What is arachnoiditis?
Arachnoiditis is an inflammation of the middle layer (arachnoid) of the meninges, which is the protective covering surrounding the brain, spinal cord, and nerve roots of the cauda equina.
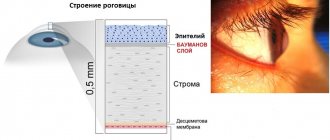
The meninges (the lining of the spinal canal) are connective tissue composed primarily of collagen and elastin. Damage, trauma, tumor or infection can cause inflammation of the arachnoid layer anywhere.
Arachnoiditis has been known since the 19th century, when its main causes were infections, mainly tuberculosis and syphilis. It has now become known that the dissolution and degeneration of the arachnoid layer is caused by genetic and autoimmune disorders.
Examination and diagnosis
In order to radically solve the problem of arachnoiditis once and for all, one must understand its true causes. Only then can we talk about real healing. Therefore, treatment in our clinic will begin with a thorough examination, questioning, and studying the results of previously performed studies. Be sure to take with you to the clinic all the medical documents available to you, even those that, at first glance, are not directly related to arachnoiditis (certificates, extracts, epicrises, tests, pictures, ultrasound, ECG, EEG, etc.).
MRI of the brain allows you to see arachnoid cysts, a cystic-adhesive process in the membranes of the brain. Signs of inflammation in the paranasal sinuses and hearing organs are also clearly visible.
We perform blood tests Tests help to find and properly treat the causes of inflammation of the arachnoid membrane.
Neurological examination with examination of reflexes, sensitivity, coordination sphere, autonomics, with a detailed interview of the patient. A complete neurological examination gives the doctor more relevant information about the function of the nervous system than even an MRI scan. We compare the data obtained with the data of analyzes and MRI, on the basis of which we establish a diagnosis. True arachnoiditis is rare; upon examination it is not always confirmed; often we discover and treat another, true cause of the ailment .
Electroencephalography (EEG) to assess the general condition of the brain and look for epileptic discharges.
Examination of cerebral vessels to assess the sufficiency of cerebral circulation.
Signs and symptoms of arachnoiditis
— Natural history of the disorder.
Without treatment, arachnoiditis has a somewhat unpredictable natural history. Some cases may resolve naturally and do so entirely without any evidence that they existed. However, once a diagnosis is made, the disease can be classified as a mild, mild, severe, or catastrophic case.
A mild case , for example, is one in which the pain is intermittent and there is no impairment of bladder function or range of motion of the limbs.
A moderate case is one with constant but easily controlled pain, accompanied by some bladder dysfunction and lower limb weakness.
A severe case will require daily pain medication as the pain is severe, constant and intractable. There is impaired bladder function, the inability to sit or stand in one position for more than a few minutes, as well as weakness and paraparesis (partial paralysis) of the lower extremities.
A catastrophic case will have all the elements of a severe case plus paraparesis (partial paralysis) of the lower extremities, cognitive impairment, severe fatigue, largely associated with bed or couch confinement, and the need for assistance to perform activities of daily living. If untreated, catastrophic cases of arachnoiditis leave the patient with a shortened life expectancy, autoimmunity, and terminal events typically associated with overwhelming infections or heart failure.
The main goal of modern treatment is to prevent the disease from progressing from mild or moderate severity to catastrophic disease.
The severity of arachnoiditis is directly related to the intensity of glial cell activation and neuroinflammation in the nerve roots of the cauda equina. Examination of serum for neuroinflammatory markers shows that neuroinflammation ranges from high intensity to relatively benign or inactive. Thus, the natural, untreated course of events is unpredictable. In addition to spontaneous resolution, some cases, for unknown reasons, have active neuroinflammation that resolves or “dies off” but leaves behind permanent neurological impairment and pain. Most cases that come to the attention of modern doctors tend to be progressive, with alternating periods of remission and activity.
The catastrophic stage of arachnoiditis may disappear, probably due to medical and physical measures that do not treat or eliminate the disorder, but seem to prevent its most catastrophic and devastating complications, such as paraplegia, adrenal insufficiency, severe autoimmunity, immunodeficiency and early , life-ending infections and sepsis.
— Symptoms.
A typical symptom complex of arachnoiditis is constant pain with various neurological manifestations. The intensity of the pain may vary as you move between sitting, reclining, or standing positions. People with arachnoiditis may achieve comfort by standing or lying down, or the situation may be just the opposite, either sitting or lying down may increase pain. In addition to positional pain relief, other symptoms experienced by most patients include the sensation of dripping water and/or insects crawling on the legs. Burning sensation in the lower legs is also common. There are some symptoms of difficulty urinating. These may include hesitancy to start or difficulty stopping urination (neurogenic bladder).
Many patients complain of blurred vision, headache and dizziness, which are believed to be caused by obstruction of the flow of cerebrospinal fluid. The narrowing of the spinal canal, as well as the clots and scar tissue present in the spinal canal, act as a “dam” that prevents the constant flow of fluid. Cerebrospinal fluid may leak or, more appropriately, “leak” through the arachnoid and dura layers of the lining of the spinal canal into the soft tissue surrounding the spinal canal. Cerebral spinal fluid is extremely toxic to soft tissue, so significant pain can develop, and soft tissue, including muscles, nerves, and fascia, can degenerate, scar, and shrink after contact with the leaking fluid.
Kinds
Depending on the location of the pathological process, clinicians distinguish the following types of arachnoiditis:
Cerebral arachnoiditis
Cerebral arachnoiditis is a direct inflammation of the choroid of the brain. Most often, the focus of inflammation forms on the convex surface of the brain, at its base or in the region of the posterior cranial fossa.
Characteristic symptoms are severe headaches, which tend to intensify after a person has been exposed to the cold for a long time, after physical and mental stress. Neurological symptoms of pathology directly depend on the location of the lesion. If arachnoiditis affects the convexital surface of the brain, then progression of convulsive seizures is possible.
If treatment for cerebral arachnoiditis is not started in a timely manner, generalized convulsive seizures may subsequently occur, during which the person will lose consciousness. If the accumulated cerebrospinal fluid begins to put pressure on the sensory and motor centers of the brain, then the person will begin to develop motor activity disorders, and sensitivity will also decrease.
Optico-chiasmatic arachnoiditis
Opticochiasmatic arachnoiditis is also often called post-traumatic. As a rule, it develops due to head injury, against the background of the progression of malaria, syphilis, and tonsillitis. Such brain arachnoiditis is usually localized near the inner part of the optic nerves and chiasm. As a result of the progression of pathology, adhesions and cysts form in these places.
If an examination is carried out at the moment, the doctor will be able to identify signs of congestion and neuritis in the fundus area. Arachnoiditis of the posterior cranial fossa is the most common form of pathology. The following symptoms are noted: nausea, vomiting, headaches, which are more pronounced in the occipital region.
Spinal arachnoiditis
In this case, inflammation of the choroid of the brain progresses due to abscesses, furunculosis, and injuries. Typically, inflammation progresses along the posterior surface of the spinal cord. Symptoms of the disease may appear in a person some time after a previous injury. The pathology is characterized by the appearance of pain in the upper and lower extremities.
Adhesive arachnoiditis
In the case of adhesive arachnoiditis, purulent inflammation develops, which leads to the formation of adhesions.
Cystic arachnoiditis
The inflammatory process is accompanied by the formation of a cyst. A characteristic symptom is severe and bursting headaches.
Cystic adhesive arachnoiditis
The disease is characterized by the formation of pathological areas in the brain. In them, the choroid will stick together with the soft membrane, and adhesions and cysts will form. As a result, seizures may develop.
Causes of arachnoiditis
In the 21st century, there are 4 main causes of arachnoiditis:
- anatomical disorders of the spine;
- genetic connective tissue diseases;
- bruises, injuries;
- autoimmune disorders.
Arachnoiditis can begin with damage to the arachnoid membrane or nerve roots of the cauda equina. No matter where the damage begins, eventually the adhesions will adhere or glue the nerve roots and arachnoid membrane together, causing severe pain and impairment.
The spinal cord ends at the top of the lumbar spine and develops into a dozen nerve roots. They float freely in the spinal cord canal ("tube") and are collectively known as the cauda equina. At some point along the lumbar and sacral spine, nerve roots individually branch off to connect and activate the feet, legs, bladder, genitals, intestines and stomach.
Any anatomical change that causes the spinal canal to narrow, bend, or otherwise distort the spinal canal in the lumbosacral spine can eventually cause arachnoiditis.
The spinal canal, which contains cerebrospinal fluid, should always remain open and free from obstruction. Spinal fluid is produced in the brain and is replenished approximately 4 times a day. It leaves the brain to enter the spinal canal. The function of cerebrospinal fluid is to transport nutrients, remove contaminants such as byproducts of inflammation, and lubricate and continually bathe the nerve roots of the cauda equina to prevent them from rubbing against each other. This can cause irritation, neuroinflammation, scarring and adhesion.
Pathological anatomy and pathogenesis
Rice.
1. Arachnoid cysts of the spinal cord (in the left picture - at the top, in the right picture - in the center). The arachnoid membrane with arachnoiditis becomes thickened, dense and acquires a grayish-white color. Adhesions form between it and the soft shell. The same adhesions often occur between the arachnoid and dura mater. The adhesive process leads to the formation of arachnoid cysts (Fig. 1), containing cerebrospinal fluid. If the cyst exists for a long time, its walls gradually become thicker and denser, and it turns into a tumor-like formation. The cyst fluid may become xanthochromic and contain large amounts of protein. The dura mater in the area of the pathological process is tense, swollen, thickened, rich in blood vessels, and loses its luster. Arachnoiditis often leads to occlusion of the cerebrospinal fluid pathways and secondary cerebral hydrops. Spinal arachnoiditis can cause blockage of the subarachnoid space of the spinal canal.
Rice. 2. Rough thickening of the arachnoid membrane with the formation of fibrous cords of various sizes. Rice. 3. Diffuse cellular infiltration of the arachnoid membrane.
Microscopic examination of the arachnoid membrane reveals fibrosis (Fig. 2) of varying degrees (thickening, coarsening of argyrophilic fibers, collagenization), hyperplasia of the endothelium of the membrane, infiltration of it with lymphoid elements (Fig. 3), proliferation of fibroblasts; vessels from the dura and choroid grow into the arachnoid membrane. In the soft shell there is hyperemia, new formation of blood vessels, inflammatory infiltration, and subsequently fibrosis. In adjacent areas of the brain, secondary changes are found caused by the pressure of meningeal cysts and adhesions, disorders of liquor and blood circulation, as well as the direct transition of the inflammatory process to the substance of the brain. Often severe arachnoiditis is complicated by periventriculitis and ependymitis.
Arachnoiditis in some cases occurs under the influence of exposure to the membranes of the pathogen itself, in others - its toxins. In case of injuries, the main role is played by disorders of blood and liquor circulation in the membranes and subarachnoid space. Dynamic disorders of blood and liquor circulation, swelling of adjacent areas of brain tissue and membranes explain the remissions and deteriorations that characterize the clinical picture of arachnoiditis.
Pathomorphological changes - from mild fibrosis of the arachnoid membrane to the formation of large cysts, numerous rough moorings in which all membranes are involved, and necrosis in the substance of the brain - make clear the varying severity of individual cases and the extremely unequal availability of their therapy.
Affected Populations
Individuals who have had spinal surgery, intrathecal injections of toxic fluids (eg, hyaluronidase, blood, dyes, steroids, and local anesthetics with preservatives) into the spinal sac, or have injuries to the spine and head may be at greater risk of developing this disorder.
However, the exact prevalence and incidence of arachnoiditis is unknown. One estimate is that approximately 11,000 new cases occur each year; however, the cause may vary from back surgery, pain relief procedures, and diagnostic procedures performed primarily in the Americas, Europe, and Asia, with an undetermined number in Africa.
It is clear that more surgical and anesthetic spinal interventions have significantly increased the number of cases. For various reasons, some cases of arachnoiditis may be misdiagnosed or undiagnosed, making it difficult to determine its true incidence in the general population.
Associated disorders
There are numerous conditions characterized by signs and symptoms that are similar to those found in arachnoiditis, however, only a few will be listed. These include failed back surgery syndrome, multiple sclerosis, fibromyalgia, reflex sympathetic dystrophy, chronic pain syndrome, cauda equina syndrome, syringomyelia, and some spinal cord tumors.
In many cases, certain conditions can occur as complications of arachnoiditis, making diagnosis more difficult. Sometimes the symptoms experienced by some people with arachnoiditis may be dismissed as psychosomatic , and these patients may be labeled as cases of "pain in your head".
Diagnostics
— Laboratory tests.
There are currently no specific laboratory tests that identify a patient with arachnoiditis. Because the condition is a neuroinflammatory disease, certain byproducts of inflammation known as "markers" are often elevated. These include erythrocyte sedimentation rate (ESR); Myeloperoxidase C-reactive protein (CRP) and cytokines.
If any of these markers are elevated, treatment goals should include suppression of neuroinflammation and reduction of the affected marker(s) to normal serum levels. It is emphasized that the absence of elevated inflammatory markers does not necessarily mean that neuroinflammation is either controlled or absent.
Some adrenal and gonadal hormones, such as cortisol, testosterone, and pregnenolone, may be decreased in serum due to severe stress and pain in arachnoiditis. Low serum hormone levels are considered indicators that the disease process is poorly controlled.
— Diagnosis of adhesive arachnoiditis.
Diagnosis requires 4 elements:
- history of the inciting event or illness;
- typical symptoms;
- abnormal physical signs;
- MRI results.
Specific features of arachnoiditis are usually recognized by contrast-enhanced MRI, which uses injected dye or high-resolution Tesla imaging (3) to contrast the cerebrospinal fluid from the spinal cord, nerve roots, and arachnoid covering.
Necessary evidence for diagnosis is the presence of nerve root lumps and adhesions that attach the lumps to the arachnoid layer of the covering of the spinal cord. While other findings, such as nerve root displacement, enlargement, and asymmetry, may be present on MRI imaging, these findings alone are not sufficient to make a diagnosis.
Prices
| Disease | Approximate price, $ |
| Prices for diagnosing migraine | 7 060 — 8 260 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for brain shunting for hydrocephalus | 33 180 |
| Prices for treatment of Parkinson's disease | 58 600 |
| Prices for migraine treatment | 9 680 |
| Prices for the diagnosis of amyotrophic lateral sclerosis | 6 550 |
| Prices for diagnosing epilepsy | 3 520 |
| Prices for rehabilitation after a stroke | 78 300 — 82 170 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of multiple sclerosis | 4 990 — 17 300 |
Treatment of arachnoiditis
Until recently, arachnoiditis was often called an “untreatable” and “hopeless” condition. However, two major scientific discoveries have led to the development of a “first generation” medical process or protocol for its treatment.
The first discovery is that neuroinflammation is caused by the activation of cells in the brain and spinal cord called glia. Pain, injury, infection, or exposure to foreign chemicals or metals (such as those that may be introduced into the cerebrospinal fluid by medical interventions and surgical procedures) can activate glial cells, causing neuroinflammation. Following these discoveries, several drugs and hormones have been identified that will suppress glial cell activation and neuroinflammation.
The second discovery is that the brain and spinal cord produce certain hormones called neurohormones, whose main functions are to suppress neuroinflammation and/or regenerate damaged nerve cells. Some are called "neurosteroids" because they contain a steroid chemical structure. These include:
- pregnenolone;
- allopregnanolone;
- progesterone;
- dehydroepiandrosterone;
- estradiol
External administration of some of these internal hormones has been demonstrated to control neuroinflammation and promote neuroregeneration in laboratory animals. Administration of some of these hormones and their chemical analogues is currently used to treat arachnoiditis.
The treatment process consists of two main elements:
- drug treatment;
- physical measures.
Medicines consist of 3 therapeutic classes: (1) suppressors of neuroinflammation (examples: ketorolac, methylprednisolone); (2) neuroregenerating agents (examples: pregnenolone, nandrolone); and (3) pain relievers (examples: low-dose naltrexone, gabapentin, opioids).
Physical measures are aimed at maximizing the flow of cerebrospinal fluid and preventing scarring and contraction of nerve roots, muscles and other potentially affected cells that can cause neurological damage and pain. Basic physical interventions include daily walking, gentle stretching of the limbs, hydration, deep breathing and athletics.
Pain control for arachnoiditis is symptomatic and largely consistent with standard pain management. Unfortunately, the pain of this condition can rival or exceed that of metastatic bone cancer and, as necessary, require extreme, symptomatic measures such as implanted electrical stimulators and high-dose opioids, including those given by injection, suppositories, and implanted intrathecals. pumps
Today, many new pain treatments are being explored for severe, intractable pain like that caused by arachnoiditis. Some, such as intravenous infusions of lidocaine, vitamin C, and ketamine, have been reported to provide long periods of pain relief. While pain control is purely symptomatic, physical measures and medications to suppress neuroinflammation and promote neuroregeneration are used to permanently achieve some resolution of the disease and reduce symptoms and impairment.
Surgical intervention
If drug treatment does not produce the desired results, the patient experiences occlusive hydrocephalus or progressive vision loss, the doctor decides on surgical intervention. During the operation, adhesions are separated and cysts are removed. To reduce the manifestations of hydrocephalus, shunt operations are prescribed.
The prognosis for the patient is often favorable. Only arachnoiditis of the posterior cranial fossa, which is almost always accompanied by occlusive hydrocephalus, can pose a great danger. With frequent relapses of the disease, epileptic seizures and its optico-chiasmatic form, the labor prognosis for the patient may worsen.
Prevention
The finding that many cases are preceded by degenerative or structural abnormalities of the spine suggests that primary prevention of arachnoiditis is possible. It is well known that chronic degenerative spinal conditions are associated with sedentary lifestyle, obesity and lack of exercise.
People who develop low back pain with leg and bladder dysfunction immediately after a medical procedure, including a spinal tap, epidural, or surgery, are at high risk of developing arachnoiditis. In suspected cases and to prevent disease, it is recommended that the most potent antiviral anti-inflammatory drugs, such as ketorolac and methylprednisolone, be administered urgently to prevent the occurrence of arachnoiditis.