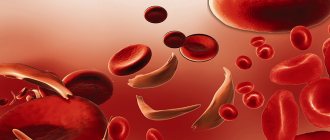
The very concept of anemia reflects pathological changes in the composition of the blood - a decrease in the concentration of the protein component (hemoglobin) and red blood cells (hematocrit), the level of which depends on the volume and number of blood cells - red blood cells. Anemia cannot be called a disease; it is only a symptom of various pathological disorders developing inside the body.
In medical circles, anemia is called fatigue syndrome. This term unites a whole group of hematological syndromes, united by common features - pathological changes in the structure of the blood.
Causes of iron deficiency anemia (IDA)
- insufficient intake of iron from food: fasting, vegetarianism, or a diet depleted in iron and protein, followed for a long time. In breastfed children, the cause may be iron deficiency anemia of the mother, early transfer to artificial feeding, late introduction of complementary foods
- impaired iron absorption: enteritis (inflammation of the mucous membrane of the small intestine caused by infection or helminthic infestation), gastritis and peptic ulcer of the stomach and duodenum; hereditary diseases (cystic fibrosis and celiac disease); autoimmune damage to the intestinal mucosa and possibly the stomach (Crohn's disease); condition after removal of the stomach and/or duodenum; stomach and intestinal cancer
- chronic blood loss. This is the most basic reason. This includes losses due to: gastric and duodenal ulcers, nonspecific ulcerative colitis, Crohn's disease, hemorrhoids and anal fissures, intestinal polyposis, bleeding from disintegrating tumors of any location and varicose veins of the esophagus; hemorrhagic vasculitis; pulmonary hemorrhages, pulmonary hemosiderosis; chronic pyelonephritis, polycystic disease and cancer of the kidneys and bladder; losses during hemodialysis; uterine fibroids, endometriosis, hyperpolymenorrhea, cervical cancer; nosebleeds
- congenital deficiency of iron in the body (prematurity, birth from multiple pregnancy, severe iron deficiency anemia in the mother, pathological bleeding during pregnancy and childbirth, fetoplacental insufficiency)
- alcoholism (the mucous membrane of the stomach and intestines is damaged, making it difficult to absorb iron)
- use of medications: non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen, aspirin) reduce blood viscosity and can promote bleeding, in addition, these drugs can provoke the occurrence of stomach and duodenal ulcers; antacids (Almagel, Gastal, Rennie) reduce the production of hydrochloric acid, which is necessary for effective absorption of iron; iron-binding drugs (desferal), these drugs bind and remove free iron and iron in ferritin and transferrin, and in case of overdose can lead to iron deficiency states
- donation (with donations more than 4 times a year, iron deficiency develops)
- disruption of transferrin synthesis. Transferrin is an iron transport protein that is synthesized in the liver.
Normal hemoglobin level in the blood: in women – 120-140 g/l, in men – 130-160 g/l
Iron in the human body
Iron deficiency anemia (IDA) is the most common form of all currently known anemias, which is due to a large number of reasons and circumstances that can lead to iron deficiency, which will lead to various disorders that are unsafe for the body.
Iron (ferrum, Fe) is a very important element for ensuring the normal functioning of the human body.
Men (of average height and weight) contain approximately 4 – 4.5 grams:
- 2.5 – 3.0 g is in heme Hb;
- in tissues and parenchymal organs, from 1.0 to 1.5 g (approx. 30%) is deposited as a reserve - ferritin;
- myoglobin and respiratory enzymes take up 0.3 - 0.5 g;
- some proportion is present in ferrum transport proteins (transferrin).
Daily losses in males, of course, also occur: every day about 1.0-1.2 g of iron leaves the intestines.
In women, the picture is somewhat different (and not only due to height and weight): their iron content is in the range of 2.6 - 3.2 g, only 0.3 g is deposited, and losses are not only daily through the intestines. Losing 2 ml of blood during menstruation, the female body loses 1 g of this important element, so it is clear why a condition such as iron deficiency anemia occurs more often in females.
In children, the levels of hemoglobin and the iron it contains change with age, however, in general, up to one year of age they are noticeably lower, and in children and adolescents under 14 years of age they approach the female norm.
The most common form of anemia is IDA due to the fact that our body is generally incapable of synthesizing this chemical element and, except from animal products, we have nowhere else to get it. It is absorbed in the duodenum and slightly along the small intestine. Ferrum does not interact with the colon in any way and does not react to it, therefore, once there, it passes through in transit and is excreted from the body. By the way, you don’t have to worry that by consuming a lot of iron with food, we can “overeat” it - humans have special mechanisms that will promptly stop the absorption of excess iron.
metabolism of iron in the body (scheme: myshared, Efremova S.A.)
Clinical manifestations of IDA
Anemic syndrome - occurs due to a decrease in the level of red blood cells and hemoglobin in the blood, reducing the saturation of cells and tissues with oxygen. The signs of anemic syndrome are difficult to recognize, but they help to suspect the presence of anemia and, in combination with the data of other examinations, make a diagnosis. These are general weakness, high fatigue and decreased performance, dizziness, tinnitus and flashing “spots” before the eyes, periodic palpitations, shortness of breath with little physical exertion, and fainting. Upon examination, pallor of the skin and visible mucous membranes, slight swelling of the legs, feet, face (mainly the area around the eyes), tachycardia, various types of arrhythmia, moderate heart murmurs, and muffled heart sounds are revealed.
Sideropenic syndrome - caused by iron deficiency in tissues, which causes a decrease in the activity of many enzymes (protein substances that regulate many vital functions), manifested by numerous symptoms:
- change in taste (desire to eat unusual foods: sand, chalk, clay, tooth powder, ice, as well as raw minced meat, unbaked dough, dry cereals)
- tendency to eat hot, salty, spicy foods
- distortion of the sense of smell (attracted by the smell of gasoline, acetone, the smell of varnishes, paints, lime)
- decreased muscle strength and atrophy
- dry, flaky skin; fragility and hair loss; dullness, transverse striations, spoon-shaped concavity of nails; Minor injuries and abrasions do not heal for a long time
- dryness and cracks in the corners of the mouth in 10-15% of patients
- feeling of tongue fullness, redness and atrophy, frequent periodontal disease and caries
- dryness of the esophageal mucosa, which causes pain when swallowing and difficulty swallowing solid food, the development of atrophic gastritis and enteritis
- urgency to urinate, inability to hold urine when coughing, laughing, sneezing, episodes of bedwetting
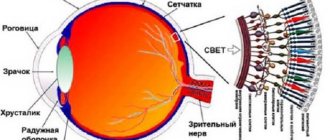
- the symptom of “blue sclera” is characterized by a bluish coloration of the sclera
- prolonged increase in body temperature to subfebrile levels (37.0-37.9°C) for no apparent reason
- frequent ARVI
At first, the body can still cope
When developing iron deficiency states, the speed of development of the process, the stage of the disease and the degree of compensation are of great importance, because IDA has different causes and can arise from another disease (for example, repeated bleeding due to a stomach or duodenal ulcer, gynecological pathology or chronic infections). Stages of the pathological process:
- Hidden (latent) deficiency does not immediately turn into IDA. But in a blood test it is already possible to detect a deficiency of the element if serum iron is examined, although hemoglobin will still be within normal values.
- Tissue sideropenic syndrome is characterized by clinical manifestations: gastrointestinal disorders, trophic changes in the skin and derivatives (hair, nails, sebaceous and sweat glands);
- When your own reserves of the element IDA are depleted, you can determine it by the level of hemoglobin - it begins to fall.
stages of development of IDA
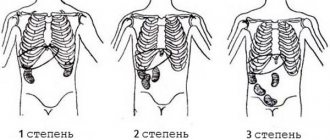
Depending on the depth of iron deficiency, there are 3 degrees of severity of IDA:
- Light – hemoglobin values are in the range of 110 – 90 g/l;
- Medium – Hb content ranges from 90 to 70 g/l;
- Severe – hemoglobin level drops below 70 g/l.
A person begins to feel unwell already at the stage of latent deficiency, but the symptoms will become clearly noticeable only with sideropenic syndrome. It will take another 8-10 years before the clinical picture of iron deficiency anemia appears in full, and only then will a person who has little interest in his health learn that he has anemia, that is, when hemoglobin has noticeably decreased.
Diagnosis of IDA
- clinical blood test: decreased level of hemoglobin, red blood cells, decreased hemoglobin content in one red blood cell, often increased ESR
- biochemical blood test: decrease in serum iron level, increase in total iron-binding capacity of serum, decrease in ferritin content in blood serum
If an iron deficiency is detected in the patient’s body using tests, then the next step will be to search for the causes of this deficiency. To identify the cause of iron deficiency, a comprehensive examination is carried out, including esophagogastroduodenoscopy, sigmoidoscopy, colonoscopy, bronchoscopy, chest x-ray, ultrasound examination of the abdominal organs, pelvis and kidneys, examination by a gynecologist, urologist, hematologist, stool analysis for occult blood and eggs. helminths, as well as examination of red bone marrow from the sternum or ilium (sternal puncture, trephine biopsy).
How does iron deficiency manifest?
The clinical picture usually does not manifest itself at the first stage; the latent (hidden) period of the disease produces minor changes (mainly due to oxygen starvation of tissues), which have not yet identified clear symptoms. Circulatory-hypoxic syndrome: weakness, tachycardia during physical exertion, sometimes ringing in the ears, cardialgia - many people present similar complaints. But few people would think of taking a biochemical blood test, which will include serum iron among other indicators. And yet, at this stage, the development of IDA can be suspected if stomach problems appear:
- The desire to eat food disappears, the person does it more out of habit;
- Taste and appetite become perverted: instead of normal food, you want to try tooth powder, clay, chalk, flour;
- There are difficulties with swallowing food and some vague and incomprehensible sensations of discomfort in the epigastrium.
- Body temperature may rise to subfebrile levels.
Due to the fact that in the initial stage of the disease symptoms may be absent or mild, in most cases people do not pay attention to them until sideropenic syndrome develops. Is it possible that during some medical examination a decrease in hemoglobin will be discovered and the doctor will begin to find out the medical history?
Signs of sideropenic syndrome already give reason to assume an iron deficiency state, since the clinical picture begins to acquire the coloring characteristic of IDA. The skin and its derivatives suffer first; a little later, due to constant hypoxia, internal organs are involved in the pathological process:
- The skin is dry and flaky on the arms and legs;
- Peeling nails are flat and dull;
- Seizures in the corners of the mouth, cracks on the lips;
- Drooling at night;
- Hair splits, grows poorly, loses its natural shine;
- The tongue hurts, wrinkles appear on it;
- The slightest scratches heal with difficulty;
- Low body resistance to infectious and other unfavorable factors;
- Muscle weakness;
- Weakness of physiological sphincters (urinary incontinence when laughing, coughing, straining);
- Socket atrophy along the esophagus and stomach (esophagoscopy, fibrogastroduodenoscopy - FGDS);
- An imperative (sudden urge that is difficult to control) urge to urinate;
- Bad mood;
- Intolerance to stuffy rooms;
- Drowsiness, lethargy, swelling of the face.
This course can last up to 10 years; treatment of iron deficiency anemia from time to time can slightly increase hemoglobin, which makes the patient calm down for a while. Meanwhile, the deficiency continues to deepen if the root cause is not addressed and gives a more pronounced clinical picture: all of the above symptoms + severe shortness of breath, muscle weakness, constant tachycardia, decreased ability to work.
Complications of IDA
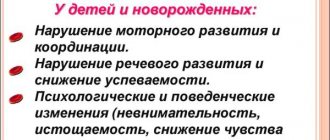
Complications arise with prolonged anemia without treatment and reduce the patient’s quality of life: decreased immunity, increased heart rate, which leads to heart failure; in pregnant women, the risk of premature birth and fetal growth retardation increases; in children, iron deficiency causes retarded growth and development; a rare and severe complication is hypoxic coma; hypoxia due to iron deficiency complicates the course of existing cardiopulmonary diseases (coronary artery disease, bronchial asthma, chronic cerebral ischemia, etc.) until the development of emergency conditions, such as acute or repeated myocardial infarction and acute cerebrovascular accident (stroke).
Anemic syndrome
This syndrome is manifested by nonspecific signs characteristic of all anemias:
- shortness of breath that appears with minimal physical activity;
- interruptions in heart function;
- dizziness when changing body position;
- tinnitus.
The severity of the above symptoms depends on the rate of decrease in hemoglobin. Iron deficiency anemia has a chronic course, so patients are able to adapt to its manifestations.
In some cases, the first complaints with iron deficiency anemia may be:
- fainting conditions;
- angina attacks;
- decompensation of vascular lesions of the brain.
Treatment of IDA
The basic principles of treatment for iron deficiency anemia include eliminating the cause of iron deficiency, correcting the diet, and replenishing iron deficiency in the body.
- The diet for iron deficiency anemia consists of eating foods rich in iron. Patients are advised to have a nutritious diet with the obligatory inclusion in the diet of foods containing heme iron (veal, beef, lamb, rabbit meat, liver, tongue). Plant foods rich in iron include beans, beans, lentils, peas, spinach, cauliflower, potatoes, carrots, beets, bananas, apricots, peaches, apples, blueberries, raspberries, strawberries, almonds and walnuts. It should be remembered that ascorbic acid, which is found in bell peppers, cabbage, rose hips, currants, citrus fruits, sorrel, enhances the absorption of iron in the gastrointestinal tract, and oxalates and polyphenols (coffee, tea, soy protein, milk, chocolate) worsen the absorption of iron. calcium, dietary fiber and other substances. However, no matter how much meat we eat, only 2.5 mg of iron will enter the bloodstream per day - this is exactly how much the body can absorb. And 15-20 times more is absorbed from iron-containing complexes - that’s why the problem of anemia cannot always be solved with the help of diet alone, and therefore iron-containing drugs are prescribed
- Oral iron supplements differ from other medications by special rules of administration: - short-acting iron-containing preparations are not taken immediately before or during meals. The medicine is taken 15-20 minutes after meals or in the pause between doses; prolonged medications (sorbifer durules, tardiferron-retard, etc.) can be taken before meals and at night (1-2 times a day); - iron supplements are not taken with milk and milk-based drinks (kefir, fermented baked milk, yogurt) - they contain calcium, which will inhibit the absorption of iron - tablets (except for chewable ones), dragees and capsules are not chewed, are swallowed whole and washed down with plenty of water, rosehip decoction or clarified juice without pulp Oral iron supplements (in tablets, drops, syrup, solution) are the initial treatment for mild to moderate anemia; if there is pregnancy, the intake is agreed with an obstetrician-gynecologist. The duration of treatment is 4–8 weeks until hemoglobin levels normalize, then the drug is taken for 4–6 weeks at half the dose. The most commonly prescribed: - sorbifer durules/fenuls 100 mg, 1-2 tablets 1-2 times a day until hemoglobin levels are restored (in pregnant women, for prevention, 1 tablet 1 time a day, for treatment, 1 tablet 2 times a day) - ferretab comp . 1 capsule per day, up to a maximum of 2-3 capsules per day in 2 divided doses, minimum period of use is 4 weeks - maltofer/actiferrin comes in three dosage forms (drops, syrup, tablets), intake 40-120 drops/10-30 ml syrup / 1-3 tablets per day in 1-2 doses - tardiferron 80 mg, 1-2 tablets per day, pregnant women 1 tablet per day, II-III trimester - totema (combined preparation of iron, copper and manganese) 2- 4 ampoules per day, solution diluted in 1 glass of water, taken for 3-6 months - ferlatum 15 ml 1-2 bottles per day in 2 divided doses
- Injectable iron preparations (venofer, likfer, cosmofer, ferrinject) are used exclusively in the hospital (it is necessary to have the ability to provide anti-shock care), contraindicated during pregnancy and lactation
- Hemotransfusion (transfusion of red blood cell-containing blood components) is performed in case of severe anemia, according to strict indications and in a hospital setting.
Side effects
The most common side effects observed during treatment with iron supplements are a metallic taste in the mouth, darkening of tooth enamel, allergic skin rashes, digestive disorders as a result of irritation to the mucous membrane of the digestive tract, especially the intestines (loose stools, nausea, vomiting). Therefore, the initial doses of drugs should be 1/3–1/2 of the therapeutic dose, followed by increasing them to the full dose over several days in order to avoid the occurrence of severe side effects.
Intramuscular administration of iron supplements is carried out only under strict indications due to the development of pronounced local and systemic side effects. Indications for intramuscular administration of iron preparations are as follows: diseases of the digestive tract (poor intestinal absorption syndrome, ulcerative colitis, chronic enterocolitis, gastrointestinal bleeding) and intolerance to iron-containing preparations when taken orally.
Contraindications to the prescription of iron supplements are anemia not caused by iron deficiency (hemolytic, aplastic), hemosiderosis, hemochromatosis.
Forecast and prevention of iron deficiency anemia
In most cases, iron deficiency anemia can be successfully corrected. However, if the cause is not addressed, iron deficiency may recur or progress. Iron deficiency anemia in infants and young children can cause delayed psychomotor and intellectual development.
In order to prevent iron deficiency anemia, annual monitoring of clinical blood test parameters, nutritious nutrition with sufficient iron content, and timely elimination of sources of blood loss in the body are necessary. Persons at risk may be advised to take prophylactic iron supplements.
Hyposiderosis
Symptoms of hyposiderosis are associated with a lack of iron in tissues. This is accompanied by:
- deterioration of the hair structure with splitting of the ends;
- signs of asthenia;
- excessive dry skin, which can be minimally corrected with moisturizing cosmetics;
- pathological changes in the nails, transverse striations of the nail plate, changes in its shape;
- violation of the body’s protective properties with frequent viral diseases;
- the appearance of angular stomatitis, manifested by cracks with areas of inflammation in the corners of the mouth;
- signs of inflammatory lesions of the tongue;
- change in skin color to a pale greenish tint;
- unusual eating habits (desire to eat chalk, ashes and other substances);
- addiction to unusual smells;
- blue sclera due to dystrophic changes in the cornea of the eye against the background of iron deficiency.
According to recent studies conducted by pediatricians and hematologists, children with tissue iron deficiency experience mental retardation. This is due to a disruption in the processes of myelination of nerve fibers with a decrease in the electrical activity of the brain. Also, in young patients there is a high risk of developing heart failure, however, clear mechanisms of myocardial damage due to hyposiderosis have not been identified. [adsen]
Diet
The International Association of Hematologists states that by normalizing the eating behavior of a patient with signs of mild iron deficiency anemia, it is possible to significantly normalize blood counts and not resort to the use of iron supplements to eliminate the iron deficiency state. For patients with severe anemia, the use of a specialized diet is indicated as an addition to the main treatment.
The fundamental principles of therapeutic nutrition for iron deficiency anemia are a sharp limitation in the consumption of fats of both plant and animal origin, as well as enrichment with foods containing large amounts of protein. It has been proven that carbohydrates do not affect the body's absorption of iron in any way, so their consumption should not be limited.
In order to replenish the level of iron necessary for normal hematopoiesis, it is necessary to include in the patient’s diet a large amount of foods containing iron (liver, beef tongue, lean turkey meat, red types of sea fish, buckwheat and millet cereals, blueberries and peaches). A large percentage of iron is also found in all types of greens, beef and eggs. Among fruits, preference should be given to persimmons, quinces and apples, raw or baked.
It is recommended that patients with iron deficiency anemia completely exclude dairy products and black tea from their diet, as they contain substances that interfere with the absorption of iron. And, on the contrary, synergistic products that should be consumed in large quantities together with iron-containing products are those that contain a high percentage of vitamin C (sorrel, currants, sauerkraut, freshly squeezed fruit and citrus juices with pulp).