Gadaeva Madina Lechaevna, ophthalmologist LLC Clinic of Doctor Kurenkov.
Keratoconus is a non-inflammatory disease of the cornea, in which, due to degenerative processes, the cornea becomes thinner and deformed, forming a conical shape. Keratoconus is more common among the male population and mainly begins to manifest itself during puberty. According to statistics, 1 case of the disease occurs in 2000 people, usually among southern peoples.
Keratoconus was first scientifically described in 1748 by the German ophthalmologist Burchard Mauchart. However, a more detailed description of keratoconus was made by the British physician John Nottingham in 1854 and listed the main symptoms: double vision, changes in the shape and strength of the cornea, polyopia, difficulty in choosing glasses. In 1859, British surgeon William Bowman began performing operations on keratoconus to improve vision by tightening the iris through small punctures in the cornea, giving it a slit-like shape like a “cat’s” pupil. Later, the German ophthalmologist Alberta von Graef proposed cauterizing the cornea with a solution of silver nitrate to stabilize its shape, applying after the operation a tight bandage with tissue impregnated with a drug that causes the restoration of corneal cells. For a long time, the only method of trying to slow the progression of keratoconus and somehow improve the vision of patients was the use of a cruel contact lens invented in France in 1888 by the doctor Eugene Kalt.
Causes of keratoconus
The exact causes of the disease are still unknown. The non-inflammatory disease is believed to be caused by genetic factors. There is a lot of evidence that the disease develops due to genetic predisposition.
About 13% of patients who go to the hospital suffer from the pathology due to its presence in other family members. Scientists have found 9 genes that may be associated with the development of keratoconus.
The cause of the disease is too high intraocular pressure and weak layers of the cornea. The earlier this disease is detected, the less complicated the treatment is. However, the pathological condition is often not immediately identified.
There are other diseases/changes with a genetic background in which keratoconus occurs.
Causes:
- neurodermatitis;
- chromosomal abnormalities (trisomy 21).
There is evidence that an imbalance of certain enzymes that play a role in tissue reconstruction leads to partial destruction of the surface layers of the cornea. Free radicals can cause premature apoptosis.
Other theories suggest that keratoconus is caused by infection or weakening of the collagen present in the cornea. But, they have not yet been confirmed and no research has been conducted.
Structure and physiology of the cornea
The cornea is the anterior layer of the eyeball. There are five layers in it. The epithelial and endothelial layers perform the function of protection from the outside and exchange from the inside. They are distinguished by increased strength , and the epithelium, as the most superficial layer, also has excellent regeneration .
The preendothelial layer, or Descemet's membrane , is a barrier to infectious agents. The corneal stroma itself consists of connective tissue cellular structures, between which there is an interstitial substance. This combination makes the cornea especially durable. The composition of the main substance of the thickest layer is collagen . In 2005, the presence of stem cells on the periphery of the superficial membrane was proven. The cornea changes its size due to the growth of collagen fibers and constituent growth cells.
One of the main properties of the cornea is its transparency . This feature of the cornea is due to the unique arrangement of cells - keratocytes, which are arranged in a strict optical order. Transparency also depends on the amount of water in the interstitial substance.
Compliance with all quantitative and qualitative components ensures the correct spherical shape of the cornea and maintenance of normal refractive power.
When there are no disorders or pathologies in all layers of the cornea, then the refractive power of this membrane does not change and, as a result, vision has no pathology. But during the development of the cornea, it is influenced by many factors, both genetic and external. This is how dystrophic diseases appear, which can be congenital or acquired.
Risk group
Descendants and relatives of patients with keratoconus are susceptible to the disease. People at risk include people with Down syndrome, sleep apnea and asthma, black men and Mexicans. People diagnosed with diabetes are less likely to develop a curvature of the cornea. This is confirmed by research conducted by Maria Woodward, during which 16 thousand people were studied.
Children, adolescents and young adults whose parents have been diagnosed with pathology are at particular risk.
Etiology and pathogenesis
The reasons for the development of keratoconus have not yet been fully established; there are many theories suggesting the causes and trigger mechanism for its development.
One of the first to emerge was the endocrine theory. The occurrence of keratoconus was associated with dysfunction of the endocrine glands, accompanied by a violation of the pituitary-diencephalic system, hyper- or hypothyroidism, adipose-genial insufficiency, and a decrease in 17-ketosteroids. It is important to note that the peak progression of keratoconus occurs during the puberty period, when the activation of the endocrine glands occurs during the growth of the body.
There is also a viral theory, proposed due to the observed infection with the hepatitis B virus in patients with keratoconus in 80% of cases.
Exchange theory: in studies of patients with keratoconus, a decrease in the activity of glutathione reductase and glucose-6-phosphate dehydrogenase was found in the anterior chamber fluid. Such enzyme disorders provoke an increase in the level of lipid peroxidation, which in turn activates the release of lysosomal hydrolytic enzymes leading to lysis of intracellular structures.
Allergic theory: Occurs against the background of allergic blepharoconjunctivitis, asthma, hay fever, eczema. This suggests a mechanism caused by a disruption of immune homeostasis by an increase in Ig M, C3, C4 complement components. It was found that as keratoconus progresses, there is an increase in the defectiveness of T-suppressors and an increase in IG, leading to a breakdown in autotolerance to corneal antigens. Moreover, in biopsy samples of the conjunctiva of patients with keratoconus, a high infiltration of lymphocytes, monocytes, macrophages, plasma cells, as well as a significant concentration of mast cells was revealed. Such signs are characteristic of immune inflammation.
Mechanical trauma: With permanent damage to the epithelium, which may be caused by prolonged wearing of contact lenses or constant scratching of the eyelids during allergic reactions. Long-term trauma provokes the launch of the following processes: chronic apoptosis of keratocytes - increase in lysosomal enzymes and proteinase inhibitors - destruction of collagen and, as a consequence, degenerative processes in the corneal epithelium.
The development of secondary keratoconus can also be caused by: inflammatory diseases of the cornea, consequences of injuries and burns, postoperative complications leading to ectasia.
However, the most widespread is the hereditary or genetic theory. Keratoconus is often combined with hereditary syndromes and developmental anomalies, such as Leber amaurosis, Crouzon syndrome, retinal pigmentary degeneration, Down syndrome, Marfan syndrome, granular corneal dystrophy, blue sclera syndrome. It should be emphasized that 68% of patients with keratoconus have one or another connective tissue pathology. Keratoconus also occurs in diseases that are accompanied by mental disorders, such as schizophrenia.
There is an autosomal dominant mode of inheritance of keratoconus and it can occur in members of the same family, transmitted through the male line. In the course of scientific research conducted in the USA, it was possible to determine the gene locus responsible for the occurrence of keratoconus; it is believed that this is the COL6A1 gene with DNA encoding the production of type IV collagen. Research continues.
Classification of keratoconus
There is a division of keratoconus into separate stages. Classification according to Titarenko (1982):
- Stage 1 - optical power 0.5–0.8 diopters. The disease can only be detected with the help of diagnostic devices used in ophthalmological centers. When performing biomicroscopy, the doctor will see a slight rarefaction of the stroma, a change in the shape of endothelial cells and clearly visible nerves.
- Stage 2 - OS 0.3–0.5 diopters. The initial stage of development is characterized by distorted vision of objects, the cornea thins to 0.3 mm. Other signs seen during biomicroscopy include visible lines of keratoconus.
- Stage 3 - OS 0.1–0.2 diopters. The depth of the anterior chamber increases to 4.2 mm. At grade 3, vision continues to deteriorate.
- Stage 4 - OS 0.02–0.08 diopters. The anterior chamber increases to 4.6 mm. At grade 4, the cornea is very thin with opacity of Bowman's membrane.
- Stage 5 - visual acuity is very low. The cornea is noticeably edematous. Stromal opacification and changes in Descemet's membrane are observed. The anterior chamber lengthens to 5 mm or more. The non-inflammatory disease is highly developed; only a cornea transplant will help. She already has scars.
How to avoid developing keratoconus?
Most often, the pathology progresses very slowly. In some cases, its development stops at a certain stage. The later ocular keratoconus appears, the better the prognosis for recovery and the slower the progression of the anomaly.
To minimize the risk of corneal curvature, it is necessary to promptly treat all diseases that can lead to pathology. Also protect your vision from injury and infection. Pay special attention to physical exercise and regularly visit your ophthalmologist for preventive examinations.
Symptoms of keratoconus
Abnormal curvature of the cornea mainly results in distortion and multiple images, resulting in poor vision. At the first stage, the disease manifests itself as a decrease in visual acuity, as with normal refractive error.
As the disease progresses, other signs appear:
- glare;
- poor twilight and night vision;
- distortion of objects;
- blur;
- eye fatigue;
- increased sensitivity to light.
In later stages, additional tissue changes occur that lead to further deterioration of vision. Double images appear and the number of objects increases.
The disease leads to tearing of the membrane on the inside of the cornea. Water penetrates into the cornea, which swells as a result.
The first signs of astigmatism appear at the age of 15–16 years. It is impossible to immediately establish the cause; keratoconus is discovered after several years, when the clinical picture worsens.
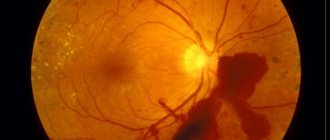
Photo
Possible complications
Defects in visual function in keratoconus significantly reduce a person's quality of life - he sees objects in a distorted form, and straight lines - broken. As the pathological process progresses, the patient faces problems with optical correction of the defect, especially with intolerance to contact lenses. In the last stages of the disease, thinning of the corneal tissue occurs, which threatens its ruptures, which are accompanied by intense pain and require immediate surgical intervention. Without appropriate treatment, keratconus can lead to complete blindness.
Bandage strengthening of the cornea and thermokeratoplasty in the treatment of acute and progressive keratoconus
Diagnosis of keratoconus
The degenerative disease is diagnosed during a routine examination by an ophthalmologist or when myopia appears. Because keratoconus is a relatively rare condition, symptoms may not be detected at the onset.
The reason is that many ophthalmologists only theoretically know about the disease and have not encountered it before. In case of uncertainty, patients should consult another ophthalmologist.
Can be detected by various diagnostic methods:
- topography;
- refractometry;
- computer keratometry;
- pachymetry;
- skiascopy;
- ophthalmometry;
- biomicroscopy.
The initial stage of the disease is difficult to diagnose. It is often confused with myopia and astigmatism. Therefore, when undergoing an examination, it is important to use a variety of diagnostic tools to exclude or confirm degenerative pathology.
Keratoglobus and its manifestations
Disturbance in the distribution of cellular composition across the layers of the cornea changes the properties of each layer. In this case, the corneal stroma suffers the most. It is the thickest corneal structure and rich in cellular composition. Normally, it is quite strong, has no blood vessels and is transparent.
A pathological effect on its development is often exerted by genetic factors, in particular a violation of the synthesis of the fibrillar protein elastin, which is transmitted according to an autosomal recessive type of inheritance. Elastin is responsible for maintaining the shape, strength and regenerative ability of the cornea.
With its pathological production, the stroma loses all the properties described above and becomes easily extensible, which causes a gross change in the shape of the cornea. In most cases, its central sections become convex due to greater extensibility and thinning of the layers. The cornea takes the shape of a ball, becoming like a school globe.
The Greek scientist who first diagnosed this disease in 1907 had no choice but to designate this pathology as keratoglobus.
Clinical manifestations of keratoglobus may appear after the first six months of life. Usually, at the age of 6 months, with this disease, a child can see an unusually large cornea for an infant of the first year of life. But most often keratoglobus is detected at the age of six and older.
Patients with this corneal pathology will complain of decreased vision, double vision, and rapid visual fatigue. Teenagers suffer from headaches that do not have a specific nature and frequency of occurrence. Considering that the primary problem of keratoglobus is visual impairment, such patients in the vast majority of cases will turn to an ophthalmologist.
With keratoglobus, there is almost never any clouding of the cornea.
Among diagnostic measures aimed at timely detection of rare corneal pathologies, the main place is occupied by visometry with correction, biomicroscopy, autorefractometry and tonometry. Fundus examination (ophthalmoscopy) is an additional mandatory method of a comprehensive ophthalmological examination.
Checking visual acuity for keratoglobus reveals low levels and correction, with which certain difficulties arise. The fact is that due to the transformation of the shape of the cornea, its important ability, refractive, is lost. It changes so much that astigmatism, which most often appears with a spherical cornea, does not improve vision. And if a positive correction takes place, then vision improves slightly.
In milder cases, at the initial stages of development, refractive errors in the form of hypermetropia or myopia may be present, but visual acuity, taking into account the correction, also does not bring the expected effect. A visual examination of the eyeball in adolescence does not always reveal a gross change in the shape of the cornea; sometimes it is not even noticeable.
The ophthalmologist should be especially wary if a similar disease has already been encountered in the family history, and the patient has signs of low vision that is difficult to correct.
In children of the first year of life, there is a need for tonometry and measurement of intraocular pressure. This study allows us to exclude congenital glaucoma, since macrocornea is a sign of buphthalmos. If there are problems with correction, ophthalmologists perform autorefractometry with the keratometry function. The data from this examination reveal serious changes in the size of the cornea and refractive data (high myopia, the presence of complex astigmatism).
Biomicroscopy, which is an integral part of the ophthalmological examination, does not reveal any signs of dystrophic degeneration of the cornea, which is one of the diagnostic signs of keratoglobus. Ophthalmoscopy also reveals no pathological abnormalities in the fundus.
If there is a suspicion of the presence of a pathology in the shape of the cornea, the patient must be referred for an additional study - keratotopography, after which the final diagnosis will not raise doubts.
Treatment of keratoconus
Contact lenses
In the early stages of the disease, much can be achieved with the help of special shape-resistant lenses or a combination of contact lenses and glasses. Soft CLs are suitable only when keratoconus is in the first stage of development.
Hard contact lenses will help correct refractive error at stage 2 of the disease. They compensate for surface unevenness with their shape. LCDs should be selected according to the curvature of the cornea so that the products do not fall out.
Hard contact lenses are perceived by the sensitive surface of the cornea as a foreign body. To minimize this, you need to choose the right optics.
LCDs can correct curvature, but they do not correct visual impairment. Lenses will not prevent further development of the disease. The patient will require surgery in the future.
Radial keratotomy
This is another procedure that is used to try to stop the disease. An incision about 7 mm wide is made around the optical axis of the cornea. The incision is then closed with a double suture. Thus, the cornea is tightened and the cone is restored.
The cornea in the area of the incision must be at least 400 µm thick and sufficiently stable.
Corneal collagen cross-linking
This is a relatively new treatment method. It has been studied for the last 10 years. Collagen cross-linking is a procedure that aims to slow, but not completely stop, the progression of the degenerative process.
The method consists in producing additional chemical cross-links between the molecules of the corneal connective tissue (stroma), which makes the tissue more rigid and less deformable.
Indeed, cross-linkage in collagen connective tissue increases with age. This is also the reason why keratoconus progresses less severely in older patients.
Intraradicular ring segments
These are small plexiglass clips in the shape of a semicircle. They reshape the cornea in a way that reduces nearsightedness and bulge.
The procedure is suitable for patients whose vision cannot be compensated by glasses or contact lenses and who do not have sufficient severity of the degenerative process to undergo a transplant.
By installing intraradicular ring segments, it is not possible to restore full visual acuity. Patients will still have to wear glasses.
Cornea transplant
For progressive disease, transplantation is the only alternative procedure. Since there are no inflammatory changes in the pathology, the chances of success are high.
At stage 3, keratoplasty is performed. Only the top layers are replaced with donor material.
Stage 4 requires perforated keratoplasty, which replaces the entire cornea. The laser technology used during the operation ensures high precision and rapid healing.
Transplantation is performed on an outpatient or inpatient basis, often under general anesthesia. The threads are removed only after a few months, since the cornea grows very slowly. In order to prevent rejection of the new membrane, the patient is prescribed medications (drops containing cortisone). Typically, the medications are taken over the next 6 months.
In 90% of cases, surgical intervention ends well and allows one to achieve visual acuity close to one hundred percent.
Recently, crosslinking has been used. This is an innovative way to treat keratoconus; the procedure lasts 40 minutes. After cross-linking, the patient recovers quickly, the rehabilitation period is short.
Postoperative period
After transplantation, it is necessary not to perform physical activity for the next 5 days. The patient should be at rest.
If endothelial layer-by-layer transplantation was performed, the patient must remain in bed for 24 hours after surgery. You should lie on your back, without standing up or turning over on your stomach or side. This will help ensure the correct position of the graft.
In the postoperative period, medications should be taken to speed up tissue healing. Antibiotics may be prescribed to prevent infection from developing.
Anti-inflammatory drugs are prescribed to relieve inflammation. They are taken orally and used in the form of drops.
Applications of femtosecond laser
It allows you to model a thin flap of the cornea with precise control of alignment, diameter and thickness. The device sends pulses to adjacent areas of the shell, causing the bubbles to merge. Then the surgeon begins laser correction.
This technique preserves the integrity of the structure of the cornea. After surgery, even in poor lighting conditions, vision remains high.
This method reduces rehabilitation time. The procedure is painless and is carried out in a medical facility.
Drug therapy
Medicines are used to saturate the cornea with nutrients and strengthening components. Courses of vitamin therapy, tissue treatment, immunomodulators and antioxidants are prescribed.
The following drugs are prescribed:
- Taurine;
- Taufon;
- Solcoseryl.
Quinax, Korneregel, Balarpan are used at the same time. Drops, gels and eye ointments slow the progression of the disease. With their help, it is possible to restore metabolic processes in the optical system and improve visual acuity.
These treatment methods are used at any stage of the disease. Can be used after eye surgery as directed by doctors.
Some medications prevent further thinning of the cornea.
Modern diagnostics at NEARMEDIC
Diagnosing keratoconus is not easy. If the doctor does not have modern equipment, then when the patient complains of decreased vision, he is mistakenly diagnosed with myopia. This is exactly what happens in most public clinics, where people with similar complaints first turn. First, a person is offered correction with glasses or lenses, which improves vision. But quite quickly it falls again and in this regard, laser or surgical methods for correcting myopia are recommended. But such intervention further aggravates the problem, and the disease keratoconus begins to progress at a rapid pace.
The main method that detects corneal keratoconus at the initial stage is a biomicroscopic examination. This is an intravital assessment of the condition of the tissues of the eyeball under magnification. The main signs that indicate this disease are thinning of the cornea, a defined conical protrusion and cracks in the adjacent membrane. A specific feature is the Fleischer ring, characteristic of late stages, in which hemosiderin is deposited along the edge of the protrusion.
Other methods that are prescribed for suspected keratoconus are primarily aimed at excluding diseases with identical symptoms. Your doctor may recommend:
- Refractometry – measurement of the degree of refraction in the eye;
- Ophthalmoscopy – inspection is possible only through transparent areas of the cornea;
- Ultrasound scanning of the eye;
- Keratopachymetry – measurement of the thickness of the cornea (its thinning is revealed);
- Optical tomography of the eye.
Forecast
The later the disease develops, the more favorable the prognosis. With timely contact with an ophthalmologist, the functioning of the affected eye is successfully restored.
In the later stages of the disease, conservative methods may not help, so they resort to surgical intervention. But even with this method of treatment, doctors manage to achieve an increase in visual acuity.
The prognosis after transplant surgery is positive in most cases. Transparency is restored and visual acuity is improved.
Modern diagnostics at NEARMEDIC
Diagnosing keratoconus is not easy. If the doctor does not have modern equipment, then when the patient complains of decreased vision, he is mistakenly diagnosed with myopia. This is exactly what happens in most public clinics, where people with similar complaints first turn. First, a person is offered correction with glasses or lenses, which improves vision. But quite quickly it falls again and in this regard, laser or surgical methods for correcting myopia are recommended. But such intervention further aggravates the problem, and the disease keratoconus begins to progress at a rapid pace.
The main method that detects corneal keratoconus at the initial stage is a biomicroscopic examination. This is an intravital assessment of the condition of the tissues of the eyeball under magnification. The main signs that indicate this disease are thinning of the cornea, a defined conical protrusion and cracks in the adjacent membrane. A specific feature is the Fleischer ring, characteristic of late stages, in which hemosiderin is deposited along the edge of the protrusion.
Other methods that are prescribed for suspected keratoconus are primarily aimed at excluding diseases with identical symptoms. Your doctor may recommend:
- Refractometry – measurement of the degree of refraction in the eye;
- Ophthalmoscopy – inspection is possible only through transparent areas of the cornea;
- Ultrasound scanning of the eye;
- Keratopachymetry – measurement of the thickness of the cornea (its thinning is revealed);
- Optical tomography of the eye.
Prevention
According to all modern research and findings, it is currently impossible to prevent the disease. However, there are preventive measures that are important to follow for people at risk:
- avoid long stays in dusty and smoky rooms;
- use moisturizing drops when working with a PC;
- spend more time outdoors and drink more fluids;
- wear sunglasses;
- promptly contact medical institutions if a foreign body gets into your eyes;
- treat illnesses according to doctor’s recommendations;
- Do not self-medicate ophthalmological problems, including dry eye syndrome.
Clinical picture
The common and most common clinical signs of keratoconus include:
- progressive decrease in vision;
- increased fatigue of the visual organs;
- itching and burning sensation on the mucous membranes of the eyeball;
- tearfulness, especially in bright light;
- deformation and clouding of the corneal layer when examined by an ophthalmologist;
- double vision;
- decreased concentration;
- distortion of objects in the field of view;
- the need to frequently change glasses and contact lenses;
- decreased performance associated with impaired vision;
- in rare cases, complete blindness.
Relationship between astigmatism and keratoconus
As can be seen from the above classification of the disease, the early stages of disease progression are accompanied by astigmatism, which is expressed in the corresponding symptoms:
- blurriness and unclearness of the picture that the patient sees;
- discomfort in the eyes, pain, itching and burning, especially in the evening; inability to focus on small objects; headaches, in most cases concentrated in the frontal lobe;
- increased eye fatigue, especially when reading;
- inability to see distant or close objects in detail.
If these clinical signs are initially recognized as astigmatism, the disease subsequently develops and the patient’s condition worsens. The present symptoms allow the ophthalmologist to suspect the presence of keratoconus, especially if the condition rapidly worsens.
How the disease develops
Initially, keratoconus typically affects only one eye. Over time, in the absence of adequate treatment, the pathological process affects both eyes. In this case, the degree of damage to the left and right eyes may differ (one eye sees better than the other), which is associated with alternating damage (initially one, after a while the other).
The early stage of the disease is characterized by a slight decrease in vision, especially blurred vision in the evening, when in poorly lit rooms. As the disease progresses, photophobia may occur, and clouding of the cornea leads to blurred vision and double vision.
Many patients develop monocular polyopia - when looking at two objects, they are perceived as one. Diagnosis of monocular polyopia includes:
- the ophthalmologist places in front of the patient a sheet of black paper with one white spot on it;
- in this case, the patient sees several randomly located spots on a black background;
- voicing the correct answer by the doctor and showing the picture over time does not change the results; in the future, if the disease develops, in the same picture the patient sees even more white spots, randomly located; in the later stages of the progression of the pathology, these spots pulsate in time with the heartbeat.
A special sign of disease progression is that the patient wears perfectly fitted glasses; after 10-15 days they will no longer fit him. In the case of standard lenses, as the disease progresses, wearing them becomes impossible. This is due to deformation of the corneal layer, as a result of which the lens cannot fit completely. Each of these signs indicates with 100% probability the occurrence and worsening of keratoconus.
Other symptoms
Among other clinical signs, the most common are unpleasant and painful sensations in the eyes, increased fatigue, and tearfulness. Such symptoms are manifested by deterioration of vision, as a result of which the patient has to squint and often instinctively rub his eyes.
The same reasons cause the occurrence of headaches, which are associated with a decrease in attention, performance, and ability to concentrate on something. In patients with keratoconus, rapid deterioration of vision is often replaced by long-term stagnation in the development of the disease.
Each of the symptoms described, with the exception of the last, is dangerous for humans. People who need to concentrate on dangerous work or while driving are especially at risk.
Clinic of acute keratoconus
Acute keratoconus is a special type of disease that develops in case of neglect of doctor’s recommendations or errors in treatment. Its occurrence is characterized by clinical signs:
- hyperemia of the mucous membranes of the eye;
- severe swelling of the corneal layer;
- sudden clouding of the cornea or sudden blindness;
- rapid deterioration of visual acuity;
- the occurrence of intense pain.
This condition is dangerous; it is accompanied by rapid deformation and other pathological changes in the corneal layer. Adjustment of treatment and unquestioning adherence to the doctor’s recommendations helps stabilize the patient after 1-2 weeks and improves the functions of the visual organ. If acute keratoconus occurs in the later stages of the pathological process, this is fraught with a violation of the integrity of the corneal layer or blindness.
Symptoms in children
In most cases, the pathological process develops from childhood. You can recognize the disease by looking closely at the child’s behavior:
- school performance deteriorates, the child is distracted and inattentive;
- when reading, the child brings the book closer to his eyes than usual;
- the child begins to squint;
- eyes water and turn red for no apparent reason;
- children systematically complain of headaches;
- in later stages, children report blurriness of the image.
If a child has previously been seen by an ophthalmologist and, according to the doctor’s indications, wears glasses, they quickly become unusable, as evidenced by the corresponding complaints. Changing glasses is accompanied by a short-term improvement and no complaints. But after a couple of weeks, the blurriness of the image and other complaints return again. The lack of timely and correct treatment threatens swelling of the corneal layer and complete blindness.