Pulmonary sarcoidosis is a systemic and benign accumulation of inflammatory cells (lymphocytes and phagocytes), with the formation of granulomas (nodules), with an unknown cause.
Mostly the age group 20–45 years old is affected, the majority are women. The frequency and magnitude of this disorder is within the range of 40 diagnosed cases per 100,000 (according to EU data). The lowest prevalence is in East Asia, with the exception of India, where the rate of patients with this disorder is 65 per 100,000. It is less common in childhood and in the elderly.
Pathogenic granulomas are most common in the lungs of certain ethnic groups, such as African Americans, Irish, Germans, Asians, and Puerto Ricans. In Russia, the prevalence rate is 3 per 100,000 people.
Reasons for development
Oddly enough, the true causes of pulmonary sarcoidosis are still unknown. Some scientists believe the disease is genetic, others that pulmonary sarcoidosis occurs due to impaired functioning of the human immune system. There are also suggestions that the cause of the development of pulmonary sarcoidosis is a biochemical disorder in the body. But at the moment, most scientists are of the opinion that the combination of the above factors is the cause of the development of pulmonary sarcoidosis, although not a single theory put forward confirms the nature of the origin of the disease.
Scientists studying infectious diseases suggest that protozoa, Histoplasma, spirochetes, fungi, mycobacteria and other microorganisms are the causative agents of pulmonary sarcoidosis. Endogenous and exogenous factors can also cause the development of the disease. Thus, today it is generally accepted that pulmonary sarcoidosis of polyetiological origin is associated with a biochemical, morphological, immune disorder and genetic aspect.
The incidence is observed in persons of certain professions: firefighters (due to increased toxic or infectious exposure), mechanics, sailors, millers, agricultural workers, postal workers, chemical industry and healthcare workers. Pulmonary sarcoidosis is also observed in people with tobacco addiction. The presence of an allergic reaction to certain substances perceived by the body as foreign due to impaired immunoreactivity does not exclude the development of pulmonary sarcoidosis.
A cascade of cytokines is responsible for the formation of sarcoid granuloma. They can form in various organs and also consist of a large number of T lymphocytes.
Several decades ago, there was an assumption that pulmonary sarcoidosis was a form of tuberculosis that was caused by weakened mycobacteria. However, according to the latest data, it has been established that these are different diseases.
Necessary preventive measures
It is recommended to lead a healthy lifestyle and not smoke.
Consume products with non-natural ingredients as little as possible. Limit the use of chemicals. The likelihood of developing sarcoidosis occurs in those patients who have pathologies in the functioning of the immune system.
If there are minor suspicions, they should seek advice from a specialist and take care of their health.
Those who are already sick should take care of their health and not allow the disease to worsen. They need to limit their calcium intake. Sarcoidosis leads to the formation of bladder stones, and calcium accelerates this process. Exposure to the sun is limited.
Vitamin D, which is produced by exposure to sunlight, helps produce calcium. It is necessary to reduce exposure to harmful chemicals and increase the body's immune reactivity.
If you suffer from shortness of breath and persistent cough, you need to consult a specialist and check your health.
The examination is necessary for people:
- If the rash on the body does not go away,
- With weight loss,
- If fatigue occurs quickly,
- Body temperature rises.
Those who have already been diagnosed with this disease need to be under the supervision of a doctor at all times.
Classification
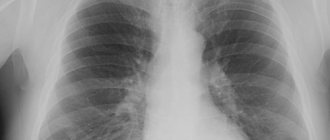
Based on the obtained radiological data, three stages and corresponding forms are distinguished during pulmonary sarcoidosis.
- Stage I (corresponds to the initial intrathoracic lymphoglandular form of sarcoidosis) – bilateral, often asymmetrical enlargement of bronchopulmonary, less often tracheobronchial, bifurcation and paratracheal lymph nodes.
- Stage II (corresponds to the mediastinal-pulmonary form of sarcoidosis) - bilateral dissemination (miliary, focal), infiltration of the lung tissue and damage to the intrathoracic lymph nodes.
- Stage III (corresponds to the pulmonary form of sarcoidosis) – severe pneumosclerosis (fibrosis) of the lung tissue, no enlargement of intrathoracic lymph nodes. As the process progresses, confluent conglomerates form against the background of increasing pneumosclerosis and emphysema.
According to the clinical and radiological forms and localization encountered, sarcoidosis is distinguished:
- Intrathoracic lymph nodes (HTNL)
- Lungs and VGLU
- Lymph nodes
- Lungs
- Respiratory system, combined with damage to other organs
- Generalized with multiple organ lesions
During pulmonary sarcoidosis, there is an active phase (or exacerbation phase), a stabilization phase and a phase of reverse development (regression, attenuation of the process). Reverse development can be characterized by resorption, thickening and, less commonly, calcification of sarcoid granulomas in the lung tissue and lymph nodes.
According to the rate of increase in changes, the development of sarcoidosis can be abortive, slow, progressive or chronic. Consequences of the outcome of pulmonary sarcoidosis after stabilization of the process or cure may include: pneumosclerosis, diffuse or bullous emphysema, adhesive pleurisy, hilar fibrosis with calcification or absence of calcification of the intrathoracic lymph nodes.
Drug treatment
Indications for emergency treatment are severe, rapid development of the disease, its generalized or combined form, obvious dissemination in the lung tissue, tumor-like lesions of the thoracic lymph nodes.
The disease is treated with long courses of Prednisolone, Indomethacin, Rezokhin and tocopherol acetate.
The combined regimen involves a course of Prednisolone, Dexamethosone and Polcortolone, alternating with the use of non-steroidal anti-inflammatory drugs Voltaren and Indomethacin.
On average, the course of treatment is 3-4 months, followed by a reduction in dosage over 6-12 months. At stages 1-2 of damage to the respiratory system, inhaled glucocorticosteroids may be used.
The patient is observed at a dispensary in the phthisiology department.
All patients are divided into two therapeutic groups:
- I - with an active stage: Ia - diagnosis established for the first time;
- Ib - relapse and/or exacerbation after main treatment;
- II - inactive sarcoidosis.
You must be registered with a dispensary for at least 24 months, in case of severe disease - up to 5 years. After complete recovery, the patient is removed from the register.
Symptoms and first signs
The development of pulmonary sarcoidosis is characterized by the appearance of nonspecific symptoms. These include in particular:
- Malaise;
- Anxiety;
- Fatigue;
- General weakness;
- Weight loss;
- Loss of appetite;
- Fever;
- Sleep disorders;
- Night sweats.
The intrathoracic (lymphoglandular) form of the disease is characterized by the absence of any symptoms for half of the patients. Meanwhile, the other half tend to identify symptoms of the following type:
- Weakness;
- Painful sensations in the chest area;
- Joint pain;
- Dyspnea;
- Wheezing;
- Cough;
- Temperature increase;
- The appearance of erythema nodosum (inflammation of subcutaneous fat and blood vessels of the skin);
- Percussion (examination of the lungs in the form of tapping) determines the increase in the roots of the lungs bilaterally.
As for the course of such a form of sarcoidosis as the mediastral-pulmonary form, it is characterized by the following symptoms:
- Cough;
- Dyspnea;
- Pain in the chest area;
- Auscultation (listening to characteristic sound phenomena in the affected area) determines the presence of crepitus (characteristic “crunching” sound), scattered dry and moist rales.
- The presence of extrapulmonary manifestations of the disease in the form of damage to the eyes, skin, lymph nodes, bones (in the form of the Morozov-Junling symptom), damage to the salivary parotid glands (in the form of the Herford symptom).
Complications
The most common consequences of this disease include the development of respiratory failure, cor pulmonale, emphysema (increased airiness of the lung tissue), and broncho-obstructive syndrome.
Due to the formation of granulomas in sarcoidosis, pathology is observed in the organs on which they appear (if the granuloma affects the parathyroid glands, calcium metabolism is disrupted in the body, hyperparathyroidism is formed, from which patients die). Against the background of weakened immunity, other infectious diseases (tuberculosis) may occur.
Diagnostics
Without an accurate analysis, it is impossible to clearly classify the disease as sarcoidosis.
Many signs make this disease similar to tuberculosis, so careful diagnosis is necessary to establish a diagnosis.
- Survey - decreased ability to work, lethargy, weakness, dry cough, chest discomfort, joint pain, blurred vision, shortness of breath;
- Auscultation - hard breathing, dry wheezing. Arrhythmia;
- Blood test - increased ESR, leukopenia, lymphopenia, hypercalcemia;
- X-ray and CT scan - the “ground glass” symptom, pulmonary dissemination syndrome, fibrosis, compaction of lung tissue are determined;
Other devices are also used. An effective bronchoscope is one that looks like a thin, flexible tube that is inserted into the lungs to examine and take tissue samples. Under certain circumstances, a biopsy may be used to analyze tissue at the cellular level. The procedure is carried out under the influence of an anesthetic, so it is practically invisible to the patient. A thin needle plucks off a piece of inflamed tissue for subsequent diagnosis.
Clinical manifestations
A feature of the disease is the absence of specific signs that would clearly indicate it. Sarcoidosis can be asymptomatic for a long time and discovered by chance when visiting a doctor for another reason. Sometimes it is disguised as other diseases, so in outpatient settings the number of misdiagnoses in these patients reaches 30%. In the advanced stage of the disease, symptoms of lung damage are combined with general manifestations and signs of involvement of other organs.
How to treat pulmonary sarcoidosis
The treatment of pulmonary sarcoidosis is based on the use of hormonal drugs, corticosteroids. Their action in this disease is as follows:
- weakening of the perverted reaction from the immune system;
- preventing the development of new granulomas;
- anti-shock effect.
There is still no consensus regarding the use of corticosteroids for pulmonary sarcoidosis:
- when to start treatment;
- how long to carry out therapy;
- what should be the initial and maintenance doses.
A more or less established medical opinion regarding the prescription of corticosteroids for pulmonary sarcoidosis is that hormonal drugs can be prescribed if radiological signs of sarcoidosis do not disappear within 3-6 months (regardless of clinical manifestations). Such waiting periods are maintained because in some cases the disease may regress (reverse development) without any medical prescriptions. Therefore, based on the condition of a particular patient, we can limit ourselves to medical examination (registering the patient) and monitoring the condition of the lungs.
In most cases, treatment begins with prednisolone. Next, inhaled and intravenous corticosteroids are combined. Treatment is long-term - for example, inhaled corticosteroids can be prescribed for up to 15 months. There have been cases when inhaled corticosteroids were effective in stages 1-3 even without intravenous corticosteroids - both the clinical manifestations of the disease and pathological changes on X-ray images disappeared.
Since sarcoidosis affects other organs in addition to the lungs, this fact must also be taken into account when making medical prescriptions.
In addition to hormonal drugs, other treatments are prescribed:
- broad-spectrum antibiotics - for prevention and in case of an immediate threat of developing secondary pneumonia due to infection;
- if the viral nature of secondary lung damage in sarcoidosis is confirmed, antiviral drugs are used;
- with the development of congestion in the circulatory system of the lungs, drugs that reduce pulmonary hypertension (diuretics, etc.);
- restoratives - first of all, vitamin complexes that improve the metabolism of lung tissue and help normalize immunological reactions characteristic of sarcoidosis;
- oxygen therapy for the development of respiratory failure.
It is recommended not to eat foods rich in calcium (milk, cottage cheese) and not to sunbathe. These recommendations are due to the fact that with sarcoidosis the amount of calcium in the blood may increase. At a certain level, there is a risk of the formation of calculi (stones) in the kidneys, bladder and gall bladder.
Since pulmonary sarcoidosis is often combined with the same damage to other internal organs, consultation and appointments of related specialists are necessary.
The role of medications
There is a connection between the development of granulomatous inflammation and the use of medications that affect the immune system:
- Interferon-alpha;
- Antineoplastic agents;
- Hyaluronic acid.
Often the disease develops spontaneously, and a probable cause cannot be determined.
Under the influence of provoking factors (antigens), predisposed people develop a special type of immune response. Lymphocytic alveolitis, granulomas, and vasculitis develop. Late stages of the disease are characterized by the presence of pulmonary fibrosis - replacement of the affected areas with connective tissue.
Prevention of disease complications
Prevention of complications of the disease involves limiting contact with factors that could cause sarcoidosis. First of all, we are talking about environmental factors that can enter the body with inhaled air. Patients are advised to regularly ventilate the apartment and do wet cleaning to avoid air dust and mold formation. In addition, it is recommended to avoid prolonged sunbathing and stress, as they lead to disruption of metabolic processes in the body and intensification of the growth of granulomas.
Preventive measures also include avoiding hypothermia, as this can contribute to the addition of a bacterial infection. This is due to deterioration of lung ventilation and weakened immunity in general. If there is already a chronic infection in the body, then after sarcoidosis is confirmed, it is necessary to visit a doctor to find out how to control the infection most effectively.
Sources
- Diagnosis and treatment of sarcoidosis (Federal consensus clinical guidelines) / Chuchalin A.G., Avdeev S.N., Baranova O.P., Borisov S.E. – 2014.
- Sarcoidosis / Michael C. Iannuzzi , Birendra P. _ Sah – 2021.
- Sarcoidosis //Russian Medical Journal /Babanov S.A. – 2013.
- Sarcoidosis in the practice of a rheumatologist // Russian Medical Journal / Sedyshev S.Kh., Vasiliev V.I. – 2003.
Folk recipes
Reviews from patients indicate their benefits only at the very beginning of the disease. Simple recipes made from propolis, oil, ginseng/rhodiola are popular. How to treat sarcoidosis with folk remedies:
- Take 20 g of propolis in half a glass of vodka and leave in a dark glass bottle for 2 weeks. Drink 15-20 drops of tincture in half a glass of warm water three times a day 1 hour before meals.
- Take 1 tbsp before meals three times a day. a spoonful of sunflower oil (unrefined) mixed with 1 tbsp. spoon of vodka. Conduct three 10-day courses, taking breaks of 5 days, then repeat.
- Drink 20-25 drops of tincture of ginseng or Rhodiola rosea every morning and afternoon for 15-20 days.
Nutrition
You should exclude fatty fish, dairy products, and cheeses, which increase the inflammatory process and provoke the formation of kidney stones. It is necessary to forget alcohol, limit the consumption of flour products, sugar, and salt. A diet with a predominance of protein dishes in boiled and stewed form is required. Nutrition for pulmonary sarcoidosis should be frequent, small portions. It is advisable to include in the menu:
- legumes;
- seaweed;
- nuts;
- honey;
- black currant;
- sea buckthorn;
- grenades.
Prevalence of the disease
Pulmonary sarcoidosis occurs at any age. Men and women from 20 to 35 years old get sick equally often; after 40 years, the disease affects mainly women. Cases of sarcoidosis are reported everywhere, but its geographical prevalence varies:
- European countries 40 per 100 thousand population;
- New Zealand 90 per 100 thousand;
- Japan only 0.3 per 100 thousand;
- Russia 47 per 100 thousand.
Sarcoidosis is a fairly rare disease, so people who are diagnosed with it usually do not know what it is.