It is now well known that the greatest impact of Covid falls on the lungs. Fears of getting fibrosis as a result of covid pneumonia are justified, but not everyone is at risk.
What is pulmonary fibrosis? This is a long-term consequence of an inflammatory pulmonary process. Including against the background of coronavirus infection. As a result of inflammation, the lung tissue is replaced by a connective tissue scar, which excludes segments or lobes of the lung from gas exchange, reducing the functional and adaptive capabilities of the respiratory system.
General information
Fibrous changes in the lungs, what is it?
This is a pathological process of the formation of fibrous tissue (connective tissue) that replaces lung tissue, which leads to disruption of the elasticity of the lung and the function of gas exchange. With the formation of fibrous changes (synonymous with “pneumofibrosis”), elasticity is irreversibly lost. Fibrous changes in the lungs are the outcome of many diseases of the bronchopulmonary system, and also occur in other diseases. As pneumofibrosis progresses, a gradual restructuring of the lung tissue occurs - the structure of the acinus , sclerosis of the walls of the bronchioles develops, the capillary network becomes empty, and abnormal glandular structures are formed. These changes destroy and deform the lung tissue, and cyst-like expansions and fibrous fields are formed in this place. Areas of fibrosis can occur around the lymphatic vessels, in the interlobular septa, along the outflow of lymph from foci of former inflammation, in the tissue around the bronchi and blood vessels.
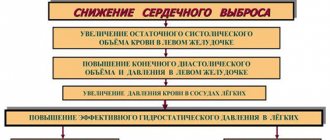
The further course of the disease and prognosis depend on the type of pulmonary fibrosis and the degree of its spread, since it determines the degree of impairment of respiratory function and gas exchange, as well as the severity of clinical manifestations. There are relatively favorable types of fibrotic changes and unfavorable ones. pulmonary hypertension quickly develop , which ultimately leads to a deterioration in the patient’s quality of life and a shortening of its duration.
Therapy of local (limited) pneumofibrosis
Scarring is limited to a small area. Often a person does not have any health problems; he learns about fibrosis only after taking an x-ray. If there are no clinical manifestations, such a person does not need medical intervention. But it would be useful to find the cause and take preventive measures: quit smoking, change jobs if it involves inhaling hazardous substances, enrich your diet with fats and proteins, avoid hypothermia and treat colds in a timely manner.
Doctor: Olga Shishkina ✓ Article checked by doctor
Pathogenesis
The final sections of the respiratory tract consist of bronchioles (terminal and respiratory), acini and lobules. Terminal bronchioles are air-conducting, and respiratory bronchioles are involved in gas exchange, since they are connected to the alveoli through pores. The acini is the structure of the lung where gas exchange occurs and includes several respiratory bronchioles. The acini (from 3 to 24) are united into pulmonary lobules. The framework of the lobule includes interlobular septa, periarterial, peribronchial connective tissue, connective tissue of the alveolar and acini septa.
Connective tissue consists of collagen, reticular and elastin fibers. Interweavings of collagen and elastin fibers are present around the bronchi and in the alveolar walls, which determines the elastic properties of the lungs. Collagen provides rigidity to the intrapulmonary framework.
Connective tissue cells (smooth muscle and fibroblasts) synthesize elastin and collagen. Its primary role is to maintain the tone of the terminal sections of the respiratory tract. At the same time, connective tissue cells also synthesize enzymes (proteases) responsible for the destruction of elastin and collagen . The enzyme and antienzyme systems are in equilibrium under normal conditions. Under conditions of infectious inflammation, they continue to have an elastolytic (destructive) effect due to the high production of elastase (an enzyme that destroys elastic fibers, elastin, collagen). This causes the destruction of the normal connective tissue matrix, the destruction of the alveolar walls and the formation of common cavities. Excessive production of elastase or the absence of enzymes for its destruction is observed in a number of lung diseases ( COPD , emphysema , cystic fibrosis ).
In parallel, during inflammatory processes, there is an activation of fibroblasts that produce collagen. As a result, there is an enhanced process of development of connective tissue in the lung parenchyma and the formation of fibrosis. The development of fibrotic changes is preceded by edema and infiltration of the lung tissue. When the alveolar membrane is destroyed, intra-alveolar fibrosis develops at this site - growths of connective tissue spread into the alveoli. Then the connective tissue around the arteries and bronchi is involved in the pathological process.
Currently, a more acceptable theory of the pathogenesis of silicosis and other pneumoconioses is the immunological one, which states that the development of these occupational diseases is impossible without phagocytosis of dust particles by alveolar macrophages. The rate of their death depends on the fibrogenic aggressiveness of the dust and is proportional to it. The death of alveolar macrophages is a mandatory step in the formation of a silicotic nodule. The formation of a nodule is possible under the condition of repeated phagocytosis of dust. The resulting pro-inflammatory mediators ( cytokines ) provoke the accumulation of inflammatory cells in the septa of the alveoli, and oxygen radicals, damaging lung tissue, cause the death of macrophages.
Proteolytic enzymes (metalloproteinase and elastase) are released from destroyed macrophages and destroy lung tissue. The inflammatory phase is accompanied by recovery processes in which growth factors stimulate the formation of cells, epithelium and new vessels in damaged tissues. Uncontrolled epithelization processes lead to the development of fibrosis. Growth factors play one of the key roles in fibrogenesis . Their stimulating effect on the proliferation of fibroblasts and the destruction of collagen and fibronectin (high molecular weight protein of connective tissue) has been proven. In idiopathic fibrosis, fibrosis predominates with mild inflammatory changes. The main mechanism for the progression of pneumofibrosis is constant damage to the alveolar epithelium with impaired regeneration and excessive deposition of connective tissue due to the activation of fibroblasts.
Basics of therapy for apical pulmonary fibrosis
Changes are found at the apex of the lung. This may be a trace of pneumonia once suffered or a proliferation of connective tissue provoked by exposure to harmful substances, also found in ankylosing spondylitis and other autoimmune diseases.
More often than not, it is enough to remove the cause to stop sclerosis. But this is a disease that needs to be observed over time. If the lesion increases, anti-inflammatory drugs (NSAIDs, steroid hormones), cytostatics and antifibrotic drugs are used.
Classification
According to prevalence and X-ray or CT signs:
- Local pulmonary fibrosis (limited). Local pulmonary fibrosis affects only part of the lung tissue, which becomes denser. The pictures clearly define the boundaries of the pathological process. Limited pulmonary fibrosis does not affect the elasticity of the entire lung and has almost no effect on respiratory function. It is asymptomatic and often does not bother patients. An example of limited fibrosis would be the outcome of macrofocal pneumonia. In chronic bronchiolitis, X-ray examination reveals, in addition to local pneumosclerosis , thickenings around the bronchi. With this disease, bilateral fibrotic changes in the lower sections are usually found.
- Diffuse. With this option, fibrosis diffusely covers the entire lung tissue and the spread of the process occurs much faster than with the local form. The lung tissue becomes denser, the structure is deformed and the volume of the lungs decreases. In this regard, respiratory function deteriorates significantly.
- Focal pulmonary fibrosis is the presence of several foci of different sizes and structures. They can be either limited (rounded) or diffuse (blurred, without clear boundaries). Focal pneumofibrosis is detected in silicosis, pneumoconiosis, at the location of granulomas of various origins.
- Linear pulmonary fibrosis. In what pathology does it occur and what does “linear pulmonary fibrosis” mean? This term is used to describe an X-ray examination or CT scan of the lungs if a tissue compaction is detected in the form of a cord of a linear shape (practically it is a scar that has a linear shape). This type of fibrosis forms after inflammatory diseases (primarily tuberculosis ), injuries, and surgical interventions. Linear pathology often appears on x-ray only several years after the illness. An area of linear fibrosis, which is associated with the root of the lungs, indicates a history of hilar pneumonia or a primary tuberculosis complex. In the chronic form of exogenous alveolitis, CT manifestations are: cellular and rough linear fibrosis. In idiopathic fibrosis, parenchymal damage is symmetrical, and depending on the stage, linear fibrosis, ground glass, bronchiectasis and honeycomb lung are very often observed.
- Peribronchovascular fibrosis is the presence of connective tissue along the bronchovascular bundle. At the same time, the lumen of the bronchi and blood vessels narrows, which causes ventilation and vascular disorders.
- Acinar (intralobular) - the process reflects the filling of acini and terminal bronchioles with connective tissue cells. With this form, pronounced perfusion-diffusion disorders are noted. This is how interstitial pneumonia appears on CT.
- “Honeycomb lung” is a complete loss of the normal structure of the lung. In the lung tissue there is an alternation of fields of fibrosis, emphysema and cysts, which resembles a honeycomb.
With the flow:
- Progressive.
- Not progressive.
Idiopathic pulmonary fibrosis is a special form/variant of chronic fibrosing interstitial pneumonia of unknown etiology, which steadily progresses and is a cause of mortality. It occurs predominantly in older people and affects only the lungs. The process is more often localized in the peripheral parts of the lungs and is manifested by interstitial inflammation of the alveoli with the formation of fibrosis around the alveolar ducts.
As mentioned above, the causes of the disease are unknown, but there are factors that aggravate idiopathic pulmonary fibrosis - smoking, inhalation of inorganic and organic dust, viral infection, diabetes mellitus .
The disease most often occurs in patients over 50 years of age. The incidence of the disease increases with age and predominates after 60–70 years.
How to treat the disease
Before prescribing therapy, an examination is carried out to establish a diagnosis.
The main diagnostic method is radiography. Additionally, bronchoscopy, assessment of respiratory function, and general laboratory tests are performed. This body of research also reveals the underlying cause of pulmonary fibrosis. There is no effective therapy against pulmonary fibrosis yet.
Pneumofibrosis without symptoms is not always treated with medications.
If the disease has not entered the acute phase, treatment is carried out at home. The main task of therapeutic measures is to eliminate the cause of the disease. When the cause is the ingress of dust particles or other harmful substances, then, first of all, stop contact with the provocateur of the disease. Excitement and stress are contraindicated for the patient.
If the cause is an infection, antibacterial drugs are indicated depending on the pathogen. Maintenance therapy is also prescribed.
Breathing exercises are useful and help improve the functionality of the breathing apparatus.
In advanced forms, surgical treatment is possible. After a course of therapy, the patient is registered with a pulmonologist for a year or more.
Treatment with folk remedies
Often, with pneumofibrosis, they resort to traditional medicine. In mild forms, this type of treatment becomes the main one. They use herbal decoctions and teas, compresses for rapid removal of phlegm, lotions and warming.
Pine buds have long been used for lung diseases. This valuable product contains many essential oils that have a beneficial effect on the respiratory tract - they help eliminate mucus, destroy pathogenic microbes, and activate the secretory ability of the epithelium.
For the decoction, take 10 g of kidneys, add a glass of water, and heat in a water bath for half an hour, leave for another 15 minutes. Then the broth is filtered and drunk warm 3 times daily at a dose of 1 tablespoon.
Causes
Pneumofibrosis is caused by various lung diseases:
- Infectious diseases, among which should be noted pneumonia of various origins (including mycotic), tuberculosis , syphilis , cytomegalovirus infection . The prolonged course of pneumonia is often complicated by lung abscess and pleural , which resolve with the formation of fibrosis. Risk factors for prolonged pneumonia are inflammation in several lobes and secondary bacteremia. Staphylococcal pneumonia is characterized by the formation of destructive changes in the lungs, slow recovery and resolution of the process with a frequent outcome in local pneumofibrosis. Pneumonia caused by Legionella pneumophila (Legionnaires' disease) is characterized by the same slow reverse development of infiltrates and a high incidence of pneumofibrosis. Pneumonia caused by Chlamydophila pneumoniae has residual changes in the form of pneumofibrosis in 10-20%, and Pneumocystis pneumonia occurs with the development of diffuse fibrosis .
- Chronic obstructive pulmonary disease , including bronchial asthma . With it, the inflammatory process causes a change in the structure of the bronchial wall with the development of fibrosis.
- Occupational dust diseases. They are caused by inhalation of aggressive dust and gases. The term “pneumoconiosis” combines various types of dust fibrosis. This is diffuse pneumonitis with the development of pulmonary fibrosis. In this regard, occupational diseases are divided into silicosis (develops from inhalation of silica dust), silicosis (cement, asbestosis , talcosis , kaolinosis ) and metalloconiosis ( aluminosis , siderosis , berylliosis , baritosis ). In the initial stages of the disease, the disease occurs with a picture of chronic bronchiolitis, progressive alveolitis, which turns into pneumofibrosis.
- Sarcoidosis . The pulmonary form of sarcoidosis (there is no enlargement of the intrathoracic lymph nodes) proceeds for a long time with minimal symptoms, and when the patient develops widespread fibrosis with gross disturbances in the structure of the lungs, with the formation of bronchial stenosis and traction bronchiectasis, severe respiratory failure develops (shortness of breath at rest, diffuse cyanosis ). The symptom of drumsticks is revealed. In the lungs, against the background of pneumofibrosis and emphysema, lesions are observed throughout.
- Ideopathic pulmonary hemosiderosis is a disease of unknown origin in which intra-alveolar hemorrhages with hemolysis periodically occur. Frequent repeated exacerbations cause the development of diffuse fibrosis.
- Allergic lung diseases (hypersensitivity pneumonitis or exogenous allergic alveolitis). Exogenous allergic alveolitis is an immunopathological disease that occurs when inhaling organic dust containing antigens. The disease manifests itself as widespread damage to the alveoli and interstitial tissue with the development of pneumofibrosis. Cases of this disease occur in workers who come into contact with resins, dyes, plastics and polyurethane. There are known cases of the development of alveolitis when exposed to fungicides (copper sulfate for spraying plants) and salts of heavy metals (beryllium, chromium, cobalt, arsenic). With this group of diseases, there is always an indication of contact with the allergen. The disease occurs with cough and shortness of breath. On auscultation there are widespread fine bubbling and crepitating rales. Severe ventilation disturbances are noted.
- Idiopathic fibrosing alveolitis . This disease is of unknown etiology and is characterized by diffuse progressive fibrosis, which is clinically manifested by progressive shortness of breath, respiratory and heart failure, and the formation of cor pulmonale. In the lungs, diffuse thickening of the interalveolar septa is noted, the structure of the pulmonary structures is disrupted and cystic cavities are formed. In acute or subacute cases, when alveolitis constantly recurs, the patient's condition quickly deteriorates as inspiratory dyspnea persistently increases, although treatment with glucocorticoids is carried out. In a chronic course, diffuse pneumosclerosis .
- A condition after surgical interventions on the lungs, which often occurs with excessive formation of pneumofibrosis.
- Diseases of other organs and systems that cause fibrosis.
- Chronic active hepatitis .
- Diabetes mellitus , which increases the risk of pneumonia by 2.5 times, asthma by 2 times, and pulmonary fibrosis by 1.5 times.
- Systemic autoimmune diseases: scleroderma , rheumatoid arthritis , systemic lupus erythematosus , ankylosing spondylitis . apical fibrosis , bronchiectasis develop . Apical (in the upper lobe) fibrosis in this disease is a specific symptom and occurs in 3-4%. It is usually asymptomatic, but can cause coughing, sputum, and shortness of breath. Systemic scleroderma is generally characterized by fibrotic changes in organs and tissues due to increased fibroblast function. In 70% of cases, scleroderma occurs with lung damage, which occurs in two variants: interstitial pulmonary fibrosis and pulmonary hypertension (primary or secondary). Pulmonary fibrosis develops in the early stages and is often limited to the basal regions (lower lobe). In some patients, it is diffuse in nature and quickly leads to a decrease in lung volume and severe respiratory failure. Pulmonary fibrosis and pulmonary hypertension are clinically manifested by shortness of breath that worsens over time and a persistent dry cough.
- Chronic form of cytomegalovirus infection .
Massage for illness
Therapeutic massage is prescribed as additional procedures to the main method of treatment. It is especially effective for local types of disease, but in all cases massage improves the respiratory functions of the lungs, strengthens the muscles in the chest area and improves blood circulation.
Contraindications to it are cardiovascular disorders, purulent processes in the organ and late stages of fibrosis. A massage therapist can use different techniques, perform the procedure using hands or instruments.
The most common options are:
- Honey massage. Warms the skin and increases blood flow to the chest. Not carried out if you are allergic to honey or have hypersensitive skin.
- Vacuum massage. The massage therapist uses special cups, the vacuum effect helps to increase blood circulation.
- Vibration massage. It is carried out with devices that strengthen muscles and eliminate hypertension.
- Massage with badger fat. It has a local antimicrobial effect and accelerates the removal of sputum.
Hand massage techniques include stroking and rubbing. The main area is the chest area, as well as the back and neck. Massage must be carried out in courses.
Common reasons
- Inhalation of toxic substances.
- Exposure to radiation therapy , the consequence of which is post-radiation pulmonary fibrosis. Most often, post-radiation fibrosis develops after irradiation of the mediastinal area for lymphogranulomatosis and breast cancer . During radiation therapy, the development of pleural fibrosis is also possible. In the acute period after irradiation, pulmonary failure often develops, and in the later stages, radiation pneumonitis , intra-alveolar and interstitial fibrosis . Such complications are explained by the fact that the focus of irradiation falls on the area of the lungs, which are very sensitive to ionizing radiation and are quickly damaged. For radiation treatment of breast cancer, the dose is 70-80 Gy, and the maximum radiation tolerance of the lungs is 35-40 Gy. The incidence of complications depends on the total focal dose. In this case, the age of the patient and the location of the lesion are important. People over 70 years old have complications from radiotherapy 1.5 times more often than people aged 40-60 years. The closer to the mediastinum the focus is, the less often radiation damage to the lungs appears. Peripheral areas suffer more from radiation exposure.
- Taking medications: Methotrexate , Amiodarone , Proctolol (fibrosis can develop many months after the end of treatment with this drug), Propranolol (pleural fibrosis is possible). When taking nitrofurans, fibrosing alveolitis develops, and Methysergide and Ergotamine cause pleural sclerosis.
Symptoms
The main complaint with slow-onset pulmonary fibrosis is shortness of breath, which occurs initially during physical exertion. As the process progresses, shortness of breath increases, which leads the patient to disability: he cannot care for himself, walk, or even pronounce a phrase. For some, the disease progresses slowly, so patients gradually adapt to their condition by reducing physical activity. A common symptom of pulmonary fibrosis is a dry cough, which is observed in 75% of cases; much less often, patients are bothered by a cough with sputum. In severe forms of the disease there may be purulent sputum. Pain and discomfort in the chest are less common. Fever and hemoptysis are not characteristic symptoms of idiopathic fibrosis.
Common symptoms include: weakness, fatigue, changes in nail phalanges, weight loss. When listening to a patient with a phonendoscope, the doctor determines crepitus (“crackling of cellophane”), which is heard at the height of inspiration in the posterior lower sections. Exacerbation of idiopathic fibrosis is a serious condition that threatens the patient’s life, since respiratory failure rapidly increases and death occurs in 85% of cases.
In general, symptoms are determined by the underlying disease against which pulmonary fibrosis developed. For example, in silicosis they are scant and nonspecific: cough, shortness of breath on exertion and sputum. With this disease, you should pay attention to the severity of changes on x-rays and the paucity of the patient’s complaints. With the formation of large fibrous nodes and involvement of the pleura, complaints of tingling between the shoulder blades and pain in the chest appear. With chronic bronchitis, patients are bothered by coughing with sputum.
Life prognosis for patients
The prognosis for pulmonary fibrosis is very ambiguous. Timely treatment helps to significantly slow down the development of the pathological process.
If the disease is advanced and a complication such as a lung abscess (purulent melting of tissue) occurs, then the patient’s prognosis for life worsens significantly.
The quality of life progressively decreases with pulmonary fibrosis, which was provoked by tuberculosis.
A lethal outcome is most often observed in the case of a secondary infection, the development of a severe form of sepsis or pulmonary tuberculosis.
Tests and diagnostics
The following are used in diagnostics:
- Fluorography and radiography of the lungs . Fluorography is used as a screening method. Fibrosis of the roots of the lungs on a fluorogram is observed in bronchitis , smoker's bronchitis, and occupational lung diseases. On the fluorogram it looks like this:
With pneumoconiosis, an altered pulmonary pattern is determined due to diffuse fibrosis, which has a mesh or cellular shape, mainly in the lower and middle sections. Linear darkening of irregular shape is also detected, reflecting fibrosis around the bronchi and vessels. With tuberculosis in the upper lobes, thickening and deformation of the pulmonary pattern are determined, there may be linear pneumofibrosis, and a fibrous path extends to the root of the lung. In cirrhotic tuberculosis, fibrotic changes predominate over the prevalence of encapsulated lesions.
A single fibrous cord in the lungs, as an x-ray sign, is detected after an inflammatory process (pneumonia, tuberculosis). A single fibrous cord is not dangerous and does not affect respiratory function, although its reverse development does not occur. Much more dangerous is the widespread (diffuse) tractable pneumofibrosis, which forms with idiopathic fibrosing alveolitis . Then diffuse changes appear in the form of fine-mesh deformation of the pulmonary pattern.
They are bilateral in nature and are expressed in the parts of the lungs above the diaphragm. A decrease in lung volume is characteristic, which is why the diaphragm dome is high. As the disease progresses, fibrotic changes and respiratory failure progress.
- A highly sensitive method for detecting pulmonary fibrosis is high-resolution computed tomography (HRCT). It is this that allows us to determine its severity, prevalence, nature and dynamics of changes. The use of thin sections and spatial reconstruction with this method increases the capabilities of spatial imaging. The CT picture of idiopathic pulmonary fibrosis at the early, exudative stage is represented by ground-glass opacities. Subsequently, bilateral basal changes in the form of a “honeycomb lung” and traction bronchiectasis . The picture of a “honeycomb lung” is given by cysts of 3-10 mm with thick and clear walls.
- Transbronchial cryobiopsy of an organ, which is comparable in accuracy to surgical biopsy.
- Study of external respiration function. A decrease in the elastic properties of the lungs due to the development of large fibrous fields and thickening of the interalveolar septa is manifested by restrictive disorders, a decrease in forced expiration and vital capacity of the lungs.
Diagnostic measures
Diagnostics combines:
- One of the most important diagnostic methods is radiographic examination. The study allows you to determine changes in your own lung tissue and its replacement with fibrous tissue. The images accurately determine the area and extent of the lesion;
- Computed tomography and MRI;
- Angiopulmonography. The study allows you to evaluate blood flow in the pulmonary vessels, changes in the vascular system of the organ;
- Spirography. The study reveals a decrease in the mechanical abilities of the respiratory organs, assesses the degree of decrease in inspiratory volume, determines the increase in respiratory rate;
- Lung biopsy is the most informative method. For the study, several samples of biomaterial are taken.
Treatment of pulmonary fibrosis
How to treat pulmonary fibrosis? There is no specific treatment for fibrosis and its reverse development does not occur. However, attempts are being made to influence it. Its development can be stopped if pneumofibrosis is the outcome of inflammatory or autoimmune diseases of the bronchopulmonary system, which occur with periodic exacerbations. If you carry out treatment that eliminates inflammation (including immune inflammation) and improve the drainage function of the bronchi, you can stop the progression.
In acute interstitial pneumonia during the inflammatory reaction (alveolitis - the equivalent on CT is “ground glass”), corticosteroids . Most patients with idiopathic pulmonary hemosiderosis also show a positive response to treatment with glucocorticosteroids - this is manifested by a decrease in the frequency of exacerbations and the rate of development of fibrosis.
For idiopathic pulmonary fibrosis, low-dose prednisolone and cyclophosphamide . However, there is no definitive evidence that survival in these patients is improved by treatment with prednisolone alone or with combination therapy. At the same time, the risk of developing adverse reactions is higher than the likelihood of improving lung function. The only drugs with proven effectiveness that exhibit an antifibrosing effect in this disease are pirfenidone ( Esbriet ) and nintedanib ( Vargatef ). They attenuate fibroblast proliferation and fibrosis progression. Other drugs have shown their effectiveness in animal experiments - cyproheptadine and ketanserin suppressed collagen synthesis and prevented the deposition of fibrotic masses in lung tissue.
Attempts are being made to influence pulmonary fibrosis with drugs that have enzymatic activity. Thus, Longidase in suppositories (containing the enzyme testicular hyaluronidase) as monotherapy or as part of complex treatment. Research has proven that this drug does not act on normal connective tissue, but destroys altered tissue in the area of fibrosis. Longidaza also has antioxidant and anti-inflammatory properties and has a long-lasting effect due to the polymer carrier in the formative base of the candle.
When administered rectally, the drug penetrates all organs and tissues. In pulmonology and phthisiology, 1 suppository is used every 2-3 days; 10-20 injections are recommended. If necessary, you can repeat the course after three months, and then switch to long-term (3-4 months) maintenance treatment - 1 suppository once a week. Longidaza can also be used in the form of injections of 3000 IU: for the first 3 months - 3000 IU (1 injection) every 4 days, then for 3 months, 1 injection every two weeks.
The basic treatment of all bronchopulmonary diseases accompanied by shortness of breath (COPD, bronchial asthma) is bronchodilators, since bronchial obstruction occurs with pneumosclerosis .
Taking bronchodilators reduces the severity of shortness of breath and increases exercise tolerance. Bronchodilators of various groups are used: beta-2 agonists , M-anticholinergics and methylxanthines . From the group of M-anticholinergics, the most commonly used are: ipratropium bromide ( Atrovent , Ipratropium-native , Ipratropium Air ) and tiotropium bromide ( Spiriva , Tiotropium-native ).
Beta-2 agonists act quickly and improve well-being in the short term, but resistance develops with long-term use. Therefore, it is recommended to take a break from use, after which the bronchodilator effect of this group of drugs is restored. If these two groups of drugs are insufficiently effective, methylxanthines ( Diaphylline , Euphylline , Theophylline and prolonged-release drugs) are added to treatment. They strengthen the work of the respiratory muscles and reduce pulmonary hypertension.
The effectiveness of combined treatment with indacaterol and glycopyrronium bromide in slowing the development of fibrosis in COPD has been noted. This combination blocks the fibrotic response in the body that occurs in patients with COPD. The inhalation drug Ultibro Breezhaler contains a combination of these two substances, which quickly and for a long time (24 hours) cause relaxation of the bronchial muscles and provide a bronchodilator effect. Ultibro Breezhaler is the main drug of choice in the treatment of COPD, the use of which improves lung function, reduces the frequency of exacerbations and increases exercise tolerance.
Mucolytics (mucoregulators, mucokinetics) are not indicated for all patients with bronchopulmonary diseases - only during exacerbation and bronchial obstruction due to poor sputum separation. If the sputum is purulent and its quantity increases, antibiotics are prescribed. General strengthening agents and vitamins are also indicated.
Considering the irreversibility of the process, treatment of pulmonary fibrosis with folk remedies is ineffective. Plant materials can be used as expectorants, mucolytics and restoratives in the complex treatment of patients.
Breathing exercises
Excellent helpers for pulmonary fibrosis are breathing exercises that help improve the functioning of the respiratory system, strengthen the entire body due to the supply of oxygen to collapsed areas of the lungs.
There are many good methodical exercises to strengthen the respiratory system, for example, the Buteyko and Strelnikova methods. But you don’t need to stick to only these methods; you can do easier breathing exercises, for example, inflating balloons. And for greater effect from such exercises, it is better to carry them out in the fresh air or in a well-ventilated area.
Here are some great exercises:
- Take a deep breath, hold your breath for a while and slowly exhale;
- While inhaling, slowly raise your hands up, exhale sharply and slowly lower your hands with the sound “ha”;
- Inflate balloons several times a day for about 1-2 minutes;
- A good exercise is to blow through a tube lowered into water for about 2-3 minutes;
- Standing, feet shoulder-width apart, slowly lean forward, at the same time spread your arms to the sides, while bending, inhale with your stomach pulled in;
- The next exercise should be performed lying on your back (can be on the floor), exhale through your mouth, slightly pressing your hands on the diaphragm.
In conjunction with the described breathing exercises, you can do other gymnastics that help better ventilation of the lungs, for example, if pulmonary fibrosis is associated with bronchitis or pneumonia.
But remember one rule - you should not do too difficult gymnastics in an acute form of the disease, first wait for the body to recover a little, and then, if it improves, start doing gymnastics.
Medicines
- Bronchodilators: Atrovent , Ipratropium-native , Ipratropium Air , Spiriva , Tiotropium-native , Ultibro Breezhaler .
- Mucolytics: Acetylcysteine , Eucabal , Bronchomucin , Fluditec , Ambrol , Ermucin , Lazolvan .
- Glucocorticoids: Prednisolone .
- Antitumor drugs (cystatics): Cyclophosphamide .
Procedures and operations
During any exercise, the heart and lungs work actively. Special breathing exercises are aimed at increasing the functionality of the lungs, reducing shortness of breath and increasing exercise tolerance. The complex should include exercises for training diaphragmatic breathing and exercises with forced exhalation. You can take breathing exercises according to the method of P. A. Buteyko as a basis. The duration of breathing exercises is 10 minutes, and you need to perform it 3-5 times during the day. The ideal option is individually selected gymnastics. If the condition of the respiratory system allows, you can engage in race walking.
Among the procedures, oxygen replacement therapy is indicated, which is carried out when the blood oxygen pressure decreases to less than 60 mm Hg. Art. In case of chronic respiratory failure, oxygen therapy is carried out at home for a long time (18 hours a day) in a low-flow (2-5 l/min) oxygen supply mode. In case of severe respiratory failure, helium-oxygen mixtures are used. Oxygen concentrators are used at home.
To remove circulating immune complexes from the blood (especially in bronchial asthma ), hemosorption .
other methods
Healing aloe
Traditional healers and their healing methods are a great assistant to therapists, but only as an addition to the main treatment.
The specialist himself will prescribe, if the diagnosis reveals pulmonary fibrosis, herbal treatment, and they will help improve breathing, ease shortness of breath, and strengthen the immune system.
Among the medicinal indoor plants is the popular aloe vera. Its leaves contain a lot of vitamins and microelements. Tinctures, mixtures and rubbings are made on its basis.
In combination with the use of medications, having received medical approval, and only scars after tuberculoma remain on the lungs, the condition of pulmonary fibrosis will improve if you include in the nutritious diet (3 times a day, 25 grams) a mixture consisting of the following ingredients:
- domestic lamb or any animal fat – 100 gr.
- walnut – 100 gr.
- honey – 100 gr.
- aloe leaves – 100 gr.
It is very easy to make a homogeneous mass; all solid elements are twisted in a meat grinder. Melt the internal fat and honey over low heat, do not bring to a boil and mix thoroughly.
The prepared tincture cleanses the respiratory tract well:
- you will need red wine -1 glass
- honey – 2 tbsp. l.
- aloe leaves – 6 large leaves
The leaves are chopped, added to wine, mixed with honey. All received products are stored in a cold place, used before eating, but no more than three times a day and no more than 1 tablespoon.
Eucalyptus is used as an antiseptic. It has many therapeutic effects for various pulmonary diseases, heart ailments, and nervous breakdowns.
It is very easy to make a medicinal potion with its leaves. You need to take boiling water and put the crushed plant there; you can use it immediately after 20 minutes. To enhance the effect, add honey to the solution.
Application does not require time restrictions, but to avoid accumulative formations, it is better to change the herbs after a month of use.
The use of common pikulnik and creeping thyme also has a beneficial effect on the body and respiratory tract. The manufacturing method is identical to eucalyptus; the herbs are simply brewed like tea.
A decoction of oat grains is considered a therapeutic method for pulmonary pathology. It is also consumed before meals. To do this, pour the cereal (1 glass) with water (1 liter) at night, and before breakfast the solution is heated to a boil and continued to be heated until the water is reduced by half. You can drink the strained broth warm.
There are many tips to alleviate the plight of a sick person, but the surest one is turning to a professional.
Consequences and complications
The progressive course of pulmonary fibrosis has the following complications:
- Respiratory failure.
- Pulmonary hypertension with a gradual increase in pressure in the pulmonary circulation. Secondary pulmonary hypertension always develops with fibrosis and appears in the first years of the disease. In the early stages it is asymptomatic. Then there is an increase in shortness of breath, the severity of which depends on the degree of pressure in the pulmonary artery.
- Emphysema.
- Lung cancer . Inhalation of asbestos fibers induces the development of not only fibrosis, but also pleural and lung cancer. Lung cancer can also develop against the background of idiopathic alveolar fibrosis.
- The formation of fibrous cavities and cysts, which are complicated by pulmonary hemorrhage , pneumothorax (entry of air into the pleural cavity due to damage to the lung) and pneumomediastinum (accumulation of air in the mediastinal tissue due to rupture of the lung, which leads to compression of the heart and large vessels).
Flow options
There are no official stages of IPF, but doctors use terms such as mild, moderate or severe.
Easy stage
At this stage, people may experience mild symptoms of IPF and be initially diagnosed. In some cases, people may not have any symptoms.
Moderate stage
At this stage, a lot of scarring occurs in the lungs and oxygen therapy may be required.
Severe stage
Symptoms at this stage are severe and a lung transplant may be required.
Forecast
The prognosis and life expectancy for pulmonary fibrosis depends on the disease against which it developed, the degree of progression of the fibrosis itself, its extent and the degree of involvement of the bronchial tree (meaning the formation of bronchiectasis, which aggravates the course of the disease). Among the prognostic criteria, the main one is the type of formation of pulmonary fibrosis.
Favorable types include fibrous changes in the form of cords in the central and peripheral interstitium of the lungs, as well as the atelectatic type of fibrosis. The latter is formed in places of organized pneumonia or at the site of long-term collapse of lung tissue as a result of closure of the bronchi. The occurrence of these types of pulmonary fibrosis does not affect perfusion and diffusion in the lungs and does not lead to the development of respiratory failure. Unfavorable types include changes in the form of acinar fibrosis and honeycomb lung, which always lead to impaired perfusion and severe respiratory failure. It is this factor that reduces the patient’s life expectancy.
Honeycomb lung and its significant prevalence are considered the most unfavorable prognostic sign. At the same time, importance is attached to the size of the “honeycombs” - large “honeycombs” or a mixed type of structure with alternating small and large cysts are considered more unfavorable. As for their localization, the lower zonal location is considered unfavorable.
The natural history of idiopathic fibrosis is associated with gradual changes in lung tissue and progressive fibrotic damage, which at the final stage takes on the appearance of a “honeycomb lung”. Increasing fibrosis progressively worsens the patient's condition and affects life expectancy.
It is difficult to answer the question of how long people live with this disease, since it depends on the state of pulmonary function. Terms can range from 2 to 6 years. Thus, in acute cases, patients live no more than 2 years, in subacute cases - from 2 to 4 years, and in chronic cases - from 4 to 6 years. The situation is aggravated by concomitant diseases that arise with age. Death is caused not only by the development of acute respiratory failure, but also by ischemic heart disease, pulmonary embolism or lung cancer .
With slowly progressing silicosis, the prognosis for life is positive, since the process of transition from one stage to another can last decades. There are cases when the progression of fibrosis is not detected at all - in such cases the prognosis for life is favorable. A severe complication of silicosis is spontaneous pneumothorax , but it is very rare in modern forms of silicosis. tuberculosis develops against the background of silicotic fibrosis , then the course of the disease is unfavorable and, in general, the prognosis depends on the severity of tuberculosis and silicosis, and the form of tuberculosis.
Physiotherapy of pneumofibrosis
During the treatment of pulmonary fibrosis, the most important task is to eliminate all its causes. If pneumonia is detected, then antibacterial therapy must be started immediately. Various medications are often prescribed along with physical therapy. Pneumofibrosis or pneumonia should be treated until complete clinical and radiological recovery. And after complete recovery, people must remain registered with a specialist for a whole year.
But in addition to drug treatment, patients with this disease are prescribed physical therapy. Iontophoresis and ultrasound with medicinal ingredients can be used as physiotherapy. This treatment gives excellent results.
And sometimes, oxygen therapy is prescribed, in which oxygen is supplied to the lungs through a machine. As much oxygen is supplied as is contained in the surrounding space.
List of sources
- Ivanova A. S. Fibrosing processes / A. S. Ivanova, E. A. Yuryeva, V. V. Dlin. M.: Overlay, 2008. 196 p.
- Idiopathic fibrosing alveolitis / M. M. Ilkovich [et al.] // In the book: Disseminated lung diseases / Ed. M. M. Ilkovich. M.: GEOTAR-Media, 2011. pp. 24–84. 3.
- Avdeev SN. Idiopathic pulmonary fibrosis: modern approaches to therapy. Practical Pulmonology 2015;1 22–31.
- Tsvetkova O.A., Voronkova O.O. Modern approach to the treatment of patients with idiopathic pulmonary fibrosis. Clinical Med 2017;95:281–5. 31.
- Aisanov Z.R., Kokosov A.N., Ovcharenko S.I., Khmelkova N.G., Tsoi A.N., Chuchalin A.G., Shmelev E.I. Chronic lung diseases. Federal program. RMJ, 2001; No. 1: p. 9 – 33.