Pituitary adenoma is a tumor of the anterior lobe of this endocrine gland. The disease most often affects people aged 40-45 years. Among all brain tumors, a third of cases are pituitary adenomas. Pituitary microadenoma is a benign neoplasm growing from the glandular cells of the organ, the size of which does not exceed 10 mm.
Due to the small size of the tumor, symptoms of the disease with pituitary adenoma are absent for a long time. Doctors at the Yusupov Hospital identify the tumor using modern research methods. Early diagnosis and adequate treatment of pituitary adenoma allows patients to get rid of the disease.
The following types of adenoma are distinguished:
By size:
- microadenoma – less than 1 cm
- macroadenoma – more than 1 cm
- giant adenomas – more than 10 cm
By localization:
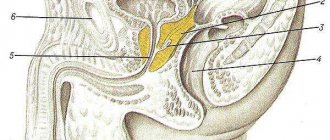
- not extending beyond the sella turcica - intrasellar
- growing to the apex of the sella turcica - endosuprasellar
- growing towards the bottom – endoinfrasellar
- growing sella turcica into the side – endolaterosellar adenoma
By hormone secretion:
- hormonally inactive tumors (about 40%)
- hormonally active adenomas (60%)
According to the nature of the hormones produced:
- somatotropinoma
- gonadotropinoma (FSH or LH)
- thyrotropinoma
- prolactinoma
- corticotropinoma
- mixed pituitary adenomas (produce several hormones at once, occur in 15% of cases)
According to statistics, pituitary adenomas make up 10–15% of all brain tumors. Adenoma occurs between the ages of 25 and 50 years, with equal frequency in men and women. Rarely, the disease can develop in children - 2-6% of all patients with adenoma are children and adolescents.
Prognosis for recovery
With microadenomas, the prognosis is good; the tumor is easier to treat than large tumors.
If a microadenoma is not sensitive to conservative therapy and surgery is prescribed, there is no need to be alarmed, because the possibility of complications with such a minimally invasive intervention is much lower than with the risk of progression of the tumor in the absence of treatment.
If the adenoma is hormonally inactive and has no symptoms, then the main task is regular monitoring of its condition.
What causes an adenoma to form?
Causes of pituitary adenoma:
- Neuroinfections: meningitis, encephalitis
- tuberculosis affecting the central nervous system
- brucellosis
- polio
- syphilis
Classification of the disease
Adenoma is the collective name for several types of pituitary benign formations of the anterior lobe. They are:
- inactive (do not form hormones), appear only in large sizes;
- hormone-producing – have the functions of pituitary cells.
The latter formations can produce various hormones. They are divided into the following types:
- prolactinoma (synthesizes prolactin);
- somatotropinoma (forms growth hormone);
- corticotropinoma (adrenocorticotropin);
- thyrotropinoma (thyrotropin);
- gonadotropinoma (produces follitropin and luteinizing hormones).
Symptoms
The signs that an adenoma may manifest vary depending on the type of tumor.
A hormonally active microadenoma manifests itself as endocrine disorders, while an inactive microadenoma can exist for several years until it reaches a significant size or is accidentally detected during examination for other diseases. 12% of people have asymptomatic microadenomas.
Macroadenoma is manifested not only by endocrine, but also by neurological disorders caused by compression of surrounding nerves and tissues.
Prolactinoma
The most common pituitary tumor occurs in 30-40% of all adenomas. As a rule, the size of prolactinoma does not exceed 2–3 mm. It occurs more often in women than in men. Manifested by such signs as:
- menstrual irregularities in women - irregular cycles, prolongation of the cycle for more than 40 days, anovulatory cycles, absence of menstruation
- galactorrhea - constant or periodic release of breast milk (colostrum) from the mammary glands, not associated with the postpartum period
- inability to get pregnant due to lack of ovulation
- In men, prolactinoma is manifested by decreased potency, enlarged mammary glands, erectile dysfunction, and impaired sperm formation, leading to infertility.
Somatotropinoma
Accounts for 20–25% of the total number of pituitary adenomas. In children, it ranks third in frequency of occurrence after prolactinoma and corticotropinoma. Characterized by increased levels of growth hormone in the blood. Signs of somatotropinoma:
- in children it manifests itself with symptoms of gigantism. The child quickly gains weight and height, which is due to the uniform growth of bones in length and width, as well as the growth of cartilage and soft tissue. Typically, gigantism begins in the prepubertal period, some time before the onset of puberty, and can progress until the end of skeletal formation (up to about 25 years of age). Gigantism is considered to be an increase in the height of an adult by more than 2 – 2.05 m.
- if somatotropinoma occurs in adulthood, it is manifested by symptoms of acromegaly - enlargement of the hands, feet, ears, nose, tongue, changes and coarsening of facial features, the appearance of increased hair growth, beards and mustaches in women, menstrual irregularities. Enlargement of internal organs leads to disruption of their functions.
Corticotropinoma
Occurs in 7 - 10% of cases of pituitary adenoma. Characterized by excess production of adrenal hormones (glucocorticoids), this is called Itsenko-Cushing disease.
Signs of corticotropinoma:
- “Cushingoid” type of obesity – there is a redistribution of the fat layer and fat deposition in the shoulder girdle, on the neck, in the supraclavicular areas. The face takes on a “moon-shaped”, round shape. The limbs become thinner due to atrophic processes in the subcutaneous tissue and muscles.
- skin disorders - pink-purple stretch marks (striae) on the skin of the abdomen, chest, thighs; increased pigmentation of the skin of the elbows, knees, armpits; increased dryness and flaking of facial skin
- arterial hypertension
- Women may have menstrual irregularities and hirsutism - increased skin hair growth, beard and mustache growth
- Men often experience a decrease in potency
Gonadotropinoma
Rarely found among pituitary adenomas. It manifests itself as menstrual irregularities, more often the absence of menstruation, decreased reproductive function in men and women, against the background of reduced or absent external and internal genital organs.
Thyrotropinoma
It is also very rare, occurring in only 2–3% of pituitary adenomas. Its manifestations depend on whether the tumor is primary or secondary.
- Primary thyretropinoma is characterized by symptoms of hyperthyroidism - weight loss, trembling of the limbs and the whole body, bulging eyes, poor sleep, increased appetite, increased sweating, high blood pressure, tachycardia.
- For secondary thyrotropinoma, that is, arising from long-term decreased function of the thyroid gland, hypothyroidism is characteristic - swelling on the face, slow speech, weight gain, constipation, bradycardia, dry, flaky skin, hoarse voice, depression.
Neurological manifestations of pituitary adenoma
- visual impairment - double vision, strabismus, decreased visual acuity in one or both eyes, limited visual fields. Significant sizes of adenoma can lead to complete atrophy of the optic nerve and blindness
- headache that is not accompanied by nausea, does not change with changes in body position, and is often not relieved by taking painkillers
- nasal congestion caused by germination of the sella turcica into the bottom
Leading clinics in Israel
Assuta
Israel, Tel Aviv
Ikhilov
Israel, Tel Aviv
Hadassah
Israel, Jerusalem
Many features of the hormones produced by the pituitary gland are not fully understood. The pituitary gland, and indeed the entire endocrine system, is so unique and complex that it still raises a lot of questions among specialists. But still, some hormones produced by the pituitary gland are, to a greater or lesser extent, known to us. Let's look at them:
- Thyroid-stimulating hormone – regulates the functioning of the thyroid gland;
- Adrenocorticotropic – responsible for the endocrine function of the adrenal glands;
- Follicle-stimulating hormone is a hormone that is responsible for the maturation of follicles in women, and therefore the ability to bear children;
- Luteinizing hormone - ensures the proper functioning of both male and female gonads. The production of the female hormone progesterone and the male hormone testosterone is also dependent on luteinizing hormone;
- Somatotropic – also called growth hormone;
- Prolactin is the main function of breast milk production. But besides this, this hormone has a number of other functions, such as the formation of secondary reproductive organs, suppression of ovulation during breastfeeding, etc.;
- Oxytocin is a hormone responsible for stimulating the muscles of the uterus during labor.
This list of functions of the pituitary gland is not final, but one thing is clear - the role of the pituitary gland is great and any deviation in its work leads to bad consequences for human health.
One of such deviations is a disease such as pituitary microadenoma.
Symptoms of pituitary insufficiency
Pituitary insufficiency may develop due to compression of normal pituitary tissue. Symptoms:
- hypothyroidism
- adrenal insufficiency – increased fatigue, low blood pressure, fainting, irritability, muscle and joint pain, impaired electrolyte metabolism (sodium and potassium), low blood glucose levels
- decreased levels of sex hormones (estrogens in women and testosterone in men) – infertility, decreased libido and impotence, decreased facial hair in men
- in children, lack of growth hormone leads to slow growth and development
Psychiatric symptoms
These symptoms of pituitary adenoma are caused by changes in hormonal levels in the body. Irritability, emotional instability, tearfulness, depression, aggressiveness, and apathy may be observed.
Possible complications
In advanced cases, the patient develops various complications.
The most common ones are:
- Diabetes.
- Incurable infertility
- Risk of miscarriage a few weeks after conception.
- Serious hormonal imbalance.
- Uncontrolled arterial hypertension.
- Tumors of the adrenal glands and thyroid gland.
- Exhaustion of the body.
- Muscle atrophy and complete immobility of the patient.
- Severe osteoporosis.
- Accidental fractures due to light load or careless movement.
Only proper treatment will help prevent complications.
Pituitary microadenoma is a serious disease accompanied by various disorders. Symptoms appear in women after a slight growth of the tumor and significantly worsen the quality of life. However, experts note that such tumors are easier to treat, and relapses occur less frequently, especially if you consult a doctor in a timely manner.
Article design: Vladimir the Great
Diagnosis of pituitary adenoma
If a pituitary adenoma is suspected, consultations with an endocrinologist, neurologist, neurosurgeon and ophthalmologist are indicated. The following diagnostic methods are prescribed:
Hormonal studies
- prolactin level in the blood, the norm is less than 20 ng/ml for women and less than 15 ng/ml for men
- test with thyrotropin-releasing hormone - normally, after intravenous administration of thyrotropin-releasing hormone, prolactin production increases at least twice within 30 minutes. Low levels of prolactin after thyrotropin-releasing hormone may indicate pituitary prolactinoma
- level of somatotropic hormone (GH) in the blood, the norm for children from one year to 18 years is 2 - 20 mIU/l, for men 0 - 4 mcg/l, for women - 0 -18 mcg/l.
- adrenocorticotropic hormone (ACTH) in the blood plasma, the norm in the morning at 8.00 o'clock is less than 22 pmol/l, in the evening at 22.00 less than 6 pmol/l, cortisol in the blood plasma in the morning 200 - 700 nmol/l, in the evening 55 - 250 nmol/l.
- daily rhythm of cortisol in the blood
- 24-hour urine test for cortisol levels, the norm is 138 – 524 nmol/day.
- study of electrolytes in the blood - sodium, potassium, calcium, phosphorus, etc.
- dexamethasone test - a study of cortisol levels in the blood and urine after taking large or small doses of dexamethasone
- level of follicle-stimulating hormone (FSH) in the blood, the norm in women is on the 7th – 9th day of the menstrual cycle 3.5 – 13.0 IU/l, on the 12th – 14th day – 4.7 – 22.0 IU/l, on the 22nd – 24th day – 1.7 – 7.7 IU /l. In men, FSH is normal – 1.5 – 12.0 IU/l.
- the level of luteinizing hormone (LH) in the blood, the norm is on the 7th – 9th day of the cycle 2 – 14 IU/l, on the 12th – 14th day – 24 – 150 IU/l, on the 22nd – 24th day – 2 – 17 IU/l. In men – 0.5 – 10 IU/l.
- serum testosterone in men, the norm of the total fraction is 12 – 33 nmol/l.
- level of thyroid stimulating hormone (TSH) and thyroid hormones (T3, T;) in the blood, normal – TSH – 0.4 – 4.0 mIU/ml, T3 – 2.63 – 5.70 pmol/l, T4 – 9.0 – 19.1 pmol/l.
- These standards may vary slightly in laboratories of different medical institutions
X-ray of the skull
MRI of the brain (in the absence of equipment - CT of the brain)
immunocytochemical study of pituitary adenoma cells
visual field examination
Reader reviews
Anonymous, Moscow. Hello! At the age of 11, my daughter experienced discharge from her nipples. We visited the doctor. A diagnosis of pituitary microadenoma was made. It was recommended to monitor prolactin levels. After 6 years, depression appeared. The psychiatrist prescribed tranquilizers. Hypoglycemia suddenly appeared. Today she has been diagnosed with secondary type 1 diabetes mellitus. Ultrasound shows no changes in the pancreas. After reading the article, I came to the conclusion that this diagnosis is associated with a pituitary microadenoma.
Anonymously. Pituitary microadenoma causes severe depression in me. I have to take antidepressants all the time.
Anonymously. A year ago, an MRI revealed a pituitary microadenoma. I take glucophage three tablets a day. I feel very bad. I associate this condition with this drug.
Anonymous, Tyumen. I have a pituitary microadenoma. I constantly want to sleep. Even after sleep I feel weak.
How to treat pituitary adenoma?
The choice of treatment method for each patient is determined individually, depending on the hormonal activity of the tumor, clinical manifestations and size of the adenoma.
For prolactinoma with a prolactin level in the blood of more than 500 ng/ml, drug therapy is used, and with a prolactin level of less than 500 ng/ml, or more than 500 ng/ml, but with no effect from medications, surgical treatment is indicated.
For somatotropinomas, corticotropinomas, gonadotropinomas, and hormonally inactive macroadenomas, surgical treatment in combination with radiation therapy is indicated. The exception is somatotropinomas with an asymptomatic course - they can be treated without surgery.
Danger and forecasts
For pituitary adenoma, the prognosis depends on the size of the tumor, the possibility of radical removal and its hormonal activity. With timely diagnosis and adequate treatment of the disease, recovery occurs in more than 85% of patients. If the duration of the disease is short, the likelihood of complete restoration of visual function is quite high.
In case of hemorrhage into the tumor, only the immediate intervention of a surgeon can save the situation. The sooner the patient goes to the Yusupov Hospital and receives specialized medical care, the greater the likelihood of a successful cure.
Surgery
There are two ways to surgically remove an adenoma^
- transsphenoidal - through the nasal cavity
- transcranial - with craniotomy
In recent years, in the presence of microadenomas or macroadenomas that do not have a significant effect on surrounding tissues, transsphenoidal removal of the adenoma is performed. For giant adenomas (more than 10 cm in diameter), transcranial removal is indicated.
Transsphenoidal removal of a pituitary adenoma is possible if the tumor is located only in the sella turcica or extends beyond it by no more than 20 mm. It is carried out after consultation with a neurosurgeon in a hospital. Under general anesthesia, the patient is introduced to endoscopic equipment (fiber optic endoscope) through the right nasal passage to the anterior cranial fossa. Next, the wall of the sphenoid bone is incised, freeing access to the area of the sella turcica. The pituitary adenoma is excised and removed.
All manipulations are carried out under the control of an endoscope, and an enlarged image is displayed on the monitor, allowing for a wider view of the surgical field. The duration of the operation is 2 – 3 hours. On the first day after surgery, the patient can become more active, and on the fourth day he can be discharged from the hospital in the absence of complications. Complete cure of adenoma with this operation is achieved in almost 95% of cases.
Transcranial (open) surgery is performed in severe cases by craniotomy under general anesthesia. Due to the high traumatic nature of this operation and the high risk of complications, modern neurosurgeons try to resort to it only when it is impossible to perform endoscopic removal of the adenoma, for example, when there is pronounced tumor growth in the brain tissue.
Further forecast
The prognosis for recovery from microadenoma is in most cases positive. This is due to its small size. The compaction usually responds well to various types of treatment and eliminates relapses. If it grows in size, it will be much more difficult to remove.
When diagnosing a small tumor, the doctor may not prescribe intervention or conservative treatment. The patient will only need to monitor changes in its size and regularly come for examination. In some cases, the tumor does not grow during a person’s life, and therefore does not affect its quality.
Radiation therapy
Used for microadenomas with a low level of activity. May be prescribed in combination with drug treatment. Recently, the method of stereotactic radiosurgery of adenoma using Cyber Knife has become widespread - a radioactive beam is supplied directly to the tumor tissue. Gamma therapy also continues to be relevant - radiation from a source outside the body.
Are there complications after surgery?
The risk of complications in the postoperative period varies depending on the surgical technique:
- with transsphenoidal approach, complications develop in 13%, and operative mortality is 3%
- with transcranial access – 27.9% and 7%, respectively.
Complications may develop:
- tumor relapse – develops in 15–16%
- adrenal cortex dysfunction
- vision loss
- thyroid dysfunction
- hypopituitarism – partial or complete failure of the pituitary gland
- speech, memory, attention disorders
- infectious inflammation
- bleeding from the pituitary vessels after surgery
Prevention of complications after surgery is drug correction of hormonal levels in the body based on the results of the examination.
Prevention
It is almost impossible to completely eliminate the risk of developing pathology. However, you can reduce the likelihood using simple methods. It is recommended to normalize the work and rest schedule, try to avoid stressful situations and overwork.
Additionally, it is necessary to balance the diet, include vegetables, fresh fruits, as well as herbs and meat. Patients taking hormonal medications should visit their doctor regularly and also have their blood taken to determine their hormone levels. This will allow deviations to be detected at an early stage.
Women with diseases of the hypothalamus, thyroid gland and adrenal glands should also visit an endocrinologist regularly, because any complication can lead to the formation of microadenoma. When the first signs of a disorder appear, you should immediately visit a doctor.