic
(hemoglobin is low). This refers to thalassemia, iron deficiency and chronic posthemorrhagic anemia.
Based on the diameter of red blood cells, anemia can be:
- normocytic
(almost all hemolytic and acute posthemorrhagic anemia); - megaloblastic
(B12-deficiency anemia); - macrocytic
(folate deficiency, hemolytic disease of the newborn); - microcytic
(chronic posthemorrhagic anemia).
Based on the iron content in the blood serum, anemia is divided into:
- normosideremic
(acute posthemorrhagic anemia); - hyposideremic
(chronic posthemorrhagic and iron deficiency anemia, thalassemia); - hypersideremic
(hemolytic and B12-deficiency anemia).
How to take it correctly
The dosage of iron supplements for low hemoglobin is prescribed by a doctor at the rate of 3-4 milligrams per 1 kilogram of body weight, which on average ranges from 100 to 300 milligrams per day. During treatment, the daily dose may be reduced in the following cases:
- with severe gastrointestinal disorders;
- with intolerance;
- for symptoms of intoxication.
In most cases, iron-containing preparations should be consumed between meals (in the first half of the day), since the effectiveness of iron absorption is affected by foods containing certain salts, acids and alkalis.
On 10-15 days after the start of treatment, a blood test is performed to check the effectiveness of the prescribed drugs, the results of which for a normal condition should look like this:
- increase in the number of reticulocytes by 2 times;
- increase in hemoglobin level by 10 g/l.
After 1-2 months, the hemoglobin level should return to normal along with the disappearance of symptoms of anemia (fatigue, brittle nails, hair loss). In this case, treatment should continue for another 2-4 months to achieve normal serum and cellular ferritin levels.
Causes of anemia
Common causes of low hemoglobin are:
- large blood loss;
- disruption of the formation of new blood cells;
- activation of pathological processes of blood destruction.
Causes of posthemorrhagic anemia:
Acute posthemorrhagic anemia is the result of the loss of a large amount of blood in a minimal period of time.
The chronic form of this disease is caused by:
- prolonged blood loss;
- polyps, hernias and stomach ulcers;
- kidney diseases;
- malignant tumor neoplasms;
- uterine bleeding;
- disorders of the blood clotting system;
- liver failure, cirrhosis.
Normal for men
In healthy adult men, hemoglobin should be at a level of 130 – 160 g/l. This concentration is optimal for providing tissues with oxygen, maintaining good health and working ability of the stronger sex. If a man is physically active (plays sports, heavy physical work), his hemoglobin may even go slightly beyond acceptable limits, which, in the absence of signs of any pathological processes, is regarded as a variant of the norm, but only a doctor should make such an assessment.
What causes hemolytic anemia
All hemolytic anemias occur if “old” red blood cells begin to destroy faster than new ones can form.
The sickle cell form is caused by the synthesis of a defective hemoglobin molecule. The emerging defective molecules form peculiar crystals that stretch the red blood cell, causing the latter to take on the shape of a sickle. Sickle erythrocytes are non-plastic. It leads to increased blood viscosity and blockage of small blood vessels. With their sharp ends they can destroy each other.
Thalassemia is a hereditary disease. It occurs due to a decrease in the rate of hemoglobin formation. Hemoglobin that is not fully formed is unstable. It resembles small inclusions that give the red blood cell the appearance of a target cell.
Deficiency anemias and their causes:
Iron deficiency anemia develops for reasons such as:
- lack of iron/increased need for iron (this is why degree 1 anemia is often diagnosed in premature babies and pregnant women);
- chronic blood loss;
- problems associated with the absorption of iron from the gastrointestinal tract, its transportation and disposal.
B12 deficiency anemia is caused by a lack of vitamin B12. The disease can be caused by poor nutrition (refusal to eat meat) or disruption of the absorption of cyanocobalamin in the gastrointestinal tract (parasites, diseases of the small intestine, stomach). Also, symptoms of B12 deficiency anemia can appear while taking hormonal drugs and anticonvulsants.
Folate deficiency anemia is a consequence of a lack of vitamin B9. It is usually observed in pregnant and lactating women, cancer patients, teenage children, premature newborns, liver disease, alcohol abuse, etc.
More about hemoglobin
Hemoglobin (Hb) is an iron-containing protein compound, mostly concentrated in red blood cells (erythrocytes) and partially found free in serum. Thanks to it, the process of transporting oxygen from the lungs to the tissues of the body and in the opposite direction of carbon dioxide occurs.
If we draw an analogy, an erythrocyte can be compared to a cargo longboat plying along the bloodstream, and hemoglobin molecules can be compared to peculiar containers in which oxygen and carbon dioxide are transported.
Reference! Normally, one red blood cell contains about 400 million hemoglobin molecules.
Participation in gas exchange is a very important, but far from the only function of hemoglobin, or “blood balls,” which received their name for their round shape (from the Greek haima - “blood” and the Latin globus - “ball”). Due to its unique chemical properties, this protein plays a leading role among other elements of the blood buffer system, maintaining the acid-base balance of the body at the proper level.
It binds at the cellular level and removes acidic compounds, which prevents acidosis - the process of acidification of blood and tissues. In the lungs, where Hb enters in the form of carboxyhemoglobin (HbCO2) due to the synthesis of carbon dioxide, it prevents the opposite process - alkalosis or alkalization of the blood.
A derivative of the described substance, methemoglobin (HbOH), has another useful characteristic - it is able to firmly bind hydrocyanic acid and other harmful substances. Thus, Hb takes the hit and significantly reduces the degree of intoxication of the body.
Causes of hypoplastic anemia
Hypoplastic anemia is manifested by a decrease in the content of all cells in the blood.
External and internal factors lead to such a pathological and life-threatening condition:
- vibration and radiation effects on the body;
- serious injuries;
- taking certain medications;
- ingestion of poisons into the body;
- herpes, fungi, bacteria;
- genetic mutations;
- rheumatoid arthritis, lack of elements involved in hematopoietic processes;
- endocrine diseases, etc.
What is the norm for glycated hemoglobin?
The definition of this indicator is used exclusively in endocrinology for the diagnosis of diabetes mellitus. According to WHO recommendations, if a person has 6.5% or more of hemoglobin bound to glucose (that is, glycated), he should be diagnosed with diabetes. In addition, periodic monitoring of this indicator in the blood of people with diabetes helps doctors assess how effective their prescribed treatment is and how accurately patients follow the recommendations.
If glycated hemoglobin is 5.7 - 6.4% of the total, doctors diagnose prediabetes. Thus, it is desirable that the amount of hemoglobin bound to glucose does not exceed 5%.
Symptoms of anemia
Conventionally, the symptoms of low hemoglobin are classified into:
- specific (manifest only in specific types of anemia);
- nonspecific (the same for all types of disease).
Nonspecific symptoms of anemia are as follows:
- pallor of the skin/mucous membranes;
- migraine;
- increased fatigue;
- noise in ears;
- refusal of food;
- constant drowsiness;
- feeling of lack of air;
- dizziness;
- cardiopalmus;
- decreased libido, sexual impotence in men;
- disruption of the menstrual cycle;
- heart failure.
Specific signs of different types of anemia:
Each type of anemia has its own specific symptoms. Thus, the acute posthemorrhagic form manifests itself:
- increased heart rate;
- fainting;
- cold sweat;
- attacks of dizziness;
- pale skin;
- decrease in body temperature.
In chronic posthemorrhagic anemia the following are observed:
- very white skin;
- craving for or intolerance to certain smells;
- swelling of the face;
- change in taste sensations;
- dry skin;
- brittle nails;
- nausea;
- lack of air;
- sweating;
- involuntary urination when sneezing or laughing;
- temperature increase.
Hemolytic anemias are characterized by:
- yellowness of the skin and mucous membranes (when red blood cells are destroyed, bilirubin enters the bloodstream);
- increased size of the spleen/liver;
- increased levels of bilirubin in the blood;
- darkening of urine and feces;
- high body temperature;
- weakness.
Sickle cell anemia - a type of hemolytic - has the following symptoms:
- jaundice;
- shortness of breath;
- formation of inflamed areas on the legs;
- blurred vision;
- the presence of hemoglobin in the urine.
Doctors diagnose thalassemia if the patient:
- the shape of the skull bones changes;
- the skin becomes very pale with a yellowish/greenish tint;
- eyes become narrow and swollen;
- there is a lag in mental/physical development;
- bones are deformed;
- the spleen/liver enlarges.
Signs of iron deficiency anemia include:
- buzzing in the head;
- lack of oxygen;
- migraine;
- constant desire to sleep, rest;
- dry skin;
- peeling of nails;
- hair section;
- desire to eat chalk, smell paint, etc.;
- violation of the act of urination;
- hyperhidrosis.
Also, during laboratory tests, it is discovered that the level of hemoglobin and red blood cells in the blood is significantly lower than the established norm.
B12 deficiency anemia affects the gastrointestinal tract and central nervous system.
As a result, the patient experiences:
- swelling of the legs;
- crawling sensation on the arms/legs;
- change in gait;
- memory impairment;
- problems swallowing food;
- enlarged liver/spleen;
- drying of the gastrointestinal mucosa.
In turn, folate deficiency anemia manifests itself:
- inability to eat acidic foods;
- glossitis;
- difficulty chewing and swallowing food;
- enlarged spleen/liver;
- atrophy of the mucous membranes of the gastrointestinal tract.
The symptoms of hypoplastic anemia are:
- the appearance of ulcers in the mouth, on the skin of the face;
- bruising on the skin;
- severe bleeding gums;
- increased fatigue;
- desire to sleep;
- tachycardia;
- decrease in the number of leukocytes, red blood cells and platelets in a blood test.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
What is low hemoglobin in adults, its signs
Stress and poor nutrition lead to a decrease in the number of red blood cells in the patient’s blood, which respond to the movement of air in the body. Hemoglobin appears in red blood cells and ensures the delivery of oxygen to organs.
It takes carbon dioxide from the body and transfers it to the lungs. If the hemoglobin level is low, it means that the body does not receive enough oxygen.
Hemoglobin norm
If the hemoglobin in the human body is below normal, then doctors call it anemia and consider it a dangerous disease.
Normally, hemoglobin should be like this:
| Normal hemoglobin level in adults | ||
| Age | Men | Women |
| 12-15 years | 120-160 | 115-150 |
| 15-18 years old | 117-166 | 117-153 |
| 18-45 years old | 132-173 | 117-155 |
| 45-65 years | 131-172 | 117-160 |
| after 65 years | 126-174 | 117-161 |
Low hemoglobin can become low for various reasons:
- Blood loss occurs during operations, hemorrhoids and serious injuries or gastrointestinal diseases (hidden).
- Lack of amino acids that help synthesize hemoglobin. The reason may be an unbalanced diet.
- Problems in the digestive system prevent iron from being absorbed normally.
- Diseases such as hepatitis and tuberculosis destroy red cells in the blood and, as a result, low hemoglobin.
- Hypothyroidism is formed due to low levels of thyroid hormones, they are responsible for the process of iron absorption, and their lack reduces hemoglobin levels.
- Autoimmune inflammation leads to a decrease in hemoglobin levels.
- Stress depresses the psyche, and such long-term conditions disrupt metabolic processes and affect hemoglobin levels.
- If you often drink tea, chocolate, or strong coffee, the absorption of iron will slow down, which will lead to a decrease in hemoglobin.
- If you move little, blood flows through the veins more slowly and the brain receives information that there are enough red blood cells in the body, so they do not need to be produced. As a result, hemoglobin decreases.
- Low hemoglobin occurs in donors who constantly donate blood, but it returns to normal quickly if everything is fine in the body.
Signs of low hemoglobin are:
- pale skin;
- weakness;
- rapid breathing;
- tachycardia;
- noise in ears;
- headache;
- dizziness.
The manifestation of low hemoglobin is also called sideropenic syndrome.
This includes:
- brittle nails;
- dry hair;
- craving for the smell of gasoline or others;
- desire to eat chalk.
Diagnosis of anemia
To identify anemia in a patient, the doctor conducts a comprehensive diagnosis, which includes:
- clarification of the circumstances under which health deteriorated for the first time, the symptoms that are most pronounced;
- studying the patient's life history. The doctor clarifies whether there are chronic diseases, a hereditary predisposition to any pathological conditions, whether there are bad habits, whether the patient has recently taken any medications, or whether there has been contact with poisons or toxic compounds;
- examination of the skin, determination of its color. Measurement of pressure, pulse;
- laboratory tests of blood and urine.
In some situations, the patient is prescribed a bone marrow test. It is necessary to understand whether there are any disturbances in the hematopoietic processes. Also, using special equipment, a trephine biopsy can be performed, during which the doctor correlates the bone marrow with the tissues surrounding it.
An ECG is usually performed to examine the heart. If necessary, the patient is referred to a hematologist.
Laboratory diagnosis of low hemoglobin
In blood biochemistry, if anemia is suspected, the levels of:
- glucose;
- cholesterol;
- uric acid;
- creatinine;
- electrolytes.
This is necessary in order to assess the condition of the patient’s internal organs. A urine test is also performed to exclude the presence of concomitant diseases.
Laboratory signs of different types of anemia:
- posthemorrhagic acute anemia. Reticulocytes more than 11%, the presence of immature red blood cells and red blood cells of abnormal shapes. Leukocytes - 12 g/l (increased), shift in the formula - to the left;
- chronic posthemorrhagic anemia. Presence of tiny, poorly colored and oval red blood cells. Unexpressed lymphocytosis. Iron - below 9 µmol/l. A decrease in the amount of calcium and copper against the background of an increase in the concentration of manganese, nickel and zinc;
- sickle cell anemia. Hemoglobin is reduced to a level of 50 to 80 g/l, red blood cells - from 1 to 2 T/l. Reticulocytes are increased by about a third. The presence of red blood cells, the shape of which resembles a sickle;
- Thalassemia. Detection of target-like red blood cells in a blood sample, an increase in the number of reticulocytes. Hemoglobin - 20 g/l, erythrocytes - 1 T/l. Decreased concentration of platelets and leukocytes;
- B12 deficiency anemia. The presence of giant erythrocytes. Their color is bright, there is no highlighted area in the center. Shape: pear-shaped or oval. Life expectancy is shortened. Detection of huge neutrophils, a decrease in the number of eosinophils (may be completely absent). The concentration of basophils and leukocytes also decreases. Bilirubin, on the contrary, is increased.
Nutrition for low hemoglobin
Nutrition plays an important role in the fight against low hemoglobin.
In this case, the menu should include iron-containing foods:
- red meat;
- beef liver;
- grenades;
- dried apricots;
- black currant;
- plums, peaches, apples.
Also, the menu for low hemoglobin should include seafood, potatoes, and nuts. A mixture of beets and carrots is effective. In this case, it is necessary that the beet juice steep for 1 hour before mixing with carrot juice. It is worth considering that foods high in calcium prevent iron from being absorbed better.
Do not forget about the reserves of folic acid, which is found in:
- cheese and cottage cheese;
- citrus fruits;
- bananas and kiwi;
- pomegranates and grapes.
Red and black caviar
This product is rich in vitamins that help raise low hemoglobin. It contains Omega-3 fatty acids, which are suppliers of sodium and iron. Caviar contains folic acid in large quantities, which normalizes blood circulation in the tissues. Red caviar is often recommended for pregnant women, because its composition is suitable for fetal development.
Treatment of anemia in children and adults
To get rid of the symptoms of anemia, you need to eliminate the factor that provoked the decrease in hemoglobin. So, if the pathological condition is associated with the presence of parasites in the body, you need to get rid of them, if with poor nutrition, start following a diet, if with a malignant/benign tumor, it should be removed.
In other words, treatment of low hemoglobin in men, women and children may be conservative or require specialized surgical procedures. Usually, in order to improve the condition of patients and reduce the severity of negative symptoms, doctors adhere to the following therapeutic regimen:
- drugs are prescribed that can compensate for the resulting deficiency - B12 for B12-deficiency anemia, iron for iron deficiency, B9 for folate deficiency, etc.;
- normalize the level of red blood cells. This can be accomplished by transfusion of red blood cells or washing of red blood cells. However, these measures when providing assistance to people with low hemoglobin levels are extreme and are carried out only if the resulting disease is life-threatening.
Treatment of acute and chronic posthemorrhagic anemia
Treatment of the acute form of posthemorrhagic anemia is carried out in a hospital. The medications prescribed to the patient help normalize the amount of blood and the level of formed elements, and are also aimed at preventing relapses of the disease. Taking into account the amount of blood lost, the patient may need a transfusion, the introduction of blood substitutes or red blood cells.
As for the chronic form of this type of anemia, it is impossible to get rid of its symptoms without eliminating the cause. After the factor that provoked the pathological condition has been eliminated, the patient will be prescribed a diet that includes eating foods rich in iron. Medicines that can be used are Sorbifer Durules, Ferrum-Lek, vitamins B12 and B9, etc.
Treatment of sickle cell anemia
The main goal of therapeutic measures when it comes to a patient with sickle cell anemia is to prevent the development of hemolytic crises. To do this, the patient must avoid being in places with low oxygen levels. In parallel, blood substitutes and red blood cell infusions can be used.
Elimination of iron deficiency anemia
Treatment of iron deficiency anemia includes eating foods rich in iron and treating existing gastrointestinal diseases. The patient should regularly eat:
- cheeses;
- porridge;
- chicken eggs;
- meat;
- dairy products.
Iron supplements can also help quickly get rid of the symptoms of anemia. The tablets usually used are “Ferrum-Lek”, “Totem”, “Sorbifer Durules”, etc. Injections are prescribed only for severe forms of the disease. It is important that the medicine used does not cause problems with the gastrointestinal tract. If constipation or flatulence occurs, the product needs to be replaced.
Treatment of B12 deficiency anemia
Complex therapy of gastrointestinal diseases and adherence to the principles of proper nutrition help eliminate the manifestations of B12-deficiency anemia. Most often, patients are prescribed vitamin B12 injections. They allow you to quickly restore hematopoietic processes in the bone marrow.
How to get rid of folate deficiency anemia
Folate deficiency anemia is treated by taking vitamin B9 and following a diet. The patient should include foods that contain high amounts of folic acid in their diet. This means citrus fruits, vegetables, herbs, asparagus, nuts, seeds, tomatoes, watermelons, corn, avocados, eggs, animal liver, cod liver, cereals, grain bread.
Treatment of hypoplastic anemia
A hematologist treats hypoplastic anemia. Depending on the age, gender and condition of the patient, he can use different methods - bone marrow transplantation, stimulation of hematopoietic processes, blood transfusion, etc.
Drugs to increase hemoglobin: which ones to take for minor changes
If hemoglobin is at the lower limit of normal, and when examining iron reserves in the body there are no significant deviations (ferritin is not reduced), then taking vitamins with iron or dietary supplements is sufficient. Their advantage is good tolerability, better digestibility, since these additional components stimulate the absorption of the mineral.
Such drugs are never prescribed for the treatment of anemia; they are needed only for preventive purposes:
- for pregnant and lactating women;
- teenagers during active growth;
- at high sports loads;
- after a long illness or exacerbation of chronic inflammation;
- during the recovery period after childbirth, injury, surgery;
- under stress.
Iron-containing vitamins
One of the best iron-containing vitamin complexes is a special Merz dragee. It contains vitamin and provitamin A, group B (B1, B2, B5, B6 and B12), vitamin E, C and nicotinamide. Contains the amino acid cystine and yeast extract. Iron is represented by fumarate; one tablet contains 20 mg. You need to take 2 pieces per day (morning and evening). The price of a package of 60 tablets is 800 rubles.
Fenyuls contains anhydrous iron sulfate in the amount of 150 mg, and vitamins B1, B2, B5, B6, C and nicotinamide help its absorption. Take one capsule per day for a month. For heavy menstruation, it is prescribed 3 days before the expected start of bleeding and stopped 2 days after its end. This helps prevent iron loss. A package of 30 pieces costs 230 rubles.
dietary supplements
Dietary supplements that help normalize Hematogen include Sports Hematogen and Aloe with iron. The first contains bovine blood to raise hemoglobin, more precisely albumin from it, sugar and vitamin complex: group B (B1, B2, B3, B5, B6, B12), A, E, C, H. It has the ability to strengthen the immune system, increase performance and body tone. It has a pleasant taste and is taken one slab per day with meals for a month. Contraindicated for diabetes, obesity, pregnant women and children under 11 years of age. One tile costs 25 rubles.
Aloe syrup with iron contains the mineral in an easily digestible form. This remedy helps normalize hematopoiesis and prevent anemia associated with:
- low acidity of gastric juice;
- intestinal diseases;
- poor nutrition;
- increased stress on the body.
It is prescribed as a teaspoon per day, added to 50 ml of water and taken before meals for 2-4 weeks. A bottle with 100 ml of syrup costs 90 rubles.
Anemia risk group
Low hemoglobin is most often diagnosed in:
- people with gastrointestinal diseases (oncology, gastritis, stomach and duodenal ulcers, inflammatory process in the large/small intestine, etc.);
- persons with poor nutrition, vegetarians;
- people with a genetic predisposition to a certain type of anemia (the disease can be passed from parent to child).
What are the dangers of low hemoglobin?
Anemia can be simultaneously called both a dangerous and harmless disease. So, if we are talking about a mild degree of the disease in a pregnant woman or a small child, then this is more likely a variant of the norm than a deviation. After taking a course of iron supplements, the baby/future mother will become absolutely healthy.
At the same time, moderate and severe degrees of some forms of anemia can lead to such dangerous conditions as:
- anemic coma (the patient loses consciousness and does not respond to any external stimuli, death may occur);
- malfunctions of internal organs (kidneys and liver are especially often affected by anemia);
- decrease in hemoglobin level to less than 70 g/l (death is also possible).
When is it prescribed?
One of the most effective methods of increasing hemoglobin levels is the use of iron-containing drugs, which fully meet the body's needs for iron, and also help normalize hematopoiesis, and are prescribed in the following cases:
- heavy periods in women;
- acute and chronic bleeding;
- irritable bowel syndrome;
- Crohn's disease;
- pregnancy;
- lactation;
- regular blood donation;
- vegetarianism;
- lack of microelements and vitamins in the diet;
- celiac disease;
- malabsorption,
Prevention of anemia
To prevent the development of anemia, it is necessary:
- avoid contact with poisons and toxic substances;
- refuse to visit areas contaminated with radiation;
- do not contact with sources of ionizing radiation;
- do not take medications uncontrollably;
- to harden;
- eat right, include meat, greens, fruits and vegetables in your daily diet;
- spend more time outdoors.
Secondary prevention of low hemoglobin includes:
- blood test once a year;
- seeking qualified medical help in the event of acute infectious and viral diseases;
- annual medical examinations;
- pregnancy planning (for women).
Using traditional methods
An alternative to medications are folk recipes that will help increase hemoglobin.
Herbs are irreplaceable helpers; their correct use will help with anemia. The following infusions and decoctions are made:
- Rosehip infusion with honey. Pour 4 tablespoons of berries into 1 liter of boiling water, leave for about an hour. Add 1 teaspoon of honey to the cooled decoction per 1 cup. One dose per day is enough.
- Rosehip + rowan. This combination is taken 100 grams before meals 3 times a day. It’s done like this: pour 3 tablespoons of berries into a glass of boiling water and leave for 20 minutes.
- A decoction of crushed blackberry leaves, St. John's wort, and clover. Add 1 tablespoon of each plant and pour 200 grams of boiling water, leave for 30-60 minutes. The amount taken per day is 50 ml, the course duration is a month.
In the morning on an empty stomach it is recommended to drink juices from vegetables and fruits.
- Equal proportions of beet, carrot, apple, lemon juice.
- Beet juice + carrot juice.
- Mix equal amounts of 50 ml of apple and cranberry juice, add 100 ml of beet juice.
Take a mixture of nuts and honey. Add 1 liter jar of honey to 2 cups of peeled, crushed kernels. Mix thoroughly and store in a cool place for 30 days. Take before meals 3 times a day.
Treatment
For anemia, treatment should be prescribed by a doctor, based on tests. Anemia can be mild or severe. The first is treated with diet and possible iron supplements. In severe cases, a blood transfusion or special medications are required. Excessive accumulation of iron has a negative effect on the body, so medications should be prescribed by a doctor.
Hemoglobin is an iron-containing protein in the blood, so drugs to increase it are synthetic compounds containing iron. Bivalent it is absorbed in the blood faster. For more active absorption of the substance, medications with ascorbic acid are prescribed.
Drugs for the treatment of anemia exist in the form of tablets, syrups, capsules, drops, and injections.
Taking into account age, gender, and health status, the doctor will prescribe the necessary medicine, indicating the dosage and duration of therapy. They should not be taken together with antibiotics. Side effects may manifest themselves in the form of bloating and diarrhea. If microelements are poorly absorbed, then not only will the intestines malfunction, but allergies may occur, tooth enamel will darken, and the heart rhythm will be disrupted. Therefore, it is important that the course of treatment is monitored by a doctor.